General Information about Warfarin
It is crucial to take warfarin as directed by a physician and to comply with all directions carefully. Taking an excessive amount of warfarin may cause bleeding, while taking too little can improve the danger of clots forming. Patients on warfarin should also be cautious when taking different medicines, as some can interact with warfarin and affect its effectiveness or increase its unwanted facet effects.
In conclusion, warfarin plays an necessary role in treating and stopping dangerous clots in the body. It has been a lifesaving medication for so much of patients, and when taken as directed and carefully monitored, it can effectively scale back the risk of great well being problems. However, it is essential to understand the potential risks and limitations of warfarin and to comply with all instructions and precautions offered by a healthcare skilled.
In some instances, warfarin can also work together with different medicines and dietary supplements, together with over-the-counter medication and natural cures. Therefore, it is essential to tell your physician and pharmacist about all of the drugs you are taking before starting warfarin.
Warfarin, also known by its brand name Coumadin, is a generally prescribed medicine for treating and preventing harmful clots in the physique. It is categorized as an anticoagulant, which implies it helps skinny the blood and prevent the formation of clots. Warfarin has been in use because the 1950s and has saved numerous lives. Let's take a more in-depth take a glance at this broadly used medication.
While warfarin is highly effective in stopping harmful clots, it does have some drawbacks. One of the primary disadvantages is the need for frequent blood exams and dosage changes, which may be inconvenient for some sufferers. Additionally, sure foods and drinks, like leafy green vegetables and alcohol, also can affect warfarin levels and may have to be limited.
Another potential danger of warfarin is the potential for bleeding, as it thins the blood and makes it tougher for the body to form clots. It is important for anybody taking warfarin to report any signs of bleeding, such as uncommon bruising or bleeding from the gums, to their physician immediately.
Warfarin is usually taken orally in the form of a pill, and the dosage is rigorously monitored by a well being care provider. When beginning warfarin, patients will normally have their blood examined regularly to discover out the right dosage and make positive that their blood just isn't too thin or too thick. The best range for warfarin levels is called the International Normalized Ratio (INR), and sometimes ranges between 2.0 and 3.0 for most patients. Regular blood checks help doctors adjust the dosage as wanted to keep the INR inside this range.
One of the main advantages of warfarin is its ability to prevent dangerous clots from forming. Clots may be dangerous in the event that they kind in the incorrect place, similar to inside an artery or vein. Arterial clots can result in circumstances like a coronary heart attack or stroke, whereas venous clots can cause DVT or PE. In these cases, warfarin can be a lifesaving medication.
Warfarin works by interfering with the body's manufacturing of vitamin K, an important nutrient for blood clotting. By blocking the action of vitamin K, warfarin reduces the physique's capability to kind clots. It is primarily utilized in patients who have a better risk of developing clots, similar to those who have a history of situations like deep vein thrombosis (DVT), pulmonary embolism (PE), atrial fibrillation, or have undergone heart valve substitute surgical procedure.
The adrenal medulla is populated by the neural crest cells originating from the neural ectoderm hypertension first line treatment buy warfarin toronto. The consequence of this migration is evident by the existence of paragangliomas (extra-adrenal pheochromocytomas) all along the paraspinal axis. The adrenal glands are located in the retroperitoneum superior to the kidney and lateral to the vena cava (on the right) and aorta (on the left). This relationship is important in determining the vascular supply to the adrenals. Each adrenal is supplied by three arteries: Superior adrenal artery (arises from the inferior phrenic artery), middle adrenal artery (branch of the aorta), and inferior adrenal artery (branch of the renal artery). The adrenal gland is histologically composed of four layers, each with their own biosynthetic products. Zona glomerulosa is responsible for mineralocorticoid production, of which aldosterone is the primary product. Aldosterone acts to increase circulating blood volume by increasing sodium and chloride reabsorption in the distal tubule of the kidney. Zona fasciculata produces the glucocorticoids of the adrenal glands, of which cortisol is the primary product. Glucocorticoids have extremely broad effects with the overall goal of inducing a catabolic state in the body in response to stress. Glucocorticoids increase blood glucose concentrations, stimulate lipolysis, enhance adrenergic stimulation of the cardiovascular system, and reduce the inflammatory response of the immune system. The adrenal medulla produces the catecholamines norepinephrine (noradrenaline) and epinephrine (adrenaline) that act on peripheral and -adrenergic receptors. Simulation of the myocardium via 1 receptors increases heart rate and contractility. Patients presenting with an adrenal mass should undergo a complete biochemical workup including (Endocr Pract. Overnight dexamethasone suppression test with measurement of plasma cortisol to evaluate for a cortisol secreting mass. Basic metabolic panel with measurement of serum potassium in hypertensive patients to evaluate for an aldosterone secreting mass. The clinical manifestations of Cushing syndrome include hypertension, edema, muscle weakness, glucose intolerance, osteoporosis, easy bruising, cutaneous striae, and truncal obesity (buffalo hump, moon facies). Women may develop acne, hirsutism, and amenorrhea as a result of adrenal androgen excess. Abnormal secretion of cortisol from a primary adrenal adenoma or carcinoma is the cause of hypercortisolism in 10% to 20% of cases. Establishing the presence of hypercortisolism: (1) the best screening test for hypercortisolism is a 24-hour measurement of the urinary excretion of free cortisol. Urinary excretion of more than 100 µg/day of free cortisol in two independent collections is virtually diagnostic of Cushing syndrome. Measurement of random plasma cortisol levels alone is not a reliable method of diagnosing Cushing syndrome due to overlap of the levels in normal and abnormal patients. Patients with true hypercortisolism have lost normal adrenalÑpituitary feedback and usually fail to suppress the morning plasma cortisol level to less than 5 µg/dL. Imaging tests are useful for identifying lesions suspected on the basis of biochemical testing. Surgical treatment of Cushing syndrome involves removing the cause of cortisol excess. Primary adrenal causes of Cushing syndrome are treated by removal of the adrenal gland containing the tumor. All patients who undergo adrenalectomy for primary adrenal causes of Cushing syndrome require perioperative and postoperative glucocorticoid replacement because the pituitaryÑadrenal axis is suppressed. Recovery of the pituitaryÑadrenal axis may take as long as 6 to 18 months following unilateral adrenalectomy. Primary hyperaldosteronism is a syndrome of hypertension and hypokalemia caused by hypersecretion of the mineralocorticoid aldosterone. Secondary aldosteronism is a physiologic response of the reninÑangiotensin system to renal artery stenosis, cirrhosis, congestive heart failure, and normal pregnancy. Adrenocortical carcinoma and autosomal dominant glucocorticoid-suppressible aldosteronism are rare causes of primary aldosteronism. Given the prevalence of essential hypertension, it is not cost-effective to screen all adults with hypertension for primary hyperaldosteronism. Adults who should be evaluated include those with new onset severe hypertension at a young age and those whose blood pressure is labile or poorly controlled on three or more antihypertensives. Laboratory diagnosis of primary aldosteronism begins with the demonstration of hypokalemia (<3. The patient should be treated with spironolactone (200 to 400 mg/day) preoperatively for 2 to 3 weeks to control blood pressure and to correct hypokalemia. A potassium-sparing diuretic, such as amiloride (5 to 20 mg/day), and calcium channel blockers have also been used. The clinical manifestations of pheochromocytoma include paroxysms of pounding frontal headache, diaphoresis, palpitations, flushing, or anxiety related to the excess sympathetic stimulation from catecholamines. The most common sign is episodic or sustained hypertension, but pheochromocytoma accounts for only 0. Uncommonly, patients present with complications of prolonged uncontrolled hypertension. Pheochromocytomas are neoplasms derived from the chromaffin cells of the sympathoadrenal system that engage in unregulated, episodic oversecretion of catecholamines.
Cases are referred mostly from doctors blood pressure chart for women order warfarin 5 mg on line, but also from registrars of births and deaths and from other sources. Right ventricular hypertrophy secondary to increased pulmonary vascular resistance due to chronic lung disease. Synthetic mineralocorticoids include fludrocortisone, used for replacement therapy and in congenital adrenal hyperplasia and postural hypotension. Use in severe sepsis remains controversial and is usually reserved for patients with confirmed adrenocortical insufficiency and/or high vasopressor requirements. Prednisolone 5 mg has equivalent anti-inflammatory activity to 20 mg hydrocortisone, 4 mg methylprednisolone and 0. All except hydrocortisone have little mineralocorticoid activity and are thus suitable for long-term disease suppression. The drugs have many side effects: related to mineralocorticoid activity: water and sodium retention, hypokalaemia, hypertension. Pituitaryadrenal axis function may take 6 months to recover following withdrawal of therapy; during this time patients are unable to mount a normal cortisone response to stress (secretion increases from 25 mg/day to 300 mg/day), and may develop circulatory collapse. Patients at risk are those who have: - received corticosteroid therapy for longer than 2 weeks within the previous 2 months (up to 1 year has been suggested). Based on studies of normal cortisone responses following surgery, estimated amounts required are 25 mg hydrocortisone equivalent for minor surgery; 5075 mg/day for 12 days for moderate surgery; and 100150 mg/day for 23 days for major surgery. These estimates include current medication; thus patients already taking the required amount do not need supplementation. Anaesthetic implications include concerns about the environmental safety of anaesthetists, scavenging and contamination of anaesthetic equipment. Intraoperative anaesthetic cost constitutes about 56% of total hospital costs, whereas the total cost for intraoperative patient care is approximately 30%. Estimates of the total costs of individual procedures have been made but vary widely according to the country and hospital, and the methods used for the calculations. In addition, techniques or drugs which appear more expensive may have cost savings elsewhere. However, it has been estimated that about half the intraoperative anaesthetic costs could be influenced by the choice of drugs and anaesthetic techniques. Methods used have included dividing the total annual expenditure by the number of patients treated and the use of severity of illness and workload scoring systems. Synthetic antibacterial drug containing one part trimethoprim to five of the sulphonamide sulfamethoxazole. Came into force in 1989 in Scotland, England and Wales, and in 1991 in Northern Ireland. Stipulate that employers must identify and control any substances which may be hazardous to health. Important guidance is given to allow 160 Cough replication and protein synthesis respectively. Side effects: nausea, diarrhoea, erythema multiforme, pancreatitis, hepatic impairment, blood dyscrasias. A deep inspiration is followed by forceful expiration against a closed glottis which is suddenly opened to allow explosive exhalation. An intrathoracic pressure of up to 40 kPa may be produced, and the peak expiratory flow may exceed 900 l/min. Afferent pathways for coughing are from the mucosa of the larynx, trachea and large bronchi via the vagus nerve and medulla, and are stimulated by physical or chemical irritants. Factors associated with coughing during anaesthesia include: insertion of a pharyngeal airway or tracheal tube if depth of anaesthesia is inadequate. Each cough increases intrathoracic pressure and expels arterial blood from the thorax; each gasp draws in venous blood. One coulomb is the amount of charge passing any point in a circuit in 1 s when a current of 1 ampere is flowing. Convey motor and sensory fibres involved in somatic, parasympathetic (visceral) and special visceral. In the middle cranial fossa, it passes forwards on the lateral wall of the cavernous sinus as far as the supraorbital fissure. Passes from the dorsum of the lower midbrain, then forwards in the lateral wall of the cavernous sinus to enter the supraorbital fissure. V: trigeminal nerve (sensory fibres supply the anterior dura, scalp and face, nasopharynx, nasal and oral cavities and air sinuses; motor fibres supply the muscles of mastication). The nerve passes from the pons to the trigeminal ganglion lateral to the cavernous sinus, where it divides into ophthalmic, maxillary and mandibular divisions. The motor nucleus is in the pons; the root bypasses the ganglion to join the mandibular division. Associated with the otic (parotid gland) and submandibular (submandibular and sublingual glands) ganglia. Sensory branches are the meningeal, buccal, auriculotemporal, inferior alveolar and lingual nerves. Somatic motor fibres supply the muscles of mastication (masseter, pterygoids, temporalis). Branches: - motor supply to the muscles of facial expression: divides within the parotid gland into temporal, zygomatic, buccal, mandibular and cervical branches from above down.
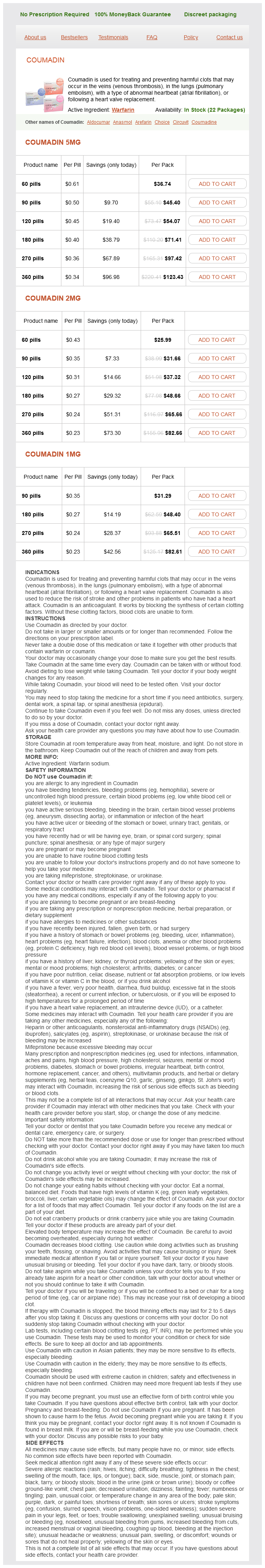
Warfarin Dosage and Price
Coumadin 5mg
- 60 pills - $36.74
- 90 pills - $45.40
- 120 pills - $54.07
- 180 pills - $71.41
- 270 pills - $97.42
- 360 pills - $123.43
Coumadin 2mg
- 60 pills - $25.99
- 90 pills - $31.66
- 120 pills - $37.32
- 180 pills - $48.66
- 270 pills - $65.66
- 360 pills - $82.66
Coumadin 1mg
- 90 pills - $31.29
- 180 pills - $48.40
- 270 pills - $65.51
- 360 pills - $82.61
They have been used in the treatment of cardiac failure and cardiogenic shock; stimulation of vascular 2-receptors causes vasodilatation and reduces afterload arteria umbilical unica consecuencias purchase discount warfarin online. Tamsulosin acts specifically at 1A-receptors and is used in benign prostatic hypertrophy. Labetalol and carvedilol (a drug with similar effects) are antagonists at both - and -receptors. Table 3 Classification and actions of adrenergic receptors Receptor type 1 Site Vascular smooth muscle Bladder smooth muscle (sphincter) Radial muscle of iris Intestinal smooth muscle Uterus Salivary glands Liver Pancreas Effect of stimulation Contraction Contraction Contraction Relaxation, but contraction of sphincters Variable Viscous secretion Glycogenolysis Decreased secretion of enzymes, insulin and glucagon Reduced release of noradrenaline Smooth muscle contraction Aggregation Increased rate and force of contraction Breakdown of stored triglycerides to fatty acids Increased renin secretion Relaxation Relaxation Relaxation Relaxation Variable; relaxes the pregnant uterus Watery secretion Glycogenolysis Increased insulin and glucagon secretion Lipolysis -Adrenergic receptor antagonist poisoning. General features include cardiac failure, bradycardia, cardiac conduction defects, hypotension, bronchospasm, coma and convulsions, the latter two especially with propranolol. Atropine is often ineffective but should be tried in vagalblocking doses (3 mg iv [40 µg/kg in children]). G protein-coupled receptors, activated by adrenaline and other catecholamines, and divided into - and -receptors. There is evidence for mixed receptor populations at both pre- and postsynaptic membranes. WaterhouseFriderichsen syndrome comprises bilateral adrenal cortical haemorrhage associated with severe meningococcal disease. In critically ill patients, treatment of occult adrenocortical insufficiency may be necessary for reversal of hypotension that is resistant to vasopressor drugs. Treatment: acute: iv saline, hydrocortisone 100 mg iv qds (preferably as the sodium succinate). Typically, both are required in primary insufficiency but only hydrocortisone in secondary insufficiency, although this may not always hold true. Polypeptide hormone (39 amino acids; mw 4500) secreted by corticotropic cells of the anterior pituitary gland in response to corticotropin releasing factor secreted by the hypothalamus. It increases corticosteroid synthesis in the adrenal glands, particularly glucocorticoids but also aldosterone. Statement, usually written, that provides for a mentally competent person to refuse certain future medical treatments, usually involving life-saving therapies, if he/ she were subsequently to become mentally or physically incompetent. From April 2007, in order to be legally valid, an advance decision must: be made by a person 18 years old, with the capacity to make it. System of advanced management of cardiac arrest and its training to paramedics, doctors, nurses and other healthcare professionals. Also encompasses the recognition and management of periarrest arrhythmias and postresuscitation care. Defibrillation should take place without delay for a witnessed or in-hospital cardiac arrest. A precordial thump should be considered for witnessed, monitored collapse when a defibrillator is not immediately available. Cardiac massage and ventilation at 30: 2; compressions should be uninterrupted once the airway has been secured. Lidocaine 1 mg/kg is an alternative if amiodarone is unavailable, but should not be used in addition (maximum 3 mg/kg in the first hour). Consider use of different pad positions/contacts, different defibrillator, buffers, if refractory. Magnesium sulphate 8 mmol may be indicated in hypomagnesaemia, torsades de pointes or digoxin toxicity. Tracheal administration of drugs is no longer recommended; the intraosseous 15 16 Advanced Life Support Group route is now the suggested alternative in the absence of iv access. Recent changes/controversies: importance of effective chest compressions with minimal interruption is emphasised, to a depth of 56 cm and at a rate of 100120/min; compressions to continue during defibrillator charging. Advance decisions may specify conditions under which patients do or do not wish to be resuscitated. Complications include trauma to abdominal organs and ribs and those associated with tracheal intubation/ attempted intubation and vascular access. Aimed at training medical and midwifery staff in the practical management of maternal and neonatal emergencies and provision of life support for the mother and child. Incorporates assessment of the airway, breathing and circulation with special emphasis on determining if the child has failure of respiration or circulation. Stresses the anatomical and physiological differences between adults and children whilst emphasising paediatric normal ranges. The patient is fully exposed to detect all life-threatening injuries, with resuscitation taking place in tandem with the primary survey. The need for radiographs of the chest, lateral cervical spine and pelvis should be considered during the primary survey but should not delay resuscitation (the cervical spine is assumed to require immobilisation for any injury above the clavicles until proven otherwise). Undesired drug effects, usually divided into: predictable (type A) dose-related side effects. Suspected adverse reactions are voluntarily reported to the Medicines and Healthcare products Regulatory Agency on yellow cards, introduced in 1964 and updated in 2000. Specific yellow cards for reporting anaesthetic drug reactions were introduced in 1988, to encourage reporting of serious reactions to established drugs and any reaction to new drugs. Anaesthetists give many different drugs iv to large numbers of patients, and therefore reactions are often seen. First exposure reactions tend to be milder and more frequent than those requiring prior exposure. Reported incidence varies between countries and according to definitions but severe allergic reactions are thought to occur in about 1: 10 000 to 1: 20 000 cases. A significant rise is suggestive of anaphylaxis, but its absence does not exclude it; conversely it can occur in non-allergic reactions, albeit to a lesser extent. Waiting for ~6 months after the reaction has been suggested in order to allow recovery of the immune system. A drug with high affinity binds more avidly than one with lower affinity, whatever its intrinsic activity.
© 2025 Adrive Pharma, All Rights Reserved..