General Information about Venlor
Venlor is available in both immediate-release and extended-release forms. The immediate-release type is taken two to a few occasions a day, while the extended-release type is taken as quickly as a day. It is essential to take the medicine precisely as prescribed by your doctor and to not cease taking it abruptly without consulting together with your doctor. Suddenly stopping Venlor can lead to withdrawal signs, such as nausea, headache, and temper modifications.
Venlor is typically prescribed for people who haven't responded properly to different antidepressant medications, corresponding to selective serotonin reuptake inhibitors (SSRIs). It may also be used for different circumstances, similar to nervousness issues, panic disorder, and social anxiousness disorder, as decided by a physician. However, it's not a first-line remedy for these conditions.
When taken as directed by a doctor, Venlor might help improve the symptoms of depression, together with temper, power ranges, urge for food, and sleep. It may take a quantity of weeks for the medication to reach its full impact, so it is essential to proceed taking it even when you don't discover an instantaneous enchancment.
Venlor, also known by its generic name venlafaxine, is a medication used for the remedy of melancholy. It belongs to the category of medicines known as serotonin-norepinephrine reuptake inhibitors (SNRIs) and works by growing the levels of serotonin and norepinephrine in the brain, two chemicals that play a job in temper regulation.
Depression is a severe psychological illness that impacts tens of millions of individuals worldwide. It is characterised by persistent emotions of unhappiness, hopelessness, and lack of interest in activities that one once loved. It can also result in physical symptoms similar to modifications in appetite, sleep disturbances, and fatigue. While the precise explanation for despair remains to be not totally understood, it is believed to be a result of a mixture of genetic, environmental, and psychological factors.
In uncommon circumstances, Venlor can even trigger extra serious unwanted facet effects, together with modifications in coronary heart price and blood strain, liver issues, and allergic reactions. These side effects are unusual however could be serious, so it is essential to search medical consideration when you expertise any unusual signs while taking Venlor.
As with any treatment, there are potential side effects related to Venlor. The commonest side effects embody nausea, dry mouth, headache, dizziness, and excessive sweating. These unwanted effects are normally gentle and may improve over time. However, in the event that they persist or turn out to be bothersome, it is very important communicate along with your physician.
It can be essential to note that Venlor can work together with different medications, so you will need to inform your doctor about all drugs, including over-the-counter medicines, vitamins, and herbal supplements, that you're taking.
In conclusion, Venlor is a commonly prescribed medication for the remedy of melancholy. It works by increasing the degrees of serotonin and norepinephrine in the brain, serving to to enhance temper and different signs of melancholy. While it might trigger some unwanted aspect effects, they are usually gentle and can be managed with close monitoring by a health care provider. If you would possibly be experiencing signs of melancholy, speak with your doctor to find out if Venlor is the proper therapy for you.
Effect of tumor necrosis factor alpha antagonists on serum aminotransferases and viraemia in patients with rheumatoid arthritis and chronic hepatitis C infection anxiety vs depression generic venlor 75 mg buy online. Tumor necrosis factor-alpha inhibitors and chronic hepatitis C: a comprehensive literature review. Hepatitis B and C virus infections and anti-tumor necrosis factor-alpha therapy: guidelines for clinical approach. Hepatotoxicity associated with sulfasalazine in inflammatory arthritis: a case series from a local surveillance of serious adverse events. Methotrexate is not associated with increased liver cirrhosis in a population-based cohort of rheumatoid arthritis patients with chronic hepatitis C. Leflunomide increases the risk of silent liver fibrosis in patients with rheumatoid arthritis receiving methotrexate. Effect of gastrointestinal manifestations on quality of life in 87 consecutive patients with systemic sclerosis. Malnutrition is common in systemic sclerosis: results from the Canadian scleroderma Research group Database. Muscarinic-3-acetylcholine receptor autoantibody in patients with systemic sclerosis: contribution to severe gastrointestinal tract dysmotility. Characteristics of patients with early systemic sclerosis and severe gastrointestinal tract involvement. Esophageal motor abnormalities in patients with scleroderma: heterogeneity, risk factors, and effects on quality of life. Loss of peristaltic reserve, determined by multiple rapid swallows, is the most frequent esophageal motility abnormality in patients with systemic sclerosis. Regional esophageal dysfunction in scleroderma and achalasia using multichannel intraluminal impedance and manometry. Distensibility of the anal canal in patients with systemic sclerosis: a study with the functional lumen imaging probe. Anorectal motility and sensation abnormalities and its correlation with anorectal symptoms in patients with systemic sclerosis: a preliminary study. Clinical features and prognosis of primary biliary cirrhosis associated with systemic sclerosis. Differences in disease features between childhood-onset and adult-onset systemic lupus erythematosus patients presenting with acute abdominal pain. Reversible acute gastrointestinal syndrome associated with active systemic lupus erythematosus in patients admitted to hospital. Acute abdominal pain in systemic lupus erythematosus: focus on lupus enteritis (gastrointestinal vasculitis). Ischemic colitis following colonoscopy in a systemic lupus erythematosus patient: report of a case. Opportunistic infections mimicking gastrointestinal vasculitis in systemic lupus erythematosus. Esophageal dysfunction in patients with mixed connective tissue diseases and systemic lupus erythematosus. The clinical characteristics of lupus related protein-losing enteropathy in Hong Kong Chinese population: 10 years of experience from a regional hospital. Systemic lupus erythematosus complicated with protein-losing enteropathy: a case report and review of published works. Increased risk of systemic lupus erythematosus in 29,000 patients with biopsy-verified celiac disease. Systemic lupus erythematosus complicated by cytomegalovirus-induced hemophagocytic syndrome and colitis. Gastroesophageal reflux incites interstitial lung disease in systemic sclerosis: clinical, radiologic, histopathologic, and treatment evidence. Management of gastrointestinal manifestations in systemic sclerosis (scleroderma). Does long term therapy with lansoprazole slow progression of oesophageal involvement in systemic sclerosis Comparison of surgical approaches to recalcitrant gastroesophageal reflux disease in the patient with scleroderma. Gastrointestinal manifestation of systemic sclerosis-thickening of the upper gastrointestinal wall detected by endoscopic ultrasonography is a valid sign. Systemic review: pathophysiology and management of gastrointestinal dysmotility in systemic sclerosis (scleroderma). Gastro-intestinal permeability is increased in patients with limited systemic sclerosis. Outcome of small-bowel motor impairment in systemic sclerosis-a prospective manometric 5-yr follow-up. Intestinal pseudo-obstruction caused by neuromyopathy in a patient with systemic sclerosis. Small intestinal bacterial overgrowth in patients suffering from scleroderma: clinical effectiveness of its eradication. Lower gastrointestinal symptoms and quality of life in patients with systemic sclerosis: a population-based study. Risk factors of mortality for salmonella infection in systemic lupus erythematosus. Pneumatosis cystoides intestinalis and benign pneumoperitoneum in a patient with antinuclear antibody negative systemic lupus erythematosus. Intestinal pseudo-obstruction in systemic lupus erythematosus: an uncommon but important clinical manifestation.
Side effects of fiber supplementation include abdominal distention anxiety definition purchase venlor 75 mg without a prescription, bloating, and flatulence, and along with its poor taste, can lead to poor patient adherence, especially for the first several weeks. Most controlled studies of the effects of fiber have shown that the minimum amount needed to consistently and significantly alter bowel function or colonic transit time is 12 g/day. To improve adherence, patients should be instructed to increase their dietary fiber intake gradually over several weeks to about 20 to 25 g/day. If results of therapy are inadequate, commercially packaged fiber supplements should be tried (Table 19. Some patients, particularly women with markedly delayed colonic transit, find that fiber aggravates abdominal distention. If patients fail to respond to a dietary fiber trial, slow transit constipation and/or a defecatory disorder could be suspected. One study of constipated patients with an average daily fecal weight of only 35 g showed an increase in fecal solids with 1, 2, and 4 g of methylcellulose/day, but fecal water increased only with the 4 g dose. Bowel frequency in this group of patients increased from an average of 2 to 4 stools a week, but the patients did not report marked improvement in consistency or ease of passage of stools (see Table 19. The suspensions, which are popular, have to be consumed quickly before the husk absorbs water. The granules may be stirred briskly in a half-glass of water and swallowed at once; carbonated water may be preferred. Although both stool dry and wet weights increase, the total weekly weights remain less than those of a healthy control group without treatment. In an observational study, 149 patients were treated with psyllium in the form of Plantago ovata seeds (15 to 30 g daily) for a period of at least 6 weeks. The response to treatment was poor among patients with slow colonic transit or a disorder of defecation, whereas 85% of patients without abnormal physiologic testing results improved or became symptom free. Nevertheless, the authors recommend a trial of dietary fiber before diagnostic testing is undertaken. Guar gum is approved for use in a number of foods and cosmetics and as a supplement. When used in high doses, guar gum has been reported to cause intestinal obstruction. Stool softeners and emollients are additional therapeutic agents (see later) (Tables 19. Osmotic Laxatives Osmotic laxatives increase fecal volume and reduce stool consistency by creating an intraluminal osmotic gradient that drives the secretion of water and electrolytes into the intestinal lumen. Poorly Absorbed Ions Magnesium, sulfate, and phosphate ions are poorly absorbed by the intestine and thereby create a hyperosmolar intraluminal environment. Their primary mode of action appears to be osmotic, but they may have other possible effects with unclear consequences, such as increasing prostaglandin concentrations in the stool. Magnesium sulfate is a more potent laxative that tends to produce a large volume of liquid stool and often leads to abdominal distention and sudden passage of a foulsmelling liquid stool. Use of magnesium, particularly in older adults, can be limited by adverse effects such as flatulence, abdominal cramps, and intravascular volume shifts. A small percentage of magnesium is actively absorbed in the small intestine; the remainder draws water into the intestine along an osmotic gradient. Hypermagnesemia-induced paralytic ileus is a rare complication,272 and hypermagnesemia with coma requiring hemodialysis has occurred in a child given 18 g/day of magnesium hydroxide for 7 days. With excessive use, even patients who are otherwise healthy can experience these complications, in addition to dehydration. Because phosphate is absorbed by the small intestine, a substantial dose must be ingested to produce an osmotic laxative effect, and it is not ideal for daily use. A rare but serious form of acute kidney injury has been associated with sodium phosphate solution used before colonoscopy, even in patients with normal baseline renal function (see Chapter 42). Lactulose is a nonabsorbable synthetic disaccharide that consists of galactose and fructose linked by a bond resistant to lactase. Lactulose is not absorbed by the small intestine but undergoes fermentation in the colon to yield short-chain fatty acids, hydrogen, and carbon dioxide, with consequent lowering of the fecal pH. When healthy volunteers receive lactulose 20 g (30 mL) daily, the sugar is not detectable in the stool. The time to onset of action is longer than that of other osmotic laxatives, and 2 or 3 days are required for lactulose to achieve an effect. Some patients report that lactulose is effective initially but then loses its effect, possibly due to alteration in the intestinal flora in response to the medication. Prolonged use of more than 1650 g of magnesium has been associated with hypermagnesemia. Tends to cause less bloating and cramps than other agents; tasteless and odorless, can be mixed with noncarbonated beverages. Typically used to prepare the colon for diagnostic examinations and surgery; also available as a powder without electrolytes for regular use. Cause apoptosis of colonic epithelial cells that are phagocytosed by macrophages; result in a lipofuscin-like pigmented condition known as pseudomelanosis coli; no definitive association has been established between anthraquinones and colon cancer or myenteric nerve damage (cathartic colon). Long-term use can cause malabsorption of fat-soluble vitamins, anal seepage, and lipoid pneumonia in patients predisposed to aspiration of liquids. Serious damage to rectal mucosa can result from extravasation of the enema solution into the submucosa. Hypertonic phosphate enemas and large-volume water or soapsuds enemas can lead to hyperphosphatemia and other electrolyte abnormalities if the enema is retained. Increases propulsion through the bowel by stimulation of5hydroxytryptamine4 receptors.
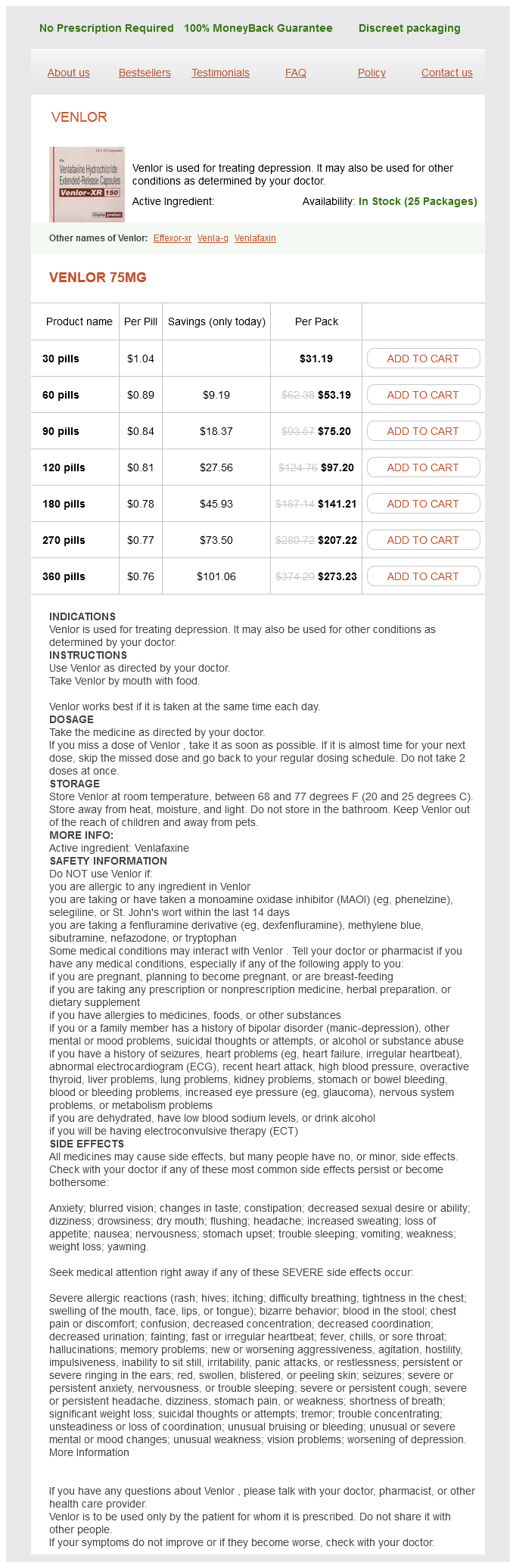
Venlor Dosage and Price
Venlor 75mg
- 30 pills - $31.19
- 60 pills - $53.19
- 90 pills - $75.20
- 120 pills - $97.20
- 180 pills - $141.21
- 270 pills - $207.22
- 360 pills - $273.23
Hepatobiliary diseases after kidney transplantation unrelated to classic hepatitis virus anxiety symptoms before period proven 75 mg venlor. Upper gastrointestinal bleeding during the first month after renal transplantation in the mycophenolate mofetil era. Incidence, management and risk factors for lower gastrointestinal bleeding in renal transplant recipients. Gastro-duodenal lesions and helicobacter pylori infection in uremic patients and rental transplant recipients. Gastrointestinal quality of life improvement of renal transplant recipients converted from mycophenolate mofetil to enteric-coated mycophenolate sodium drugs or agents: mycophenolate mofetil and enteric-coated mycophenolate sodium. Reduction of gastrointestinal complications in renal graft recipients after conversion from mycophenolate mofetil to enteric-coated mycophenolate sodium. Recurrence of autoimmune liver disease after liver transplantation: a systematic review. Natural history, risk factors and management of hepatitis C after liver transplantation. Recurrent hepatitis C after liver transplantation: clinical and therapeutical issues. The association between hepatitis C infection and survival after orthotopic liver transplantation. What determines the natural history of recurrent hepatitis C after liver transplantation Gastric ulcer perforation in heart-lung transplant patient: a successful case of early surgical intervention and management. Pretransplant gastroesophageal reflux compromises early outcomes after lung transplantation. Successful conversion from cyclosporine to tacrolimus for gastric motor dysfunction in a lung transplant recipient. The surgical management of severe gastroparesis in heart/lung transplant recipients. Improved lung allograft function after fundoplication in patients with gastroesophageal reflux disease undergoing lung transplantation. Fungal infection in heartlung transplant recipients receiving single-agent prophylaxi with itraconazole. Gastroesophageal reflux in cystic fibrosis: current understandings of mechanisms and management. Hepatitis virus infections in heart transplant recipients: epidemiology, natural history, characteristics, and impact on survival. Gastrointestinal infectious disease complications following transplantation and their differentiation from immunosuppressant-induced gastrointestinal toxicities. Adverse drug reaction driven immunosuppressive drug manipulations: a single-center comparison of enteric-coated mycophenolate sodium vs. Clostridium difficile colitis: increasing incidence, risk factors, and outcomes in solid organ transplant recipients. Update on cytomegalovirus infections of the gastrointestinal system in solid organ transplant recipients. Clostridium difficile colitis in patients after kidney and pancreas-kidney transplantation. Saccharomyces cerevisiae fungemia in a neutropenic patient treated with Saccharomyces boulardii. Supply of pre- and probiotics reduces bacterial infection rates after liver transplantation-a randomized, double-blind trial. Microsporidiosis in solid organ transplant recipients: two Enterocytozoon bieneusi cases and review. Incidence and risk factors for diarrhea following kidney transplantation and association with graft loss and mortality. Histological spectrum of mychophenolate mofetil-related colitis: association with apoptosis. Methylnaltrexone, a novel peripheral opioid receptor antagonist for the treatment of opioid side effects. Prevalence of cytomegalovirus in the gastrointestinal tract of renal transplant recipients with persistent abdominal pain. Intestinal amoebiasis in a patient with acute graft-versus-host disease after allogeneic bone marrow transplantation successfully treated by metronidazole. Strongyloides stercoralis hyperinfection in hematopoietic stem cell transplantation. The role of multiplex molecular panels for the diagnosis of gastrointestinal infections in immunocompromised patients. Diagnosis and treatment of digestive cryptosporidiosis in allogeneic haematopoietic stem cell transplant recipients:a prospective single centre study. Mucosal barrier injury: biology, pathology, clinical counterparts and consequences of intensive treatment for haematological malignancy: an overview. A second look at anorectal infections in cancer patients in a large cancer institute: the success of early intervention with antibiotics and surgery. Reactivated cytomegalovirus proctitis in an immunocompetent patient presenting as nosocomial diarrhea:a case report and literature review. Executive summary: clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Hepatitis C virus infection among hematopoietic cell transplant donors and recipients: American Society for Blood and Marrow Transplantation Task Force Recommendations. Impact of hepatitis C virus infection on clinical outcome in recipients after allogeneic hematopoietic cell transplantation. Hepatitis C virus infection after bone marrow transplantation: a cohort study with 10 year follow-up.
© 2025 Adrive Pharma, All Rights Reserved..