General Information about Trileptal
Trileptal, also recognized by its generic name oxcarbazepine, is an anticonvulsant medication primarily used for the therapy of epilepsy. It was first approved by the Food and Drug Administration (FDA) in 2000 and has since become a commonly prescribed medicine for those with seizure issues.
Trileptal works by stabilizing the electrical activity in the mind, stopping or lowering the occurrence of seizures. It does this by blocking the sodium channels within the brain, reducing the abnormal electrical exercise that leads to seizures. It is particularly effective in treating focal seizures, which originate in a selected a part of the mind.
In addition to its major use for controlling seizures, Trileptal has additionally been found to be efficient in managing different conditions similar to bipolar disorder and neuropathic pain. It has been used off-label for these situations, and while extra analysis is required, the outcomes have been promising.
Trileptal is available in pill or liquid form, and the dosage relies on the affected person's age, weight, and medical situation. It is necessary to follow the prescribed dosage and to not stop taking it without consulting a health care provider, as suddenly stopping can increase the chance of seizures.
However, as with all treatment, there are some precautions and potential dangers related to Trileptal. It may interact with other medications, together with birth control tablets, and will trigger start defects if taken during being pregnant. It is essential to seek the advice of with a healthcare skilled before starting or stopping any medications.
One of the primary advantages of Trileptal is its long-lasting impact. It is usually taken twice a day, and in contrast to another anticonvulsant drugs, it could present steady and constant seizure management with out frequent dosage changes. This makes it a convenient option for patients to manage their epilepsy.
In conclusion, Trileptal is an effective and convenient medication for the treatment of epilepsy. It is well-tolerated, has a long-lasting impact, and can also be used for other conditions. With correct administration and common monitoring, Trileptal can significantly enhance the standard of life for these living with epilepsy. However, you will need to focus on any considerations or potential risks with a healthcare professional earlier than starting this medication.
Trileptal can additionally be considered to have a favorable security profile in comparison with other anticonvulsants. It is usually well-tolerated and has a lower risk of serious unwanted effects. In scientific trials, the most common unwanted effects reported have been dizziness, drowsiness, and fatigue. These unwanted effects are often delicate and sometimes subside over time with continued use.
Epilepsy is a neurological dysfunction that affects hundreds of thousands of people all over the world. It is characterized by recurring seizures, that are sudden bursts of electrical exercise within the mind. These seizures can vary from mild to severe and can tremendously impact an individual's quality of life. Thankfully, there are medicines available to assist handle and management seizures. One such medication is Trileptal.
Prevention can be classified as primary (interventions in asymptomatic individuals to reduce known risk factors for the development of a disease) or secondary (to detect symptoms at an early stage and to intervene to stop further development or to improve the prognosis of the condition) medicine quizlet 600 mg trileptal buy free shipping. To stop recurrence of an illness or preventing it becoming chronic is tertiary prevention. There are known predisposing factors such as age, obesity, family history, parity/vaginal childbirth, and surgery. Identification of individuals at risk might help with implementing preventative measures. Although the prevalence of incontinence is increased in the elderly, the two do not necessarily have a cause-and-effect relationship; other pathological processes associated with aging might be responsible. Likewise, management of other risk factors such as chronic cough, smoking, and adjusting medication that has an adverse effect on the bladder could help incontinence. Regular toileting, easy access to toilets, restricting fluids (especially caffeine), and prevention of urinary tract infection. Menopause and Hormone Replacement Therapy There is a definite aging process in the lower urinary tract, resulting in atrophic change and poor urethral function. Urgency 126 Urgency is a distressing symptom for the older patient with restricted mobility, causing panic and anxiety on the sensation of bladder fullness. Often, patients void more frequently to prevent urgency incontinence, which can have the opposite effect, by reducing bladder capacity and worsening the symptoms. There is evidence that patients with urgency incontinence (more than once a week) are at increased risk of falls and bone fracture than in those without [48]. One study in morbidly obese women undergoing surgically induced weight loss showed subjective and urodynamic improvement in incontinence 1 year after surgery [55]. A randomized trial in 338 overweight and obese women found that a mean weight loss of 8% in the intervention group (vs. Familial and Genetic Factors Identification of risk groups is important and family history might be relevant. A small study in four pairs of postmenopausal identical twins with different parity status, i. Childbirth Vaginal birth probably has an important role in the pathogenesis of pelvic floor dysfunction. However, not all women develop pelvic floor problems following vaginal birth, suggesting that identifying "atrisk" groups might provide an opportunity for prevention [68]. Primigravidae with excessive bladderneck mobility antenatally (a possible marker for weak pelvic floor collagen) appear to be at higher risk 127 of postpartum stress incontinence [69], itself a risk factor for long-term incontinence [10]. Antenatal and prepregnancy incontinence [11,13] family history of incontinence in pregnancy, obesity [53], and persistent postnatal incontinence [70] also appear to be important risk factors. However, this assumption might not be correct; pregnancy itself might also be responsible [76]. Identifying women at risk before or early in a first pregnancy might enable preventative measures to be introduced. Prevention Cesarean Section Identification of risk groups might help with prevention, but what this intervention should be is a matter of debate. Results from these studies provide evidence for patient counseling and careful planning of mode of delivery to prevent pelvic floor dysfunction. Various models for scoring risk factors have been proposed and are being validated to provide estimates of postpartum pelvic floor pathologies to facilitate decision making and prevention of pelvic floor trauma [84,85]. It seemed that the more intensive the program, the greater the treatment effect [86]. Longer-term studies with 6 and 8 years follow-up [93,94] and one review [95] have shown that the initial beneficial effect does not persist, probably due to poor compliance. However, the incontinence in those women was not severe enough to require surgery. For example, there is conflicting evidence regarding prolonged second stage of labor, birth weight, epidural, episiotomy, and mode of delivery. A Cochrane review has shown an increased association of maternal perineal trauma with forceps delivery [96]. The review also suggested a significantly more third- or fourth-degree tears (with or without episiotomy), vaginal trauma, and flatus incontinence with forceps [96]. However, as with all studies assessing episiotomy, the technique and angle are poorly described (see later). It would appear that prevention by changing obstetric practice is not possible with the current state of knowledge. However, it might be worthwhile considering earlier delivery (by cesarean section) in short stature primigravidae who have obstructed labor before full dilatation to prevent pelvic floor injury [28]. Despite repair, 30%50% of affected women suffer from anal incontinence [102104], and 40% will opt for a future elective cesarean section to avoid worsening of symptoms from a further vaginal birth [105,106]. A higher risk of third- or fourth-degree perineal tears was associated with a maternal age above 25 years; instrumental delivery (forceps and ventouse), especially without episiotomy; Asian ethnicity; a more affluent socioeconomic status; higher birth weight; and shoulder dystocia. The authors concluded that changes in risk factors were unlikely explanations for the observed increase and that this was likely due to better training and recognition. For example, the "overlap repair" for complete tears seems to be associated with a lower incidence of fecal urgency and deterioration of anal incontinence symptoms compared with "end-to-end" repair [110]. This is ongoing via excellent courses run throughout the world (Sultan A and Thakar R, personal communication). For example, fewer third- and fourth-degree tears have been seen following mediolateral episiotomy [111,112], whereas the risk is increased by midline episiotomy [113]. Standard obstetrics textbooks state that a mediolateral episiotomy should be performed at an angle of at least 40°, with most suggesting an angle of between 45° and 60°.
It should be noted that avoiding fluid intake in the evening hours can be helpful for reducing nocturia treatment of diabetes cheap trileptal 300 mg amex. Similarly, it can be very helpful for some patients to restrict fluids for a time when toilet access will be limited, such as before a church service. Women using such targeted fluid restriction should be reminded to compensate for these missed fluids earlier or later to ensure that their total daily fluid intake is adequate. In patients who consume an abnormally high volume of liquids, fluid restriction is often appropriate. Some patients maximize their fluid intake deliberately in the belief that they need to "flush" their 649 kidneys, to avoid dehydration, or in an effort to lose weight. It is not uncommon to see women carry a water bottle throughout the day taking frequent drinks for health reasons. In these cases, reducing excess fluids can relieve problems with sudden bladder fullness and urgency. Caffeine Reduction Caffeinated beverages in particular can exacerbate incontinence because in addition to its diuretic effect, caffeine is a bladder irritant for many people. Research has demonstrated that caffeine increases detrusor pressure [58] and that it is a risk factor for detrusor instability [59,60]. Evidence also exists that reducing caffeine intake helps to reduce episodes of incontinence [6163]. Although it is very difficult for most coffee drinkers to completely eliminate it from their diet, provided with the knowledge that caffeine may be aggravating their incontinence, many will be willing to reduce their intake or to eliminate it for a few days as a trial. Reducing caffeine intake can be done gradually by mixing decaffeinated beverages with caffeinated beverages in increasing increments. For example, coffees can be mixed to consist of ¼ decaffeinated coffee in week 1, ½ in week 2, ¾ in week 3, and full decaffeinated coffee in week 4. Avoiding Bladder Irritants Many clinicians recommend, even as a first-line approach, restricting certain foods and beverages that are believed to irritate the bladder, including sugar substitutes, citrus fruits, spicy foods, and tomato products. Although there is little scientific evidence on dietary factors, there are many cases in which these substances appear to be aggravating incontinence, and reducing or eliminating them has provided clinical improvement. A diary of food and beverage intake can sometimes be useful in identifying which substances are irritants for individual patients. Rather than recommending that all patients restrict their intake of these substances, a diary or trial restriction can help to identify which patients are sensitive and may chose to reduce their intake. Women with higher body mass index are not only more likely to develop incontinence, but they also tend to have more severe incontinence than women with lower body mass index. Research on the relationship between body mass index and incontinence reports that each five-unit increase in body mass index increases the risk of daily incontinence by approximately 60% [64,65]. Intervention studies of morbidly obese women report significant improvement in symptoms of incontinence with weight loss of 4550 kg following bariatric surgery [6668]. Similarly, significant improvements in continence status have been demonstrated with as little as 5% weight reduction in more traditional weight loss programs [69]. Both groups received a booklet describing a step-by-step self-administered behavioral program to reduce incontinence. The weight loss program, which resulted in a mean weight loss of 8%, showed significantly greater reductions in number of incontinence episodes compared to the control group, which had a mean weight loss of 1. Because moderate weigh loss is an achievable goal for many women, it is rationale to recommend weight loss as a first-line treatment or as part of a comprehensive program to treat incontinence in overweight and obese women. Bowel Management Fecal impaction and constipation have been cited as factors contributing to urinary incontinence in women, particularly in nursing home populations [71]. In severe cases, fecal impaction can be an irritating factor in overactive bladder or obstruct normal voiding, causing incomplete bladder emptying and overflow incontinence. Disimpaction relieves symptoms for some patients, but it can recur in the absence of a bowel management program. Bowel management may consist of recommendations for a normal fluid intake and dietary fiber (or supplements) to maintain normal stool consistency and regular 650 bowel movements. When hydration and fiber are not enough, stool softeners or enemas may be used to stimulate a regular daily bowel movement, preferably after a regular meal such as breakfast to take advantage of postprandial motility. This reliance on patient behavioral change is perhaps the main limitation of this treatment approach. Like any new habit or skill, changing daily bladder habits and learning new skills require effort and persistence over time. It can be challenging for women to remember to use their muscles strategically in daily life as well as to maintain a regular exercise regimen for strength and skill. A key ingredient in addressing this challenge is to maintain contact with the patient during this period of time when her benefit is not yet appreciable. In addition, when initiating behavioral treatment, it is important to make it clear to the patient that her improvement, as with any new skill, will likely be gradual, with good days and bad days, and that it will depend on her consistent practice. The patient who expects this course of treatment will be better prepared to persist over time so that results can be achieved and maintained long term. Little research has examined the durability of behavioral treatments in the long term, but studies are promising in that many patients are able to sustain improvements in bladder control over time [7274]. Most patients who engage actively with behavioral treatment for incontinence experience some degree of improvement, yet there is considerable variation in outcomes. Little is known to help us predict which patients will respond best to behavioral treatment.
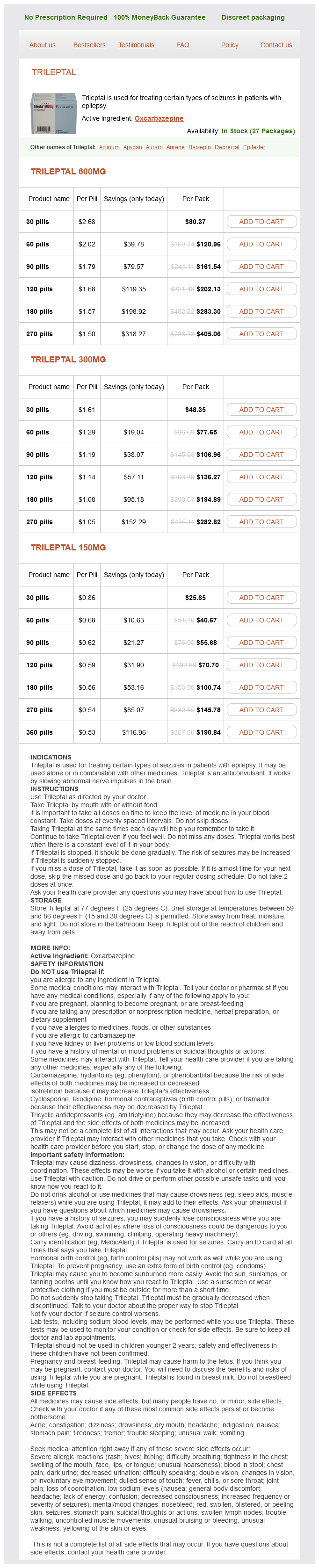
Trileptal Dosage and Price
Trileptal 600mg
- 30 pills - $80.37
- 60 pills - $120.96
- 90 pills - $161.54
- 120 pills - $202.13
- 180 pills - $283.30
- 270 pills - $405.06
Trileptal 300mg
- 30 pills - $48.35
- 60 pills - $77.65
- 90 pills - $106.96
- 120 pills - $136.27
- 180 pills - $194.89
- 270 pills - $282.82
Trileptal 150mg
- 30 pills - $25.65
- 60 pills - $40.67
- 90 pills - $55.68
- 120 pills - $70.70
- 180 pills - $100.74
- 270 pills - $145.78
- 360 pills - $190.84
Alternatively medicine 257 buy generic trileptal 300 mg on-line, manual reduction of the uterus can be performed or a Hodge pessary may be inserted to maintain uterine position and relieve the obstruction on the bladder neck. Risk factors include a first labor, instrumental delivery epidural analgesia, and a longer duration of labor (800 minutes) [62]. Studies have looked at sensation after delivery [63] and found that the bladder can take up to 8 hours to regain sensation after the last top-up of an epidural. Overdistension of the bladder may occur during this period, leading to permanent detrusor dysfunction. Urinary Incontinence Incontinence is a common symptom associated with pregnancy and has been reported in up to 85% of women [64]. Francis [63] found that in the first trimester of pregnancy 16% of women complained of stress incontinence and 34% in the second half of pregnancy. Viktrup and Lose [8] interviewed 305 primiparae and found that 39% had stress incontinence before, during, or after pregnancy and 7% developed de novo stress incontinence after delivery. The association with these obstetric risk factors was lost by 3 months postpartum. However, in a subsequent follow-up study of the original cohort of 278 women, they reported a prevalence of stress incontinence of 30% at 5 years. In those without symptoms after the first delivery, the incidence was 19%; however, in those who reported stress incontinence 3 months after the first delivery, there was a 92% risk of having stress incontinence 5 years later [8]. A prospective cohort study of 949 women undertaken to find risk factors for postpartum stress incontinence at 3 months 918 found that urinary incontinence was experienced by 22. New onset urinary incontinence was more common in parous compared to nulliparous women. This study highlights the high proportion of women who suffer from urinary incontinence as 15. It confirms previous data that have found that the presence of antenatal and prepregnancy stress incontinence seems to increase the risk of future stress incontinence [66,67]. The pattern of the development of incontinence during pregnancy, with rapid postpartum recovery followed by a steady decline of continence over time, suggests a dual mechanism of nerve and tissue damage. The evidence regarding the contribution of obstetric factors to the development of stress incontinence is conflicting. The data are unclear whether it is pregnancy or the birth itself that is the major contributor to postpartum incontinence. Some investigators have found a relationship with the duration of the second stage of labor [68,69] and birth weight [1]. Conversely, other investigators have found no significant correlation between stress incontinence and fetal head circumference [70], second stage of labor [1,71], or birth weight [9092]. However, most of these studies are relatively small population studies that differ widely in their questioning techniques and definition of stress incontinence. Thus, pregnancy itself rather than the mode of delivery may also be an etiological factor in the development of urinary incontinence. Epidural analgesia has been reported to be more protective than pudendal block against postpartum stress incontinence [90]. However, this has not been supported by other research that has found a higher incidence of stress incontinence in those who received epidural analgesia than those who did not [92]. Changes in the Lower Urinary Tract and Pelvic Floor Related to the Development of Incontinence the exact etiological mechanism of stress incontinence is unclear and probably multifactorial, related to nerve damage and/or physiological and structural changes of the lower urinary tract. Functional Changes Iosif and Ulmsten [72] compared urethral pressure profile measurements in pregnant women with stress incontinence with continent healthy women from an earlier study. The maximum urethral closure pressure increased to 93 cmH2O at 38 weeks and then dropped to prepregnancy values of 69 cmH2O postpartum. These changes were not seen in women complaining of incontinence and are postulated to be a mechanism whereby continence is maintained despite an increase in intravesical pressure in pregnancy. This corresponds with other studies that have shown evidence of low urethral pressure in nonpregnant women with stress incontinence [59,73]. This increase in urethral closure pressure may be the result of an increase in urethral sphincter volume from increased blood flow. There is also an increase in the amplitude of vascular pulsations recorded from the urethral wall, especially in the first 16 weeks of pregnancy, which may be related to an increase in blood volume in pregnancy. Pregnant women with urodynamic stress incontinence showed a decrease in the amplitude of vascular pulsations in the periurethral plexus compared to continent women, suggesting that this affects urethral closure pressure [74]. Three-dimensional imaging of the urethral sphincter after vaginal delivery shows a reduction in sphincter volume, which has been implicated in the development of stress incontinence [75]. The mean values for urodynamic variables in the third trimester and postpartum were lower than the values defined in a nonpregnant population and not related to obstetric or neonatal variables (Table 58. However, despite the high prevalence of symptoms in this study, there was poor correlation between symptoms and urodynamic findings, which agrees with data in nonpregnant women [76]. Therefore, these observed changes in bladder function were consistent with a pressure effect of a gravid uterus and not related to mode of delivery or neonatal factors. Nerve Damage Patients with urodynamic stress incontinence have been shown to have abnormal conduction in the perineal branch of the pudendal nerve, which innervates the periurethral striated muscle and pubococcygeus muscle [77,78]. This damage is likely to lead to a loss of striated muscle of the urethral sphincter [79]. The degree of pudendal nerve damage was greater in multiparous women and correlated with the use of forceps and a longer second stage of labor [77,78]. In 60% of these women, pudendal nerve latency had returned to normal at 2 months postpartum [12].
© 2025 Adrive Pharma, All Rights Reserved..