General Information about Trihexyphenidyl
Artane is out there in two varieties: tablets and an injectable solution. The tablets are usually taken one to three instances a day with or with out food. The dosage is tailored to every particular person primarily based on their signs and response to the medication. Injections are usually reserved for more extreme instances of Parkinson's disease, particularly when patients are unable to take the oral kind. The injection is normally given once each three to 4 weeks, but the dosage might differ.
In conclusion, Artane, also called Trihexyphenidyl, is a medication generally used to deal with the signs of Parkinson's disease and other muscular conditions attributable to certain drugs. It works by blocking the effects of acetylcholine, helping to revive the balance of neurotransmitters within the brain. While Artane is mostly well-tolerated, it is important to discuss any potential unwanted aspect effects with a physician and comply with the prescribed dosage accordingly. With correct use, Artane can greatly improve the quality of life for individuals living with Parkinson's illness and different similar situations.
Trihexyphenidyl, commonly generally identified as Artane, is a prescription medication used to treat the symptoms of Parkinson's disease. This neurological disorder affects the central nervous system, inflicting quite a lot of movement-related points such as stiffness, tremors, spasms, and poor muscle management. Artane belongs to a class of medications referred to as anticholinergics, which work by blocking the motion of a neurotransmitter called acetylcholine. It can be used to deal with related muscular circumstances attributable to certain drugs, including chlorpromazine, fluphenazine, perphenazine, haloperidol, thiothixene, and others.
As with any treatment, Artane may cause side effects. The most common side effects embody dry mouth, blurred vision, and drowsiness. Other attainable unwanted aspect effects embrace nausea, constipation, and urinary retention. Some individuals may also expertise confusion, hallucinations, and reminiscence issues. It is necessary to discuss any considerations or potential side effects with a doctor earlier than beginning Artane or making any modifications to the dosage.
Aside from treating Parkinson's disease, Artane is also prescribed to treat and stop the same muscular situations attributable to certain drugs. These circumstances, also referred to as extrapyramidal signs, include muscle spasms, stiffness, and tremors. These signs are commonly related to medications used to deal with psychiatric disorders, corresponding to schizophrenia and bipolar disorder. Artane is particularly effective in treating these signs as a result of it particularly targets the underlying trigger of those signs, which is the overstimulation of acetylcholine.
Artane works by blocking the effects of acetylcholine, a neurotransmitter that helps control movements throughout the body. In Parkinson's disease, there is an imbalance between dopamine and acetylcholine, resulting in the overstimulation of acetylcholine. This results in the signs of Parkinson's illness. By blocking acetylcholine, Artane helps to restore the balance between these two neurotransmitters, alleviating the symptoms and bettering motor perform.
Parkinson's disease is a progressive disorder that impacts approximately one million folks within the United States alone. It is attributable to a loss of dopamine-producing cells within the mind, resulting in a decrease in dopamine levels. Dopamine is a chemical messenger that is responsible for regulating movement, mood, and cognition. As the levels of dopamine decrease, it causes the standard symptoms of Parkinson's illness, corresponding to tremors, rigidity, and problem with actions. Other non-motor signs can embrace despair, anxiety, sleep disturbances, and cognitive impairment.
From this point where the nerve divides to the midline pain treatment for herniated disc order trihexyphenidyl canada, medial and lateral alveolar plates of bone develop in relation to the forming tooth germs subdividing the trough of bone. Thus the teeth come to occupy individual compartments, which finally are enclosed totally by growth of bone over the tooth germ. This point of divergence is marked by the lingula in the adult mandible, the point at which the inferior alveolar nerve enters the body of the mandible. As the cartilage is degraded, the space previously occupied by cartilage becomes filled with new bone. Forward from this point to the midline, some evidence exists that the cartilage might make a small contribution to the mandible by means of endochondral ossification. The further growth of the mandible until birth is influenced strongly by the appearance of three secondary (growth) cartilages and the development of muscular attachments. These secondary cartilages include (1) the condylar cartilage, which is most important; (2) the coronoid cartilage; and (3) the symphyseal cartilage. They have a different histologic structure from the primary cartilages in that their cells are larger, and less intercellular matrix is formed. The condylar cartilage appears at 12 weeks of development and rapidly forms a cone-shaped or carrot-shaped mass that occupies most of the developing ramus. This mass of cartilage is converted quickly to bone by endochondral ossification (see Chapter 6), so that at 20 weeks of development only a thin layer of cartilage remains in the condylar head. This remnant of cartilage persists until the end of the second decade of life, providing a mechanism for growth of the mandible, in the same way as the epiphyseal cartilage does in the limbs. The coronoid cartilage appears at about 4 months of development, surmounting the anterior border and top of the coronoid process. Coronoid cartilage is a transient growth cartilage and disappears long before birth. Small islands of cartilage also may appear as variable and transient structures in the developing alveolar processes. Maxilla the maxilla also develops from a center of ossification in the mesenchyme of the maxillary process of the first arch. No arch cartilage or primary cartilage exists in the maxillary process, but the center of 104 ossification is associated closely with the cartilage of the nasal capsule. As in the mandible, the center of ossification appears in the angle between the divisions of a nerve (that is, where the anterosuperior dental nerve is given off from the inferior orbital nerve). As a result of this pattern of bone deposition, a bony trough forms for the infraorbital nerve. From this trough a downward extension of bone forms the lateral alveolar plate for the maxillary tooth germs. The medial alveolar plate develops from the junction of the palatal process and the main body of the forming maxilla. This plate, together with its lateral counterpart, forms a trough of bone around the maxillary tooth germs, which eventually become enclosed in bony crypts in the same way as described for the mandible. Arrows indicate the future directions of bone growth to form the lateral and medial alveolar plates. A zygomatic, or malar, cartilage appears in the developing zygomatic process and for a short time adds considerably to the development of the maxilla. At birth the frontal process of the maxilla is well marked, but the body of the bone consists of little more than the alveolar process containing the tooth germs and small though distinguishable zygomatic and palatal processes. The body of the maxilla is relatively small because the maxillary sinus has not developed. This sinus forms during the sixteenth week as a shallow groove on the nasal aspect of the developing maxilla. At birth the sinus is still a rudimentary structure about the size of a small pea. In the first branchial arch, a gradient of gene expression involving the Dlx family of transcription factors (1 to 6), the so-called intra-arch Dlx code, promotes coordinated gene expression along the dorso-ventral axis that regulates jaw patterning. Distinct sets of Dlx family members are important for determining the identity of the mandible (Dlx1/2/5/6) versus the maxilla (Dlx1/2). A dramatic demonstration of the importance of the selective set of Dlx molecules in jaw specification is observed in mice lacking both Dlx5 and 6 genes. Lack of Dlx5/6 causes a reversal of the mandible into a maxilla, generating an animal with two mirror-image upper jaws. Dlx5/6 activate expression of other downstream transcription factors (Dlx3/4, heart- and neural crest derivativesexpressed 1 and 2[Hand1/2], Alx3/4, Pitx1, gastrulation brain homeobox 2 [Gbx2], bone morphogenic protein 7 [Bmp7]) important for mandibular development processes and repress others (pou domain class 3, transcription factor 3 [Pou3f3], forkhead box l2 [Foxl2], Iroquois homeobox protein 5 [Irx5]) that are themselves important for maxillary processes and under control of Dlx1/2. Thus Dlx family members are critical for determining the identity of the mandible versus the maxilla. Another level of complexity is brought about by local environmental signaling cross talk that directly or indirectly modulates the transcriptional Dlx program. Targeted ablation of the endothelin pathway in mice causes duplication of maxillary processes, whereas ectopic expression induces duplication of the mandibular processes. Common Features of Jaw Development this account of jaw development shows that in their development the mandible and maxilla have much in common. Both begin from a single center of membranous ossification related to a nerve, both form a neural element related to the nerve, and both develop an alveolar element related to the developing teeth. Development of the Temporomandibular Joint the temporomandibular joint is an articulation between two bones initially formed from membranous centers of ossification. Before the condylar cartilage forms, a broad band of undifferentiated mesenchyme exists between the developing ramus of the mandible and the developing squamous tympanic bone. With formation of the condylar cartilage, this band is reduced rapidly in width and is converted into a dense strip of mesenchyme.
This very first birth has later been followed by three more births cordova pain treatment center memphis generic trihexyphenidyl 2 mg with amex, proving that the outcome of uterus transplantation at this early stage of clinical implementation exceeds expectations for a novel surgical method (6). Given these results, many more cases of uterus transplantation performed at other centers are to be expected in the near future. This article reviews the worldwide experience of uterus transplantation as a treatment for absolute uterine factor infertility and the future prospects of uterus transplantation. Yet women with uterine factor infertility represent a substantial portion of the infertile population, and for decades have remained the largest non-treatable fraction. This research field was rediscovered in the early 2000s, and has since been progressing rapidly. Uterus transplantation models have been developed in several animal species including rodents (79), large domestic species (1013), and nonhuman primates (1416). The experiments have been focusing on a variety of aspects of uterus transplantation such as optimizing the surgery (17), recognition and monitoring of rejection episodes (8,15,18), and ischemic effects (19,20). Successful pregnancies and live births have been described in different species including mice (19,21), rats (22,23), sheep (11,24) and non-human primates (25). In addition, stable uterine allografts have also been achieved in large animals (14). Nevertheless, due to a growing demand for organs, live donor donations are essential to meet current patient needs. Consequently, despite involving non-negligible risks for the donor, live donation is practiced in several organ transplantation settings. Out of the 11 published cases and one unpublished case of human uterus transplantations performed worldwide up until 2015, 11 were performed with uteri from live donors (2,4) and only one with a uterus from a deceased donor (Table 63. A comparison concerning the different aspects relating to the living and deceased donor surgical concepts in uterine transplantation is stated below and in Table 63. Surgery in the live donor setting In a live donor setting, it is possible to optimize the planning of the surgery, and this concept yields sufficient time to evaluate the donor and organ prior to transplantation. Unsuitable and inappropriate donor candidates and organs of inferior quality can be excluded and thus enhance the outcome. Comparison of a living donor versus a deceased donor setting in uterus transplantation Living donor Planning of surgery Investigation of donor qualities Investigation of organ qualities Donor autonomy Donor pain Donor time commitment Donor complication Long-term organ function Complexity of surgery Abbreviations: Table 63. The recipient and donor should have the transplantation at a specific date when both parties are in optimized condition, with fully prepared surgical teams, thus increasing the odds of graft survival. A major disadvantage in the live donor setting is the surgical risk for the donor and the innate risks associated with the retrieval surgery. The technically most demanding part in the surgical procedure and thus most likely to create complications is the dissection of the uterine veins and ureters. To minimize the risk for the live donor, it has been suggested that a larger alternative vein, such as one of the ovarian veins, would be preferable to use for anastomosis (29). This would probably require removal of the ovary itself, resulting in hormonal dysfunction in a premenopausal donor. Because of the resulting hormonal dysfunction, the live donor setting with the selection of the ovarian veins will only be suitable for use in postmenopausal donors. The uterine branch of the utero-ovarian vein may provide an adequately good substitute for anastomosis, but the lengths may be poorer. In the future, the surgical technique for uterus transplantation will most likely undergo development and the risks of surgical complications are surely likely to decrease. Moreover, new, less invasive methods like robotic-assisted laparoscopy may provide options to minimize the risk for the donor in a live donor setting (30). In 2000, the first human uterus transplantation was performed in Saudi Arabia (2). A 26-year-old woman who had previously an emergency peripartum hysterectomy received a uterus from a 46-year-old donor. The non-related healthy donor was scheduled for bilateral oophorectomy due to benign bilateral ovarian cysts. The vascular pedicles recovered with the uterus were of insufficient lengths for direct anastomosis to the external iliac vessels and elongated by segments of the saphenous veins. Vascular anastomoses were established with the extended vascular pedicles end-to-side to the external iliac vessels of the recipient. In the donor, a perioperative small ureteric laceration was reported and repaired perioperatively by a urologist (2). The authors advocated that insufficient tissue graft support led to tension and thrombosis of the supplying vessels. The 2013 Swedish uterus transplantation trial, in which nine recipients received a uterus, also used the live donor concept (4). All of the donors had a minimum of one normal pregnancy and subsequent delivery prior to transplantation. Five of the donors were postmenopausal, and cyclic hormonal pretreatment was given to these women before uterus transplantation to ensure withdrawal bleedings. The uterus recovery included dissection and separation of the graft with long bilateral vascular pedicles of the uterine arteries from the internal iliac arteries distal to the branching of the gluteal artery. Preparation of the recipients included dissection of the external iliac vessels, separation of the vaginal vault from the bladder and rectum, and preparation of uterine fixation sites (rudimentary round ligaments and paravaginal connective tissues). Endto-side vascular anastomoses of the uterine veins of the graft to the external iliac veins of the recipient and of the anterior divisions of the internal iliac arteries to the external iliac arteries bilaterally were performed. Due to the complex and thorough dissection of the ureters with intact uterine veins and arteries, the donor surgeries lasted longer than estimated, with durations of >10 hours.
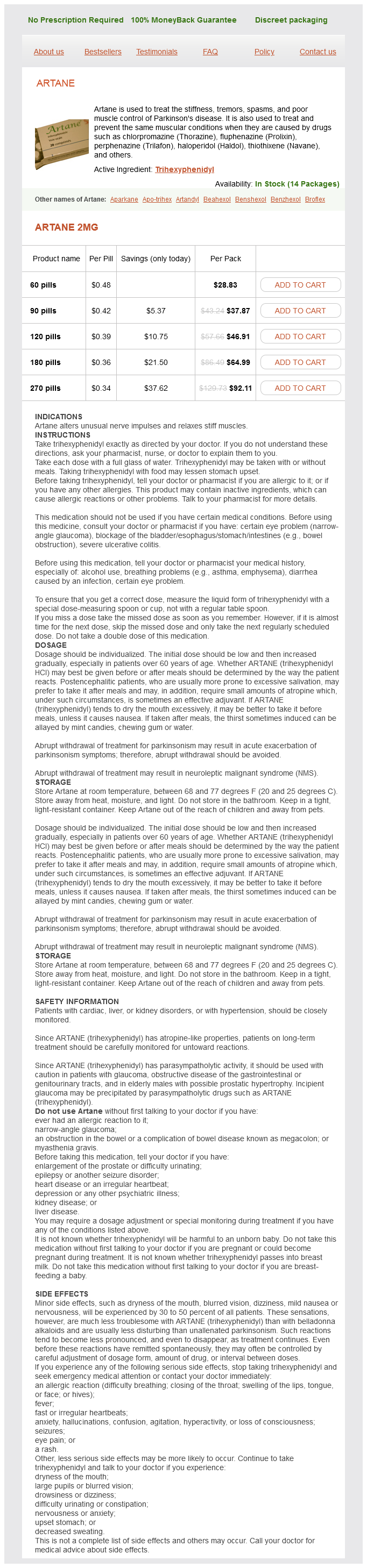
Trihexyphenidyl Dosage and Price
Artane 2mg
- 60 pills - $28.83
- 90 pills - $37.87
- 120 pills - $46.91
- 180 pills - $64.99
- 270 pills - $92.11
Within this area are the spine treatment for long term shingles pain purchase trihexyphenidyl 2 mg fast delivery, pelvic bones, hips, pelvic floor muscles, connective tissue, pelvic nerves, and pelvic organs. Pain with no objective sensory impairment Pain relieved by diagnostic pudendal block. Striated muscles, connective tissue, and ligaments provide mechanical support for pelvic organs. Pelvic floor muscles are made of Type 1 slow twitch and Type 2 fast twitch skeletal fibers [7]. This multimodal pelvic floor musculature assists with core stability and closure of the urogenital hiatus and is responsible for voluntary control of bowel, bladder, and sexual functions. The individual pelvic floor muscles have unique clinical characteristics that the pelvic floor physical therapist considers. The transverse perinei muscles are the site of most episiotomies and/or tearing during vaginal delivery. Even after the trauma has healed these muscles may develop significant scarring that can impede muscle expansion and cause pain with penetration. With overactivity or myofascial trigger points, the obturator internus can contribute to pain with sitting, dyspareunia, and constipation. Additionally, overactivity in muscles surrounding the urethra can create urethral discomfort, dysuria, and incomplete bladder voiding [9]. This is the only nerve in the pelvic area that has motor, sensory and autonomic functions. The pudendal nerve has three branches: the dorsal clitoral, posterior labial (perineal), and inferior rectal. These branches provide sensory, motor, and sympathetic innervation to the vulva and vagina. Injury to the entire nerve or any of its branches may result in urogenital pain, dyspareunia, and female genital arousal disorder. Pudendal nerve pain is often referred to as pudendal neuralgia, which is currently defined by the Nantes criteria (Box 21. These nerves include the ilioinguinal, iliohypogastric, genitofemoral, and posterior and lateral femoral cutaneous nerves. Careful Musculoskeletal Management of Pelvic and Sexual Pain Disorders Obturator n. Connective tissue is a key component of the pelvic floor and covers its structures. The collagen provides tensile strength, while the elastin provides flexibility [14]. Fascia is a type of connective tissue that is found throughout the abdominopelvic region. Damage or an insult to the pelvic floor may injure the connective tissue or fascia, which then may become a primary or a secondary contributor to pelvic and sexual pain disorders, ranging from mild to significant in severity [16]. Pathophysiology of Sexual Pain the pathophysiology of pelvic floor dysfunction involves impairment in the functional anatomy of the pelvic floor. Any process that interrupts the integrity of pelvic neuromusculoskeletal 300 Textbook of Female Sexual Function and Dysfunction or connective tissue can result in dysfunction of the bowel, bladder, and sexual activity, or problems with core stability or abdominopelvic organ support and function. Pelvic floor impairments leading to sexual pain include overactive pelvic floor muscles, skeletal abnormalities, myofascial restrictions, and inflammation. Neuromusculoskeletal impairments cause somatosensory stimulation that may result in inhibition or excitation of visceral functions; this effect is called the somatovisceral reflex. This reflex can cause diffuse pain throughout the pelvis and can contribute to dyspareunia. Due to the physiology and biomechanics of the lumbosacropelvic region, muscle overactivity may result from chronic straining, poor postures in the sitting, standing, or toileting positions, dysfunctional gait patterns, previous sexual or physical abuse, or harmful repetitive movements from a sport or work activity. Overactive pelvic floor muscles may also result from childbirth injuries, infection, a traumatic event, cancerrelated treatments, and abdominal or pelvic surgery. Autoimmune disorders and inflammatory conditions, including fibromyalgia, ulcerative colitis, interstitial cystitis, inflammatory bowel disorders, and endometriosis, can also contribute to pelvic floor muscle overactivity [7, 17, 18]. Regardless of the initial insult, disruption of appropriate movement patterns results in dysfunctional modifications of the pelvic floor musculature and connective, visceral, and neural tissues [1921]. Biomechanical abnormalities due to musculoskeletal causes, such as scarring and adhesions, skeletal misalignment, tissue lengthening or shortening, and muscular asymmetry, may be the primary cause of myofascial trigger points, shortened myosarcomeres and connective, visceral, and neural restrictions from reduced range of motion [20]. Myofascial trigger points are hyperirritable points or nodules in skeletal muscle that possess high levels of inflammatory mediators and sensitized nociceptors [22]. Myofascial system dysfunction has been shown to be an important contributor to pelvic pain; up to 78% of women with chronic pelvic pain may suffer from some form of myofascial dysfunction [3]. Prolonged pelvic floor muscle contraction due to habit or lack of awareness can also cause myofascial trigger points and restrictions. Detrimental holding patterns may also be secondary to painful or noxious stimuli from various pelvic disorders, such as vulvodynia, vestibulodynia, persistent genital arousal disorder, bladder pain syndrome, irritable bowel syndrome, and incontinence [23]. These conditions contribute to muscle overactivity because of muscle guarding, shortening of skeletal sarcomeres and connective tissue, reduction in the mobility and range of motion of nerves, decreased blood flow, decreased tissue perfusion, and the development of myofascial trigger points [24, 25]. In turn, pelvic floor muscle overactivity can cause or contribute to pain in these disorders. Muscle and connective tissue abnormalities and myofascial trigger points result in localized, referred, or radiating pain and tenderness [26]. As a result, the affected areas exhibit increased restrictions and decreased mobility, which further perpetuate the pain cycle. Common areas of myofascial pain and trigger points are in the back, thigh, gluteal, abdominal, and pelvic floor muscles. Altered connective tissue tension may result in tissue hypoxia leading to sensations of burning, itching, tingling, cold, shooting, and/or sharp pain [20, 27, 28].
© 2025 Adrive Pharma, All Rights Reserved..