General Information about Torsemide
In conclusion, torsemide is a commonly prescribed medicine for the remedy of edema related to coronary heart, kidney, or liver failure, as well as different circumstances that lead to extra physique water. By rising the excretion of sodium and water within the urine, torsemide helps to reduce fluid buildup within the physique and alleviate symptoms of edema. While it could have potential unwanted effects, when used as directed and beneath the supervision of a physician, torsemide could be an effective therapy for edema.
As with any treatment, torsemide can have some potential unwanted effects. The most common unwanted effects include dizziness, headache, and dry mouth. It may trigger changes in electrolyte levels, similar to low ranges of potassium, which can lead to muscle weak spot and irregular heart rhythms. Patients with a historical past of kidney or liver illness ought to use warning when taking torsemide, as it might additional impair the functioning of those organs.
Before beginning torsemide, patients should inform their physician of any other medications they are taking, in addition to any allergic reactions or medical circumstances they have. It is essential to observe all directions and precautions given by the prescribing doctor to make sure the safe and efficient use of the medication.
The dosage of torsemide is determined by a doctor and may range relying on the affected person's condition and response to the medication. It is often available as an oral tablet and must be taken with or without food. It is essential to take the medication on the same time every day to maintain up a consistent stage of the drug in the physique. Too high of a dose can result in dehydration and electrolyte imbalance, while too low of a dose may not be efficient in treating edema.
Torsemide works by blocking the reabsorption of sodium and chloride in the kidneys, which outcomes in elevated excretion of these substances in urine. This, in flip, results in increased water excretion, lowering the quantity of fluid in the physique and relieving edema. The medicine is also identified to have a longer duration of motion compared to different loop diuretics, which means it may be taken once a day instead of a quantity of occasions a day.
Torsemide is a medication that is commonly used for the treatment of edema, or swelling, in sufferers with coronary heart, kidney, or liver failure. The treatment can be prescribed for conditions where there could be an extra of body water, such as in certain lung diseases. It belongs to a class of drugs referred to as loop diuretics, which work by rising the quantity of salt and water that's excreted from the physique via the urine.
Edema is a common symptom in patients with heart, kidney, or liver failure. It happens when fluid accumulates within the tissues, causing swelling and discomfort. This can occur due to the physique's incapability to pump blood efficiently, leading to elevated pressure in the blood vessels. In addition, circumstances like cirrhosis of the liver can impair the liver's capability to take away toxins and extra fluids from the physique, leading to edema.
Research substantiating that the use of topical estrogen therapy improves outcomes is lacking heart attack meme torsemide 20 mg order online. Consequently, surgeons should discuss postoperative use of topical estrogens with their patients to determine when to utilize this therapy. Operations in which aseptic conditions are fully maintained: surgical wounds are primarily closed and, if necessary, drained using a closed system. Surgical wounds after nonpenetrating trauma injuries are included in this class if they fulfill the above criteria Surgeries involving opening of the respiratory, digestive, genital, or urinary tracts under controlled conditions and without abnormal contamination. Operations involving biliary tract, appendix, vagina, and oropharynx that exhibit no evidence of infection and where aseptic conditions are fully maintained arc included in this class Fresh (within 7 h of causal event), open trauma injuries. Surgical procedures with a major sterile technique (open heart surgery), or with significant contamination from the gastrointestinal tract. Wounds with acute, nonpurulent inflammation are included in this class Old (more than 7 h after causal event) trauma injuries with devitalized tissue and with preexisting clinical infection or perforated viscera. When suspected, the patient should be taken to the operating room immediately for wound exploration. The incision should be opened and debrided, either mechanically or chemically, and a mass closure with permanent suture should be performed. The complexity of these adverse events led to the publication of a new classification system by the International Urogynecologic Association and the International Continence Society in 2011 (Table 25-4). The committee recommended more specific terms as outlined below in lieu of the generic term erosion. Treatment of mesh complications depends in large part on their timing and their severity. Intraoperative complications, such as cystotomy during retropubic sling placement, can be managed simply by removing and replacing the trocar. It is imperative that the surgeon check for these potential problems after mesh placement as their morbidity, if unrecognized, is significant. At three months, clinical examination confirmed an infected midline 15 mm vaginal mesh exposure together with a rectovaginal fistula. Had this been identified intraoperatively, the mesh could have been removed and the fistula potentially avoided. Suture erosions can usually be treated in clinic by removing the suture and providing vaginal estrogen. However, when conservative management fails or the extrusion is large, a return to the operating room may be necessary to remove the mesh. Vaginal examination revealed a mesh exposure of 20 × 15 mm at the anterior vaginal wall and vaginal cuff that was management by excision and removal in the operating room. Adynamic or paralytic ileus is a mild to moderate ileus and is a normal postoperative event that is expected to follow any intraperitoneal or pelvic operation. Fifteen percent of patients undergoing hysterectomy and 30% who have had bowel resection may suffer this complication. Factors that may predispose or exacerbate postoperative ileus include dehydration, electrolyte abnormalities, bowel manipulation during surgery, retroperitoneal dissection, peritonitis, abscess, and hematoma. There are no clear definitions for prolonged postoperative ileus, but many consider it to be when symptoms continue three to five days after surgery. Clinical findings of adynamic ileus include absence of flatus, abdominal distention, nausea and vomiting, and obstipation. Physical findings of abdominal distention and tympany, reduced bowel sounds, and mild diffuse tenderness are common. The differential diagnosis for prolonged postoperative ileus must include mechanical small bowel obstruction. While both of these conditions may initially be managed conservatively, prolonged small bowel obstruction ultimately requires surgery to prevent intestinal ischemia, necrosis, perforation, and subsequent peritonitis and sepsis. Differentiating these two entities can be difficult, as they share many of the same signs and symptoms (Table 25-5). However, when prolonged postoperative ileus is present, supine and upright plain radiographs are suggested to diagnose and rule out small bowel obstruction. Often times these radiographic findings can be present in patients with both postoperative ileus and small bowel obstruction. Radiograph shows a pattern suggestive of ileus with slightly dilated colon, measuring up to 9 cm on the right in a patient with spinal fixation devices. Upright radiograph shows a distended stomach and slightly dilated loops of small bowel with air-fluid levels, and a paucity of colonic gas, consistent with small bowel obstruction. Postoperative ileus is typically a self-limiting condition that responds to supportive measures. Patients should not be allowed to eat or drink and intravenous fluids should be administered and electrolytes closely monitored. When postoperative ileus is prolonged, the clinician should evaluate the patient for reversible causes and exclude other diagnoses such as obstruction or bowel perforation. Strategies to reduce the incidence and duration of postoperative ileus are listed in Table 25-6. Routine use of nasogastric suctioning, however, is associated with a slower routine of bowel function and trends toward increased pulmonary complications, increased discomfort, and longer hospital stays. The most common cause of obstruction is postoperative adhesion formation and hernia, which cause extrinsic bowel compression. Less common causes include tumors and strictures, which can cause intrinsic obstructions. Similar to postoperative ileus, patients with small bowel obstruction report obstipation, vomiting, and painful abdominal distention.
A small hemostat is inserted into the bladder via the urethra blood pressure monitoring chart template cheap torsemide 10 mg otc, and the proximal end of the catheter is drawn up and out of the patient via the urethra. This usually ensures that the catheter does not interfere with the subsequent fistula closure. Unless the orifice is lying within the line of fistula closure, the catheter should be removed at the end of the repair. The rationale for this step is twofold, in that it is hoped that this injection will reduce blood loss, and the bulking of the tissues may accentuate tissue planes for dissection. Then this incision is carried horizontally on either side out to the lateral wall of the vagina. This incision defines the posterior portion of the dissection, the area where the vaginal mucosa is freed from the base of the bladder. This anatomic region is also home to the major vascular pedicle of the bladder, and therefore it is prudent to direct the dissection along the inner surface of the vagina rather than into this potentially dangerous region. In difficult fistula repair, tissue mobility is a must, so it is a good practice to do a fairly complete posterior dissection, even on relatively small fistula defects. For difficult cases, retractors such as Heaney retractors or a selection of Sims retractors can be of benefit. Yet, as this posterior vaginal flap is developed, it is generally possible to palpate the remnant of the cervix internally, even when nothing is visible per vagina. Once this posterior portion of the vagina has been completely freed from the bladder base, the anterior dissection is next. The remaining anterior vaginal tissue is dissected from the bladder and urethra in much the same way. The most awkward phase of the dissection of the vagina from the bladder is during the initial mobilization of the two halves of the anterior vagina. Because of the fixation of tissue in this area beneath the pubic arch, the surgeon trying to develop the three-dimensional dissection plane will point the dissecting scissors directly back toward his or her own face. The tissue quality in this region can be quite tenuous, and this dissection must be carried out gently and accurately. A few cuts with the tips of the scissors directed back toward the surgeon can free the most troublesome of the dense bony attachments, and soon the remaining flap development is easily done. Once one half of the anterior vagina has been completely freed from the bladder and urethra, the flap can be retracted and held out of the surgical field with a stay suture from the tip of the flap to the skin of the labia majora. However, unless the surgeon is quite experienced, it is probably safer to err on the side of "too much" dissection rather than "too little. When dissection has been done well, the edges of the bladder defect tend to fall together with no tension whatever. There are common fistula variants that require some modification to this dissection scheme. Pinpoint fistulae, especially those near the bladder base, can be easily managed with a cruciate incision, with horizontal and vertical limbs intersecting at the fistula defect. Mobilizing the vagina for 2 to 3 cm in all directions is generally all that is necessary. Multiple fistulae can often be joined together into a single defect, which is then dissected as a single, larger opening. Urethral fistulae require much more careful and limited dissection to avoid damaging anatomic structures involved in continence. Heavily scarred fistulae are difficult to dissect no matter what their anatomic location. One special situation in terms of dissection is the fistula sometimes known as the lungu fistula (lungu is a Hausa word for "around the corner"). These fistulae are lateral defects where the lateral border of the fistula is densely adhered to the pubic arch. Although it may be tempting to repair the fistula without dealing with the attachment to bone, this approach will surely fail. The problem is being able to properly visualize the correct dissection plane between the bladder and the periosteum of the pubic arch. Rather than attacking the problem just at the point of scarring, it can be helpful to try to perforate the endopelvic fascia about 1 cm above and below the fistula. Using these perforations as portals of entry into the space lateral to the bladder, blunt finger dissection can be used to free all but the strongest scar between the bladder and the arch. The surgeon can then place an index finger above and middle finger below the fistula and retract the bladder tissue medially, allowing the final bridge of scar to be divided safely. The fistula must be confirmed "watertight" intraoperatively to achieve successful closure. If there is difficulty in bringing the fistula edges together for closure, the dissection is inadequate and needs to be extended. Some employ interrupted sutures exclusively, while others prefer a running stitch. Some surgeons obsess on folding all of the bladder mucosa inside the bladder, while others insist on everting the mucosa so that mucosa-to-mucosa closure can be visually confirmed. Some surgeons insist on a two- or threelayer closure; others are content with a single layer. Likewise, there are divergent opinions about suture material: 0 versus 2-0 versus 3-0 versus 4-0, braided versus monofilament, and swedged-on versus handthreaded. It seems apparent from the urologic literature that all common absorbable suture materials are roughly equal in their efficacy for bladder wound closure. If any one of the above-listed tenets were truly superior, it would seem that centers employing these techniques would boast superior closure rates. Here again, opinions range across a wide variety of clinical products and practices.
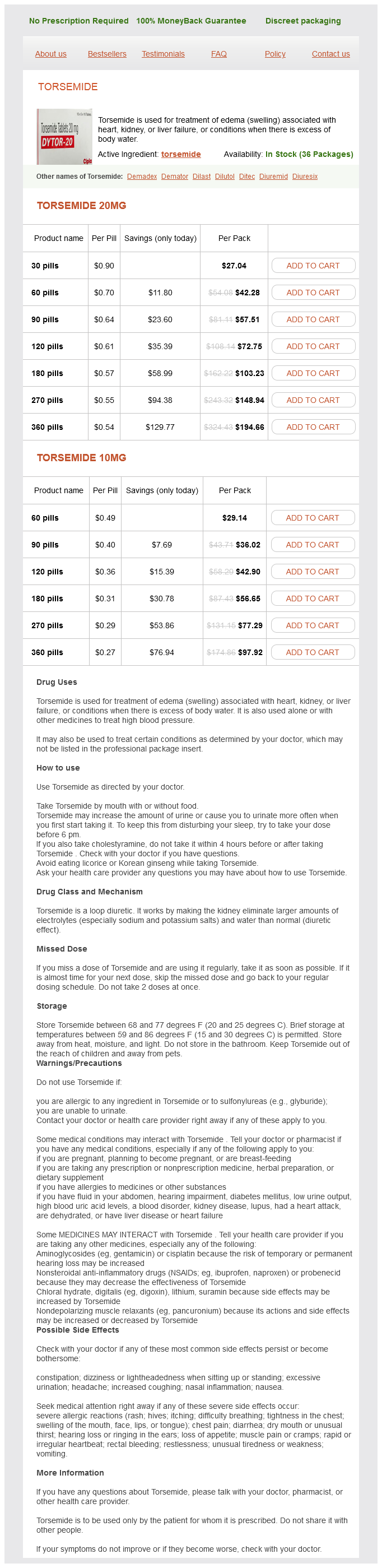
Torsemide Dosage and Price
Torsemide 20mg
- 30 pills - $27.04
- 60 pills - $42.28
- 90 pills - $57.51
- 120 pills - $72.75
- 180 pills - $103.23
- 270 pills - $148.94
- 360 pills - $194.66
Torsemide 10mg
- 60 pills - $29.14
- 90 pills - $36.02
- 120 pills - $42.90
- 180 pills - $56.65
- 270 pills - $77.29
- 360 pills - $97.92
Nonetheless blood pressure chart for senior citizens torsemide 10 mg purchase mastercard, some surgeons, citing practices of other subspecialties, have recommended an early resumption of sexual activity to decrease scarring and prevent vaginal rigidity and dyspareunia. The decision to resume sexual activity should be mutual one between the patient and her partner. A subanalysis of the previous multicenter trial revealed patients who had posterior repair were more likely to report postoperative dyspareunia (28% vs 57%, P =. Levator plication, which was used in the past to augment a posterior repair, has been shown to significantly increase the rate of de novo dyspareunia and should be avoided. The use of mesh during pelvic floor surgery may also adversely affect vaginal caliber. A case series of 17 patients with mesh contraction found that all patients presented with severe vaginal pain and dyspareunia. In addition, mesh erosion (9 of 17), vaginal tightness (7 of 17), and vaginal shortening (5 of 17) were frequently present together. After surgical correction, 88% of women in the previous study had a substantial reduction in vaginal pain and 64% experienced a reduction in dyspareunia. Evacuation of the bladder can be achieved with transurethral and suprapubic catheters as well as intermittent self-catheterization. Bladder Drainage In 1937 Foley described the first self-retaining transurethral catheter. An alternative to transurethral catheterization is suprapubic catheterization, which avoids the high bacterial density of the periurethral region producing lower rates of bacterial infection. These benefits make them ideal for patients who are likely to require catheterization for a longer period time. However, their small caliber makes suprapubic catheters prone to obstruction and necessitates their frequent irrigation. In addition, the invasive method of their insertion can cause rare complications such as cellulites, bowel injury, urine extravasation, and catheter fracture. This approach requires that the patient have the mental and physical capacity to perform self-catheterization. Patients can start selfcatheterization immediately postoperatively or after removal of a Foley catheter. Typically, patients are instructed to empty the bladder every three to four hours and as needed during the night. Intermittent self-catheterization is safe and has lower complication rates than indwelling or suprapubic catheter placement. One commonly used definition is the inability to adequately empty the bladder six weeks postoperatively. It is hypothesized that during anterior repair, inflammation and edema from plication of the vesicovaginal muscularis, especially near the urethrovesical junction, may act to obstruct the urine outflow. Alternatively, patients who have had abdominal surgery may hesitate to contract their abdominal muscles, which can inhibit the voiding reflex. This reflex relies on the generation of sufficient intra-abdominal pressure to trigger the parasympathetic function of the bladder detrusor. Weak Recommendation · Unless otherwise clinically indicated, consider using the smallest bore catheter possible, consistent with good drainage, to minimize bladder neck and urethral trauma · Changing indwelling catheters or drainage bags at routine, fixed intervals is not recommended · Unless obstruction is anticipated (eg, as might occur with bleeding after prostatic or bladder surgery) bladder irrigation is not recommended · Routine irrigation of the bladder with antimicrobials is not recommended · Routine screening of catheterized patients for asymptomatic bacteriuria is not recommended Modified from Ref. Symptomatic urinary tract infections and bacteriuria in patients receiving antibiotics were reduced in a randomized placebo-controlled trial. Removal While drainage of the bladder via catheterization is often necessary after pelvic floor surgery, it should be removed expeditiously. In addition, catheterization is often viewed by patients as one of the more disruptive interventions of the postoperative period. Some authors advocate removal of the catheter when postvoid residual volumes are 20% of the voided volumes. Cleaning the catheter near its origin of insertion with soap and water is adequate for ongoing maintenance. For urethral indwelling catheters, meatal disinfectants or antibacterial lubricants should not be used as they do not prevent infection and may lead to the development of resistant bacteria at the meatus. The collecting system should be emptied regularly, avoiding contact of the drainage spigot with the collection container. Leakage around a transurethral or suprapubic catheter can occur with chronic use (>6 weeks). In patients with neurogenic conditions, using antimuscarinics or partially deflating the balloon may be effective solutions to reduce leakage around the catheter. Sphincteroplasty and Fistula Repair Research on bowel management following sphincteroplasty or fistula repair is sparse. Some physicians recommend a laxative regimen in the early postoperative period to encourage easy passage of soft stool to prevent trauma to the suture line. Others have recommended a bowel confinement technique or constipating regimen to prevent immediate stress on the suture line and pain associated with bowel movements. One randomized trial compared a bowel confinement regimen (a clear liquid diet with loperamide 4 mg by mouth three times per day and codeine phosphate 30 mg by mouth four times per day until the third postoperative day) with a regular diet beginning the day of surgery in patients undergoing anorectal reconstructive surgery. However, the investigators did find a delay in first bowel movement and increased cost in the bowel confinement group. There was no difference in other symptomatic or functional outcomes between the two groups. Surgical management for pelvic floor disorders can be classified as intraperitoneal or extraperitoneal. Vaginal surgery that remains extraperitoneal (eg, retropubic slings, anterior and posterior trocar-guided mesh placement or placement of free grafts) is typically performed as an outpatient procedure without dietary limitations.
© 2025 Adrive Pharma, All Rights Reserved..