General Information about Topamax
Topamax works by inhibiting the activity of sure neurotransmitters, such as glutamate and GABA, which are involved in the transmission of nerve indicators in the brain. By doing so, it helps to stop irregular electrical exercise and the spread of seizures all through the brain.
In addition to epilepsy, Topamax can be permitted for stopping migraine complications in adults. It works by affecting the neurotransmitters answerable for inflicting the blood vessels in the mind to widen, which might set off migraines.
In conclusion, Topamax is a extensively used treatment for treating epilepsy and preventing migraines. It successfully works by lowering abnormal electrical exercise within the brain, and its dosage may vary relying on the patient's situation and age. Like any treatment, it might cause side effects, however these are often mild and may be managed. Overall, Topamax has proven to be a useful treatment possibility for these residing with seizures and migraines.
Topamax, also called topiramate, is a medication used to deal with seizures and forestall migraine headaches. It is categorized as an anticonvulsant or anti-epileptic drug and works by reducing irregular electrical exercise within the brain.
The dosage of Topamax varies depending on the condition being handled and the affected person's age. When used for epilepsy, the beginning dose is normally low and progressively elevated as needed. The recommended beginning dose for adults with epilepsy is 50 mg twice a day, with a maximum dosage of four hundred mg per day. Children are sometimes prescribed a decrease dose, primarily based on their weight.
Like any treatment, Topamax could cause unwanted side effects in some individuals. The commonest unwanted effects reported are tingling sensation in the fingers and toes, fatigue, nausea, and problem with concentration. In uncommon cases, it can trigger extra severe side effects, similar to suicidal ideas, kidney stones, or a lower in sweating.
Topamax is usually thought of secure and effective in controlling seizures and stopping migraines. However, it's not really helpful for pregnant ladies or ladies who are breastfeeding, as it might pose a danger to the fetus or the toddler.
For migraine prevention, the recommended starting dose is 25 mg once a day, increasing to a maximum of 200 mg per day. It is necessary to comply with the dosage guidelines as prescribed by a physician and to not all of a sudden stop taking the medicine with out medical advice, as it could possibly cause withdrawal symptoms.
The use of Topamax for epilepsy was first approved by the US Food and Drug Administration (FDA) in 1996. Since then, it has become a popular therapy choice for both adults and youngsters with epilepsy. It is usually used to treat partial-onset seizures, where seizures start in a single a part of the mind, and first generalized tonic-clonic seizures, which contain the complete brain.
Topamax may also work together with other medications, so it's essential to inform a physician about all medications being taken earlier than beginning this treatment. It can be essential to mention any history of kidney problems, glaucoma, or metabolic disorders, as Topamax can worsen these conditions.
The requirement for increased T4 secretion increases iodine requirements during pregnancy medicine video topamax 200 mg order fast delivery. In addition, maternal iodine intake must be increased to supply the requirements of the fetal thyroid during the second and third trimesters (see Table 11. This series of events is well documented in areas of endemic iodine deficiency or borderline iodine supply, such as Brussels, Belgium. During pregnancy, autoimmunity is suppressed, affecting patients with Graves and Hashimoto diseases (see Chapters 12 and 13). The changes of pregnancy, together with the decreased peripheral vascular resistance, vasodilatation, and modest tachycardia, may suggest thyrotoxicosis (see Table 11. It is important to appreciate that such changes are physiologic in pregnancy, especially when managing the hyperthyroid pregnant patient. This transfer may be significant, given the capacity of the fetal brain to increase the efficiency of T4-to-T3 conversion. Furthermore, T4 can be found in coelomic and amniotic fluids before the onset of thyroid function. Fetal Thyroid Function the peripheral metabolism of T4 in the human fetus differs markedly from that in the adult, both quantitatively and qualitatively. Overall, rates of production and degradation of T4 in terms of units per body mass exceed those in the adult by 10-fold. In addition, D1 catalysis is reduced and D3 is enhanced, favoring the formation of the inactive rT3 at the expense of T3. D3 is highly expressed in fetal tissues, including the liver, skin, tracheobronchial, urothelial, and gastrointestinal epithelia. This change permits the highly regulatable conversion of T4 to T3 by D2 to be the major pathway for generating tissue T3. Maternal-Fetal Interactions the fetal pituitary-thyroid axis functions as a unit that is essentially independent from the mother. In infants with congenital hypothyroidism caused by Thyroid Function in the Newborn Mean total T4 level in cord sera is 150 nmol/L (12 g/dL). In response, the serum T4, T3, and Tg concentrations increase rapidly during the first few hours after delivery and are in the hyperthyroid range by 24 hours of life. All of these issues need to be taken into account when evaluating the thyroid status of the preterm infant, particularly given the increased prevalence of congenital hypothyroidism in this age group. The daily levothyroxine requirement is about 10 g/kg in the newborn, decreasing progressively to about 1. There is a reduction in weight of the gland, in the size of follicles, and in the content of colloid, and there is increased fibrosis, often with marked lymphocytic infiltration. This constellation of findings is termed the low T3 syndrome, the euthyroid sick syndrome, or nonthyroidal illness. During fasting, there is a reduction of 50% or more in serum T3 and an increase in serum rT3 without initial changes in serum total or free T4 (Table 11. The finding of normal T3 plasma levels in mice with the genetic absence of both D1 and D2 enzymes suggests that, under normal conditions, the thyroid gland by itself is able to compensate for impaired peripheral conversion to normalize serum T3. This observation suggests that very powerful mechanisms are in place to maintain serum T3 levels within the normal range, with the notable exceptions of when it is not meant to be in that range. In these circumstances, by a mechanism probably regulated by the hypothalamus, all compensatory mechanisms are reduced and serum T3 may drop to almost undetectable levels. The finding that D3-null mice can still develop the low T3 syndrome suggests that D3 upregulation is not the only event occurring in this clinical state. It is not yet known if such an increase in D3 also occurs during caloric restriction. During fasting, basal oxygen consumption and heart rate decline, and nitrogen balance, initially negative, returns toward normal. Thus the decrease in T3 during fasting (and presumably illness) can be viewed as a beneficial energy-sparing and nitrogen-sparing adaptation. Chronic malnutrition such as occurs in anorexia nervosa is also associated with a reduction in serum T3 and rarely in free T4. In contrast, overfeeding, particularly with carbohydrates, increases T3 production rates and the serum T3 concentration, reduces serum rT3, and increases basal thermogenesis. Thus T4-to-T3 conversion by D1 and D2 is reduced while D3-mediated T3 and T4 inactivation continues. Postmortem studies show that hepatic D1 activity is reduced by about 50%, skeletal muscle D2 is absent, and D3 is present in liver and skeletal muscle. Interestingly, the same global pattern of changes during acute medical illness has been described in patients with primary hypothyroidism receiving levothyroxine. Therapies have been introduced in an attempt to ameliorate certain of the illness-related central abnormalities in the hypothalamic-pituitary axis (including decreases in growth hormone and gonadotropins). Such patients meet all laboratory criteria for primary hypothyroidism with the exception of the clinical context. Despite the severity of the abnormalities, particularly in serum T3, there is still disagreement as to whether therapeutic intervention should be initiated even in the most severely ill patients because most controlled studies have not shown beneficial effects of T4 or T3 supplementation in such individuals. However, treatment of the adrenal insufficiency can lead to complete resolution of these abnormalities, suggesting that in some patients they are a consequence of glucocorticoid deficiency rather than primary thyroid disease. Likewise, patients successfully treated for Cushing disease can develop thyroid autoimmunity. Estrogen also increases the levothyroxine requirement in patients with primary hypothyroidism.
The diagnosis is made by the presence of the classic triad of polyuria medications nursing cheap topamax 200 mg mastercard, hypernatremia, and dilute urine after exclusion of other possibilities such as diabetes mellitus and mannitol therapy. Sometimes diuresis after surgery is the result of water retention during the procedure. Vasopressin is released during surgical procedures and administered fluid is retained. When the stress of surgery abates, the vasopressin level falls and retained fluid is excreted. If an attempt is made to match the urine output with further fluid infusion, persistent polyuria might be mistaken for diabetes insipidus. If in doubt, fluid should be withheld until there is a modest increase in serum sodium. If the urine output decreases and the serum sodium remains normal, the polyuria was due to excretion of physiologically retained fluid. If the serum sodium begins to rise while urine osmolality is low and there is a positive response to administered desmopressin, the diagnosis of diabetes insipidus can be established. Urine output will be reduced in 1 to 2 hours and the duration of effect is 6 to 24 hours. Care should be taken that hypotonic intravenous fluids are not given excessively after administering desmopressin, as the combination can lead to profound hyponatremia. Because a comatose patient must be given fluids parenterally, it is important to monitor serum sodium concentration regularly to check for dilutional hyponatremia. Persistent diabetes insipidus has been demonstrated in prospective studies to be a predictor of fatal outcome after traumatic brain injury, perhaps because it is a manifestation of rising intracranial pressure and imminent herniation. A carefully monitored regimen of a fixed dose of desmopressin to maintain chronic antidiuresis and a prescribed volume of fluid intake is preferable. Treatment of Diabetes Insipidus in Pregnancy Desmopressin is the only therapy recommended for treatment of diabetes insipidus during pregnancy. Desmopressin has 2% to 25% the oxytocic activity of lysine vasopressin or arginine vasopressin193 and can be used with minimal stimulation of the oxytocin receptors in the uterus. Physicians should be cautious about overadministration of fluid parenterally during delivery because these patients will not be able to excrete the fluid and can develop water intoxication and hyponatremia. After delivery, plasma oxytocinase decreases and patients can recover completely or be asymptomatic with regard to fluid intake and urine excretion. Nephrogenic diabetes insipidus does not respond to desmopressin therapy, although occasionally partial defects have limited response to high doses of desmopressin. It has been hypothesized that contraction of extracellular fluid volume, decreased glomerular filtration rate, proximal tubular sodium and water reabsorption, and decreased delivery of fluid to the collecting duct result in a decreased volume of urine. Persistence Adipsic Diabetes Insipidus the combination of attenuated thirst and diabetes insipidus confers high risk of severe hypernatremia. As well, when treated with Chapter 10 Posterior Pituitary 315 of nephrogenic diabetes insipidus can be treated by hydrochlorothiazide and amiloride. Plasma volume contraction produced by thiazide diuretics can decrease lithium excretion and predispose to lithium toxicity. V2 receptor antagonists (vaptans) have been reported to act as pharmacologic chaperones that combine with the misfolded receptor, changing the confirmation to allow maturation and transport to the plasma membrane where vasopressin (in excess of the vaptans) would cause the receptor to be activated. These agonists combine with the mutant receptor trapped in the endoplasmic reticulum and allow maturation of the mutant receptor. Molecular testing of newborns will confirm the need for long-term treatment to avoid complications in the affected children and obviate the need for water deprivation or other testing in unaffected children. Patients who miss their hydrocortisone doses are vulnerable to desmopressin-induced hyponatremia. Hypertonic Encephalopathy Hypertonic encephalopathy is uncommon in diabetes insipidus and is only seen when there is inadequate fluid intake in an adipsic patient or in a patient who is unconscious and not receiving adequate fluid supplementation. Conditions other than diabetes insipidus are more common causes of hypernatremic encephalopathy. The condition is associated with loss of hypotonic fluids by the kidney or the intestines, or from insensible losses; or, it might occur following administration of hypertonic sodium containing fluids or hyperalimentation. Studies indicate that in the brain idiogenic osmoles, mainly polyols, trimethylamines, and amino acids, are generated intracellularly so the degree of cell shrinkage is less than would occur based on the degree of hypernatremia. This asynchrony increases the potential for cerebral edema and worsening of the neurologic condition with overzealous treatment of hypernatremia. In cases where the duration of the hypernatremia is not known, the degree of correction of hypernatremia should not exceed 0. This led to the identification of the first well-described cases of this disorder in 1957226 and the subsequent clinical investigations that resulted in delineation of the essential characteristics of the syndrome. Pharmacologic therapies have been tried but without consistent evidence of success. Diabetes Insipidus in Association With Other Therapeutic Decisions Routine Surgical Procedures In all cases there should be preoperative consultation of the surgeon, the anesthesiologist, and the endocrinologist/nephrologist. For most routine surgical procedures the patient is not unconscious for a sufficiently long period of time to require anything more that administration of the usual dose of desmopressin and careful monitoring of fluids during the surgery to prevent overhydration. Most investigators have used the serum sodium concentration ([Na+]) to determine the clinical incidence of hypoosmolality. When hyponatremia is defined as a serum [Na+] of less than 135 mEq/L, prevalences as high as 15% to 38% have been observed in studies of both acutely and chronically hospitalized patients. Nonetheless, hyponatremia is important clinically because (1) severe hypoosmolality (serum [Na+] levels <120 mEq/L) is associated with substantial morbidity and mortality,232 (2) even relatively mild hypoosmolality can quickly progress to more dangerous levels during the course of therapeutic management of other disorders, (3) overly rapid correction of hyponatremia can itself cause severe neurologic morbidity and mortality,233 and (4) it has been observed that mortality rates are from 3-fold to 60-fold higher in patients with even asymptomatic degrees of hypoosmolality compared to normonatremic patients.
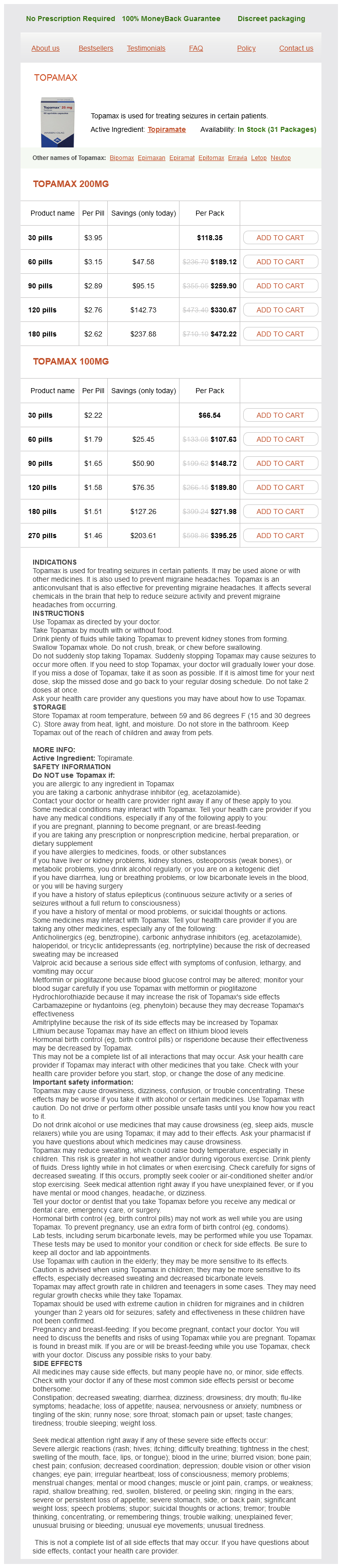
Topamax Dosage and Price
Topamax 200mg
- 30 pills - $118.35
- 60 pills - $189.12
- 90 pills - $259.90
- 120 pills - $330.67
- 180 pills - $472.22
Topamax 100mg
- 30 pills - $66.54
- 60 pills - $107.63
- 90 pills - $148.72
- 120 pills - $189.80
- 180 pills - $271.98
- 270 pills - $395.25
A section of vastus lateralis muscle shows necrotic muscle fibers symptoms 9 dpo buy topamax cheap, some of them invaded by macrophages (arrow). Calcium influx across the defective surface membrane overwhelms mechanisms that maintain a low resting Ca2+ concentration and triggers excessive contraction. The pathologic changes in skeletal muscle (illustration of modified Gomori trichrome stain). These represent overcontracted segments of sarcoplasm situated between degenerated segments. Other fibers are packed with macrophages (myophagocytosis), which remove degenerated sarcoplasm. These fibers have enlarged, vesicular nuclei with prominent nucleoli and represent regenerating fibers. Developing endomysial fibrosis is represented by the deposition of collagen around individual muscle fibers. Pathologically, these diseases resemble other muscular dystrophies, with variable fibrosis and fatty infiltration of muscle. Some affected proteins also cause certain limb-girdle muscular dystrophies, albeit with different mutations. Other extraskeletal manifestations include gastrointestinal dysfunction (from degeneration of smooth muscle) and intellectual impairment. While the clinical presentation of patients with Becker muscular dystrophy is typically milder and of later onset, affected individuals often have exercise intolerance with muscle cramping, occasional rhabdomyolysis and myoglobinuria. Defects in many proteins have been implicated, but these patients show similar clinical features that include pelvic and shoulder girdle weakness. As a result, proper diagnosis requires detailed clinical histories, plus immunohistochemical, immunoblotting and genetic tests. Nucleotide Repeat Syndromes May Cause Muscular Dystrophies Several human genetic diseases are caused by abnormal numbers of intragenic oligonucleotide repeats. Myotonic dystrophy and oculopharyngeal muscular dystrophy are trinucleotide repeat syndromes with very different muscle pathologies. Myotonic Dystrophy Is the Most Common Adult Muscular Dystrophy Myotonic dystrophy is an autosomal dominant disease characterized by slowed muscle relaxation (myotonia), progressive muscle weakness and wasting. Its prevalence is about 14 per 100,000, although minimally affected individuals are hard to diagnose, so this estimate may be low. Congenital Muscular Dystrophies Present in the Perinatal Period these diseases are characterized by hypotonia, weakness and contractures (Table 31-2). Patients develop slowly progressive eyelid ptosis and dysphagia and weakness of other muscle groups including the face and limbs. The autosomal dominant form is prevalent among French Canadians in Quebec and Bukhara Jews (formerly from central Asia), now living in Israel. Biopsies show intranuclear inclusions, rimmed vacuoles and filamentous inclusions similar to those in inclusion body myositis (see below). Normally, there are fewer than 30 copies of this repeat, but in minimally affected myotonic dystrophy patients, there may be 50 or more copies. The greater the number of repeats (sometimes as many as 4000), the more severe the disorder. Necrosis and regeneration, although occasionally present, are not prominent (as they are in Duchenne muscular dystrophy). Muscles in congenital myotonic dystrophy show myofiber atrophy, frequent central nuclei and failure of fiber differentiation. These features closely resemble those of the X-linked recessive type of myotubular myopathy (see below). Life expectancy is usually normal, and extraskeletal involvement includes bundle branch block, hearing loss and retinal vasculopathy. Chronic inflammation is prominent, resembling an inflammatory myopathy such as polymyositis (see below), but does not correlate with the disease course. A detailed clinical history is essential to making the proper diagnosis; otherwise, a patient with muscle weakness and a lymphocytic inflammatory infiltrate could easily be misdiagnosed as suffering from polymyositis. Extraskeletal features sometimes present in myotonic dystrophy include frontal balding, gonadal atrophy, cataracts, personality degeneration and endocrine abnormalities. A few patients exhibit involvement of smooth muscle, with disorders of the gastrointestinal tract, gallbladder and uterus. Many of these children have a difficult perinatal period because of pulmonary complications of weak respiration. Many of the muscle diseases already described are "congenital" in the sense that they are due to mutations present at birth. Many muscle fibers contain a single central nucleus, and most of the affected muscle fibers are abnormally small. These fibers resemble the late myotubular stage of fetal development of skeletal muscle. These people become ambulatory and live a normal life span, although sometimes with secondary skeletal complications of hypotonia such as severe scoliosis. Muscle from these patients rarely reveals distinctive structurally abnormal myofibers. All show congenital hypotonia, decreased deep tendon reflexes, decreased muscle bulk and delayed motor milestones. In all three conditions, abnormal muscle morphology is usually limited to type I fibers, with type I fiber predominance in some disorders and type I hypotrophy in others. There is no active myofiber necrosis or fibrosis, and patients have normal serum creatine kinase.
© 2025 Adrive Pharma, All Rights Reserved..