General Information about Terramycin
As with any antibiotic, there are potential side effects that may happen whereas taking Terramycin. The most common unwanted effects embrace nausea, diarrhea, and skin rash. In some instances, it could also trigger photosensitivity, which is an increased sensitivity to sunlight. It is necessary to take precautions when outdoors, such as wearing sunscreen and protective clothing, to keep away from sunburn. If any severe or persistent unwanted side effects are experienced, you will want to seek medical attention.
One of the principle advantages of using Terramycin is its low danger of causing allergic reactions. Unlike different antibiotics, it is much less prone to trigger an allergic response in people who discover themselves sensitive to penicillin. This makes it an appropriate different for these who are allergic to other antibiotics.
This antibiotic works by inhibiting the growth and replica of bacteria. It does this by interfering with the manufacturing of proteins which may be important for the survival of bacteria. This hinders the bacteria's capability to grow, spread and trigger hurt to the physique. Terramycin is efficient against both gram-positive and gram-negative bacteria, making it a useful remedy for a selection of infections.
There are sure precautions to suppose about when taking Terramycin. It shouldn't be used in youngsters under the age of eight years, as it could trigger discoloration of enamel and have an effect on bone growth. It can also interfere with the effectiveness of oral contraceptives, so an alternate type of contraception ought to be used throughout therapy. Terramycin shouldn't be taken by pregnant or breastfeeding women, as it could harm the developing fetus or be handed to the infant by way of breast milk.
Terramycin, also called oxytetracycline, is an antibiotic used to deal with quite so much of bacterial infections. It is a broad-spectrum antibiotic, that means it's effective towards a variety of micro organism. Originally found in 1949, Terramycin has been an important a half of medical therapy for over 70 years.
Terramycin is commonly used to treat infections in the respiratory tract, skin, and urinary tract. It can also be effective towards certain kinds of sexually transmitted illnesses, similar to chlamydia and syphilis. In some cases, it might even be used to prevent or treat bacterial infections in individuals who have been exposed to others with such infections.
In conclusion, Terramycin is a highly effective antibiotic used to treat varied bacterial infections. Its broad-spectrum nature makes it useful in treating a wide range of infections, and its low threat of allergic reactions makes it an acceptable selection for those who are allergic to different antibiotics. However, like all medicine, it must be taken as prescribed and with warning to keep away from potential unwanted effects. If you think you studied you've a bacterial an infection, consult with your healthcare provider to see if Terramycin will be the proper therapy for you.
Terramycin is available in varied forms, including tablets, ointment, and eye drops. The dosage and period of treatment may vary relying on the severity of the bacterial an infection and the patient's medical historical past. It is necessary to observe the prescribed dosage and finish the entire course of therapy, even if symptoms improve. Stopping therapy early can lead to the re-growth of bacteria and the development of antibiotic resistance.
In the case of the tethered cord antibiotic xifaxan colitis purchase terramycin 250 mg overnight delivery, there may be a Hx of myelomeningocele repair at birth or an overlying cutaneous lesion or mass. Many patients will have some degree of accompanying hydrocephalus, but decisions regarding the placement of ventricular shunts are best postponed until the malformation has been treated, as hydrocephalus may improve with reduction in intracranial venous pressure. Embolization via the arterial or venous system minimizes resistance or reduces flow in the fistula, improving cardiac function. Open microsurgical techniques, endovascular methods, or a combination of both may be used to reduce flow through the malformation. Because of the high mortality associated with treatment by surgery alone and the advances in endovascular techniques, vein of Galen malformations currently are managed without direct primary surgical approaches. Surgery, as an option, is more likely to occur in the setting of staged or attempted embolizations. Subtemporal, midline occipital, or bilateral occipital craniotomies can be used to isolate and occlude arterial feeders to the malformation. Stereotactic radiosurgery has been used successfully as an adjunct to embolization for surgery. Surgical repair is becoming less frequent as interventional radiologists get better at embolization. Patients that present for surgical repair have generally undergone multiple embolizations over months or years. During the procedure hypotension can result in ischemia to the brain (cerebral steal). Hassan T, Nassar M, Eighandour M: Vein of Galen aneurysms: presentation and endovascular management. The ventriculoscope permits direct inspection and limited navigation within the ventricle for both diagnostic and therapeutic purposes and often is most commonly applied in the setting of hydrocephalus. The enlarged ventricles produced by the hydrocephalus contribute to the safety and feasibility of most endoscopic approaches, enabling a variety of procedures. The endoscope can be used to fenestrate multicompartmental periventricular or arachnoid cysts, position ventricular catheters during shunt insertion, biopsy, or, in some cases, resect intraventricular tumors. Neuroendoscopy generally does not help in the initial cannulation of the ventricle (a common misconception). Endoscopic ventriculoscopy may be performed through either frontal or parietal occipital approaches, with the patient typically supine with the neck slightly flexed. A twist drill or burr hole is created and the ventricle cannulated by insertion of the shunt catheter or an introducer with a peel-away sheath (for larger endoscopes). After the ventricle is "tapped" through conventional methods, the endoscope can be inserted and the ventricular anatomy identified. After the intraventricular anatomic landmarks-such as the choroid plexus and/or Foramen of Monroe-are recognized, the scope can be navigated to the site of interest. Smaller endoscopes are used to position the catheter in the optimal ventricular location during shunt placement or revision. Larger endoscopes equipped with channels for instrumentation are used for biopsy, tumor resection, cyst aspiration, or fenestration procedures. Most scope systems have a separate channel for fluid irrigation if minor bleeding or debris obscure visibility. Intraop complications associated with neuroendoscopic procedures include minor or major intraventricular hemorrhage; air entrapment (pneumocephalus); injury to paraventricular structures (basal ganglia, hypothalamus, brain stem); cardiorespiratory depression; and delayed arousal from anesthesia. Intraventricular hemorrhage is caused by direct or indirect injury to ependymal and extraependymal blood vessels. Fortunately, most bleeding encountered is minor but may be sufficient to interfere with visualization and illumination of the ventricle. Third ventriculostomy is one of the more common endoscopic procedures and refers to fenestration of the floor of the 3rd ventricle to create a communication between the 3rd ventricle and the basilar cistern. The technique is most commonly applied to patients with obstructive, or noncommunicating, hydrocephalus, although broader indications are being explored. The fenestration is conducted first by direct visualization of the floor of the 3rd ventricle and then by perforation of the ependymal and arachnoid tissue between the mammillary bodies and the infundibular recess. The perforation can be dilated by inflation of a balloon catheter passed through the fenestration. Because of the proximity to the brain stem-in addition to the complications encountered with ventriculoscopy-3rd ventriculostomy carries the additional risk of mesencephalic injury, hypothalamic dysregulation, cranial nerve injury, and hemorrhage from the basilar artery and adjacent perforating vessels. In the event of excessive bleeding, conversion to an open craniotomy is unlikely to improve control of the hemorrhage. Patients also may be prepped for shunt insertion in the event the ventriculostomy is aborted because of unfavorable 3rd ventricular anatomy. The figure depicts fenestration of the floor of the 3rd ventricle by a blunt probe inserted through the endoscope. Bouras T, Sgouros S: Complications of endoscopic third ventriculostomy: a systematic review. It consists of direct connections between arteries and veins without an interposed capillary network and leads to a tangle of malformed vessels and channels (the nidus), carrying blood at arterial pressure. They may occur in any location of the brain, brain stem, or spinal cord; however, cerebral malformations are the most common. The arterial vessels deliver blood to the veins at systolic blood pressure and that may cause bleeding. The lack of an interposed capillary network prevents local oxygen delivery leading to focal ischemia (steal) and seizures. In addition, venous congestion with arterial pressure blood may produce neurologic symptoms due to venous congestion and reduced perfusion to surrounding brain. It is reported that after a hemorrhage, the risk may be as high as 6% during the subsequent year.
Individuals will also show atrophy of the supraspinatus and infraspinatus muscles antimicrobial journals order 250 mg terramycin mastercard. The supraspinatus is responsible for abduction of the arm and stabilizes the humerus while the infraspinatus is responsible for external rotation of the humerus. Patients with chronic shoulder pain will usually have an accompanied limited range of motion of the shoulder. Athletes specifically will report a decrease in overhead range of motion performance. Plain films of the shoulder are extremely useful to rule out bony abnormalities of the shoulder joint. Evidence Base Chronic Pain Two randomized control trials comparing suprascapular nerve block to intraarticular joint injections for chronic shoulder pain showed that suprascapular nerve block improved pain and function to a greater extent at 12 weeks [6, 7]. Similarly, several other studies showed that suprascapular nerve block was effective in patients with severe rheumatoid arthritis and adhesive capsulitis [8]. Another study comparing an ultrasound technique to landmark-based technique showed that both groups improved significantly initially, but the ultrasound group showed sustained relief at one month with no side effects [10]. Suprascapular pulsed radiofrequency lesioning and cryolesioning can provide relief for 18 months [1113]. The use of chemical neurolysis with phenol is only supported in a few case reports and a single study of rheumatoid arthritis patients; hence its routine use is not recommended at this time [14]. Anatomy the suprascapular nerve is primarily derived from fibers of the brachial plexus from C5 and C6 nerve roots with some contributions from C4. It branches from the superior trunk of the brachial plexus in close proximity to the anterior and posterior divisions. The bundle of nerves travel inferiorly and posteriorly in the posterior triangle of the neck before it forms the suprascapular nerve [3, 1620]. The nerve roots are accompanied by the suprascapular artery and vein until they reach the suprascapular notch. The nerve runs under the coracoclavicular ligament and superior transverse ligament as it makes its way through the suprascapular notch. It then runs underneath the trapezius and the omohyoid as it enters the supraspinatus fossa where it also lies directly under the transverse scapular ligament. In the suprascapular fossa, the nerve gives off motor branches to the supraspinatus and infraspinatus. In addition, sensory branches supply the posterior glenohumeral capsule, acromioclavicular joint, as well as the coracohumeral and coracoclavicular ligaments and subacromial bursa. The main trunk of the nerve leaves the fossa and enters the lateral border of the spine of the scapula through a fibro-osseous tunnel formed by the spinoglenoid ligament and ends in the infraspinatus muscle. Acute Pain Studies comparing interscalene block to a suprascapular block for arthroscopic shoulder surgeries have shown that interscalene block is superior based on pain scores and morphine consumption [15]; however, suprascapular nerve block, especially along with axillary nerve block, could be a good alternate to interscalene block in patients with diminished pulmonary reserve. Suprascapular block does not cover non-arthroscopic surgeries of the shoulder which usually cause pain in the anterior portion of the shoulder, since it is an area not covered by the suprascapular nerve. It also is an ideal target for blockade because the nerve is accessible and has not yet divided into its motor and sensory branches. Physical examination must include a complete evaluation of the shoulder including range of motion, both for pre-procedure assessment and post-procedure success of the block. Medication protocol should be consistent with the American Society of Anesthesiologists conscious sedation guidelines. For treating painful conditions that are mediated by the suprascapular nerve, a total of 80 mg of depot steroid such as methylprednisolone or triamcinolone can be added although there is no good evidence to state that it adds any benefit [3]. Doulatram Blind Technique It is not always possible to ascertain any dermal analgesia as a result of the suprascapular block, although pain relief can be immediate if short-acting local anesthetics are used. With higher concentrations of local anesthetic, a motor block may be apparent when testing the shoulder for abduction of the arm which may be compromised for the first 15 degrees before the deltoid muscle takes over [3]. A direct approach deposits medication in the suprascapular notch, while an indirect approach deposits it in the floor of the supraspinatus fossa. Direct approaches targeting the notch increase the risk of pneumothorax and nerve injury when compared to the indirect approaches. Anterior Approach the needle is inserted between the junction of the medial border of trapezius and posterior border of the lateral third of the clavicle. Posteromedial Approach A line is drawn along the length of the spine of the scapula and divided into three equal parts. The needle is directed toward the scapular notch about 12 cm above this intersection point. Radiographic Technique Direct Approach the spine of the scapula is first identified and marked. A line is drawn vertically at the midpoint of the spine and parallel to the vertebral column. The upper outer quadrant is formed and is bisected, and then a needle is inserted at a distance of 2 cm along the line drawn by the operator. The needle is inserted at a right angle and is then advanced until the dorsal surface of the scapula is located. The needle is then "walked along" the dorsal surface until the suprascapular notch is identified or the needle is "walked off. If a nerve stimulator is used, contractions of the supraspinatus and infraspinatus muscles will confirm placement at which point the combination of local anesthetic and steroid is injected. Keeping the hand on the contralateral shoulder increases the distance toward the thoracic cavity and minimizes the risk of pneumothorax [17]. The patient is placed in prone position on the radiology table with arms to the side. The C-arm is angled away from the side of the proposed block in a cephalocaudal direction.
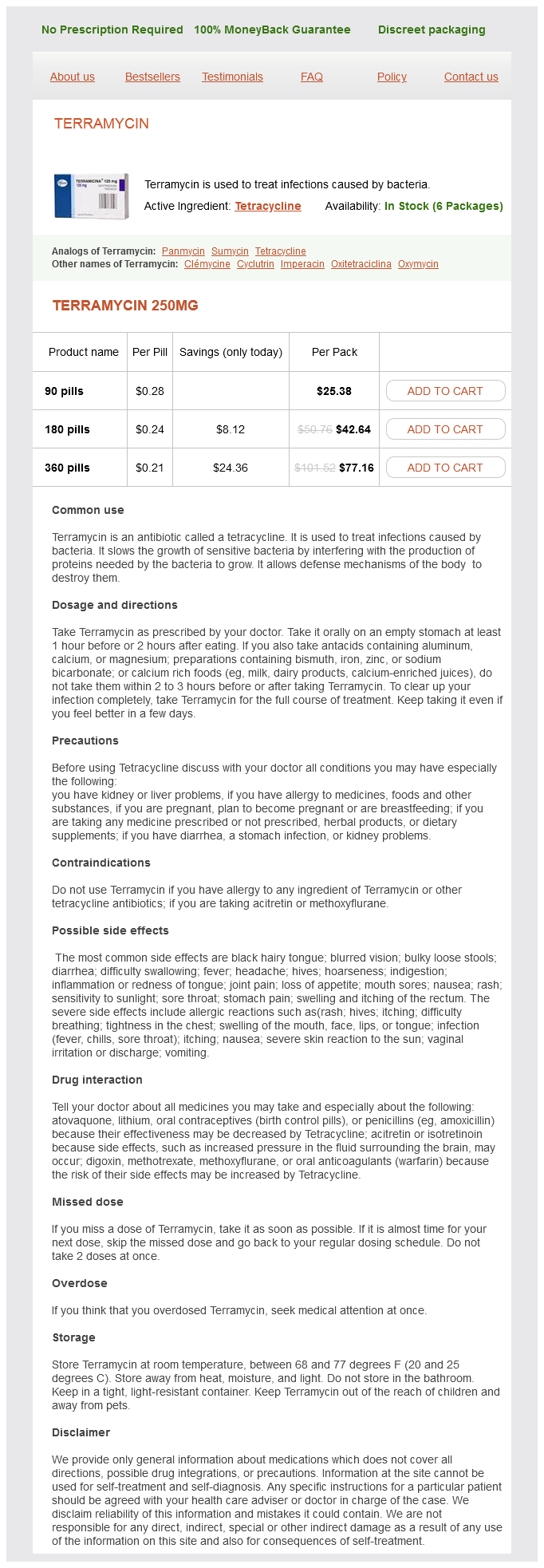
Terramycin Dosage and Price
Terramycin 250mg
- 90 pills - $25.38
- 180 pills - $42.64
- 360 pills - $77.16
Local anesthesia is acceptable for simple herniorrhaphy bacteria kingdom characteristics terramycin 250 mg line, although discomfort may be elicited if the peritoneum is manipulated. Most inguinal procedures are done on an outpatient basis, and the anesthetic should be planned appropriately. Castorina S, Luca T, Privitera G, El-Bernawi H: An evidence-based approach for laparoscopic inguinal hernia repair: lessons learned from over 1,000 repairs. If the tumor can be resected with a safe margin of at least 2 cm, partial penectomy is usually enough. A tourniquet is placed at the base of the penis, which is amputated at least 2 cm proximal to the tumor. The corpora cavernosa are sutured, and the tourniquet is released, followed by inspection for bleeding. The edges of the urethra are sutured to the ventral skin, and the lateral and dorsal skin edges are approximated over the ends of the corpora cavernosa. Usual preop diagnosis: Squamous cell carcinoma of the penile skin Insertion of penile prosthesis is performed for impotence. Sacral anesthesia (saddle block) is sufficient; lumbar epidural anesthesia may be less reliable than spinal or caudal at blocking sacral fibers. Usual preop diagnosis: Metastatic prostate cancer Vasovasostomy is the reestablishment of the continuity of the vas deferens and restoration of fertility following a previously performed vasectomy. The site of previous vasectomy is identified and excised and the two ends of the vas deferens anastomosed. It is bilateral and requires the use of either the operating microscope or magnifying loupes. Usual preop diagnosis: Infertility 2° vasectomy Hydrocelectomy: the testis, with the surrounding hydrocele. The wall of the hydrocele is excised and the edges sutured around the epididymis to prevent recurrence. Variant procedure or approach: Aspiration used as a temporizing approach because recurrence is almost 100%. Usual preop diagnosis: Hydrocele Spermatocelectomy: A spermatocele is a cyst of the epididymis, usually excised with the part of the epididymis from which it arises. Variant procedure: Aspiration as a temporizing maneuver until the operation can be performed. Usual preop diagnosis: Spermatocele or epididymal cyst Insertion of testicular prosthesis: A small incision is made in the scrotal skin, and a pouch is created by blunt dissection in dartos fascia. The prosthesis is placed in the pouch and fixed to the dartos fascia to prevent prosthesis migration. Usual preop diagnosis: Absent testis, either congenital or following orchiectomy Reduction of testicular torsion is an emergency operation that must be performed within 6 h of occurrence to prevent irreversible ischemic damage to the testis. Through a small scrotal incision, the testis is reduced and fixed to the dartos fascia to prevent retorsion. Many of these procedures are done on an outpatient basis, and the anesthetic should be appropriately planned to facilitate early discharge. A transverse or longitudinal perineal incision is made and carried down to the urethra, which is dissected free from surrounding tissues. The strictured area is excised and end-to-end anastomosis is performed over a catheter. Repair of a long urethral stricture may require placement of a patch from the scrotum, foreskin, or buccal mucosa. Variant procedure: Transurethral incision and dilation, which is associated with a 3050% recurrence rate. Usual preop diagnosis: Urethral stricture, usually posttraumatic Urethrectomy: Partial or total urethrectomy is done through a longitudinal perineal incision. The urethra is dissected free of surrounding tissues and followed proximally and distally from the membranous urethra to the external urethral meatus. In total urethrectomy, a tubularized skin graft is interposed between membranous urethra and perineal skin. Usual preop diagnosis: Urethral carcinoma Insertion of artificial urinary sphincter, performed for incontinence, consists of a perineal incision, through which a cuff is inserted around the bulbar urethra. A suprapubic incision is made to place the reservoir and pump, which inflates and deflates the cuff. Usual preop diagnosis: Urinary incontinence Transperineal prostate seed implantation (brachytherapy): High doses of radiation can be delivered to the prostate by implanting radioactive seeds directly into the prostate gland. Using a transrectal ultrasound probe, radioactive seeds (iodine 125 or palladium 103) are implanted into the prostate. The patient is placed in lithotomy position, and a rectal ultrasound probe, with a perineal grid attached, is introduced to image the prostate. This procedure is done by a combined team of radiation oncologists and urologists. Lumbar epidural anesthesia may be less reliable at providing sacral anesthesia and offers no advantages over the above techniques for shorter procedures, although caudal anesthesia may be an acceptable alternative. They include the following: Repair of vesicovaginal fistulas: the vaginal approach is usually recommended for small and distally located vesicovaginal fistulas; otherwise, a transabdominal repair is performed (see Open Bladder Operations, p. An incision is made in the anterior vaginal wall around the fistula, which is excised. Bladder and vaginal walls are separated and closed with interposition of tissues or flaps to separate the incisions and prevent recurrence.
© 2025 Adrive Pharma, All Rights Reserved..