General Information about Terbinafine
In addition to treating tinea versicolor, terbinafine has additionally been found to be effective in treating different kinds of fungal infections such as athlete's foot, jock itch, and ringworm. These infections occur when fungi invade the top layer of the skin, inflicting it to turn out to be purple, itchy, and inflamed. By destroying the fungal cells, terbinafine might help to clear up these infections and supply reduction from uncomfortable signs.
Terbinafine, marketed underneath the model name Lamisil, is an anti-fungal antibiotic that is generally used to treat fungal infections. It is primarily used to deal with tinea versicolor, a standard pores and skin an infection attributable to yeast, however can be effective in opposition to other kinds of fungal infections.
In conclusion, terbinafine is an efficient treatment for treating fungal infections, notably tinea versicolor. With its ability to inhibit the growth of fungi and clear up pores and skin infections, it has turn into a preferred alternative for both medical doctors and sufferers. However, it's important to use this treatment as directed by a healthcare professional and to listen to any potential side effects. If you would possibly be experiencing signs of a fungal an infection, seek the assistance of with your doctor to determine if terbinafine may be the right remedy possibility for you.
Tinea versicolor, also recognized as pityriasis versicolor, is a skin an infection that's brought on by the yeast Malassezia furfur. This fungus is of course discovered on healthy skin, but in some circumstances, it can overgrow and trigger discolored patches on the pores and skin. These patches may be lighter or darker than the encompassing skin and may be accompanied by gentle itching. Tinea versicolor is extra frequent in warm and humid climates and might have an result on individuals of any age, but is mostly seen in adolescents and younger adults.
Lamisil is available as both an oral medicine and a topical cream. The oral kind is commonly prescribed for tinea versicolor, as it might possibly successfully attain the deeper layers of the pores and skin where the fungus may be current. It is taken as quickly as a day for a interval of two to four weeks, relying on the severity of the an infection. The topical cream is often prescribed for milder instances or as a upkeep therapy to forestall future outbreaks. It is applied directly to the affected areas a couple of times a day, relying on the instructions offered by the doctor.
It is crucial to notice that while terbinafine is efficient against fungal infections, it doesn't have any impact on bacterial or viral infections. Therefore, it should not be used to deal with situations corresponding to colds or the flu. It is also not beneficial to be used in pregnant or breastfeeding ladies, as the consequences on the unborn youngster usually are not fully understood.
Terbinafine is mostly well-tolerated, and most of the people expertise few side effects. The most typical unwanted effects that have been reported embody rash, itching, and gastrointestinal points such as nausea and diarrhea. Rarely, more severe side effects such as liver harm have been reported, so it may be very important observe the prescribed dosage and monitor any changes in your well being whereas taking terbinafine.
Terbinafine works by inhibiting the growth of the fungus answerable for the an infection. It does this by interfering with the production of ergosterol, an important component of fungal cell membranes. Without ergosterol, the fungal cells are weakened and finally die, allowing the infection to clear up.
Still under investigation are whether this is an effective approach antifungal body powder order terbinafine once a day, how and when to apply angiogenic agents, and the possible side effects of angiogenic stimulants. Long-term studies are necessary to definitively exclude adverse consequences such as tumor promotion. In contrast, vasculogenesis is the creation of blood vessels de novo by differentiation of new blood cells. Endothelial cell precursors in the bone marrow and circulating in the bloodstream can incorporate into developing vessels and contribute to vessel growth in a manner very similar to the vasculogenesis of embryonic development. The therapeutic potential of these cells has not been tested, but they can be recruited from bone marrow and may be a means to accelerate endogenous revascularization in patients with ischemia. In contrast to angiogenesis, arteriogenesis is the recruitment of existing vessels to increase their capacity and consequent blood flow to ischemic tissue. Most collateral vessels visualized by arteriography are probably vessels that have undergone arteriogenesis instead of angiogenesis. Because arteriogenesis creates capacitance vessels, this process is more likely to increase blood supply in a way that substantially affects tissue perfusion. The therapeutic potential of arteriogenesis has not been tested, but given the role of arteriogenesis in collateral formation in patients with chronic myocardial ischemia, this represents another potential therapeutic tool for the creation of new blood vessels in patients with refractory angina. Treatments designed to enhance blood vessel growth are being tested on patients with otherwise refractory disease, but eventually these approaches could be applied to any patient with ischemic heart disease and could even obviate the need for revascularization procedures in a significant cohort of patients. This review provides a broad overview of the role of angiogenesis in a variety of physiologic and pathologic processes, including cardiovascular diseases. Summarizes potential roles for targeting angiogenesis therapeutically to treat or prevent complications of atherosclerosis. The creation of new blood vessels to increase tissue perfusion is one way to alleviate myocardial ischemia. The challenge is to determine the best way to increase tissue perfusion with minimal side effects. Atherosclerotic plaque progression and vulnerability: angiogenesis as a source of intraplaque hemorrhage. This review discusses the specific role of intraplaque angiogenesis in plaque destabilization via its effect on enhancing hemorrhage within atherosclerotic lesions, and the potential adverse consequences of enhancing angiogenesis as a therapeutic strategy for cardiovascular diseases. Morphologic changes that narrow the vessel lumen (stenosis) or abnormally enlarge its diameter (aneurysms) cause alterations in flow patterns, thereby leading to ischemic symptoms. The imaging method of choice depends upon the vessels in question and the end organs and tissue that are affected. This chapter summarizes the various diagnostic techniques available to evaluate the most commonly encountered occlusive and aneurysmal clinical disorders of the aorta and renal, carotid, and lower and upper extremity arteries. Symptoms range from mild, intermittent claudication (pain or discomfort that develops during exercise and is relieved with rest) to constant, severe rest pain. In these individuals, the femoral artery pulses are usually abnormal, diminished, or absent. Superficial femoral and popliteal artery stenoses result in foot and calf symptoms. Cross referral between cardiology and vascular surgeryinterventional radiology services is vital to identify patients at risk for treatable coronary disease. By far the most common etiology is atherosclerotic plaque formation in the vessel wall leading to luminal narrowing, wall calcification, plaque destabilization and hemorrhage with rupture, thrombosis, and end-organ damage or showering of emboli distally with resulting tissue damage and necrosis. In other circumstances, atherosclerosis leads to weakening of the vessel lumen leading to true aneurysms, defined as a vessel diameter greater than 1. Genetic abnormalities and environmental exposures are almost always contributory in individuals with advanced vascular pathology. Extrinsic mass effects or vessel encasement in the case of popliteal artery entrapment by the gastrocnemius muscle, celiac artery by the diaphragmatic crus (median arcuate ligament syndrome), or renal artery by neurofibromatosis may lead to similar occlusive symptoms. Clinical manifestations depend on the location and severity of the vessel disease and presence of collateral circulation (see Chapter 44 for additional information on the pathogenesis of atherosclerosis). Diagnostic Approach Examinations used to evaluate the lower extremity arteries are designed to establish the presence and location of disease, quantify severity, and determine temporal progression. This examination has a high positive predictive value except in diabetics with noncompressible calcified vessels. The decreased blood pressure can be quantified and localized using pneumatic cuffs and either continuous Doppler or plethysmographic sensors. Pulsatility index derived by dividing the peak-to-peak frequency by mean forward frequency. A Duplex ultrasound of the left popliteal artery (at knee level) beyond the occluded superficial femoral artery. Note the colorflow pattern at baseline (A) and after left femoropopliteal bypass grafting (B). B Characteristics of stenotic arterial examination Laminar flow proximal to stenosis Frequency Waveform distal to severe arterial stenosis Flattened forward flow peak 0 Absence of Time reverse flow Doppler waveform becomes monophasic in severe arterial stenosis, with loss of reverse flow component and decreased systolic acceleration of forward flow (waveform "broadening"). Pressure measurements at multiple levels along the leg can estimate the location of an arterial occlusion. Blood pressure cuffs are placed on the upper and lower thighs and calves, and a gradient of greater than 10 to 15 mm Hg between adjacent sites suggests a physiologically significant stenosis. Measurements after treadmill exercise may disclose a hemodynamically significant lesion that is unapparent at rest. A change in the flow velocity waveform-an increase in peak systolic velocity at the site of the lesion, turbulence, loss of the reverse flow component, or a decrease in pulse velocity distal to the lesion-is diagnostic of a flow-limiting arterial lesion.
The former is due to a decrease in protein binding anti fungal uti cheap terbinafine 250 mg overnight delivery, and the latter is due to an increased tissue binding. This is seen in patients with renal failure, owing to decreased albumin and impaired binding capacity of albumin. The extraction ratio and the clearance rate are measures of the efficiency of the device. A high clearance rate is necessary but not sufficient for effective removal of a drug. This movement takes time, and with rapid removal of the drug from the vascular space, the pseudoequilibrium will be disturbed as the substance is removed from the vascular space faster than it can be replaced from extracellular and cellular stores. With discontinuation of the extracorporeal elimination, there will be a rebound in the concentration as the movement into the vascular space catches up. A report of a significant drop in concentration of a drug with therapy may just represent a disruption in the pseudoequilibrium between the intravascular space and the tissues. The important data is the fraction of the total drug burden removed and is best determined by measuring the drug in the effluent. Although hemodialysis is effective at removing lithium in intoxication, the rebound can be significant following termination of the therapy and repeated treatments with hemodialysis or the use of a continuous therapy may be necessary. The actual removal of digoxin is even less because of the slow equilibration of digoxin from tissue stores. The compound must equilibrate quickly from tissue stores to the vascular compartment. As discussed earlier, the clearance rate is determined by a combination of drug and device characteristics. Device-Related Factors In addition to drug or toxin characteristics, the effectiveness of the extracorporeal removal is also determined by the properties of the extracorporeal device. A high flux membrane is more permeable to middle molecules and allows for clearance of toxins with higher molecular weights. Most dialysis membranes in use today are high efficiency and high flux and therefore maximize the clearance rate of small and middle molecular weight compounds. Characteristics of the individual patient: does the patient have impaired endogenous clearance of the toxin. Characteristic of the compound: What are the toxic effects of the substance ingested, are there antidotes available, and are the adverse effects likely to be severe, permanent, or life-threatening Characteristic of the ingestion: Was it a toxic dose, what is the plasma concentration, how is the level changing with time, and is it likely to go up over time or fail to fall Extracorporeal elimination that increases the total body clearance by 30% or more is believed to be a worthwhile intervention in the proper clinical setting. The ingestion is likely to cause severe morbidity or mortality, and the removal of the drug from the serum will lessen this risk. In some intoxications the effect is too rapid and irreversible for extracorporeal removal to help. The extracorporeal therapy will add significantly to the total body elimination of the drug (>30%). In this case, the device must have a high Cl for the compound and the compound must be mostly in the vascular space. In some cases, this condition might be met partly because of a decreased endogenous clearance in the patient in question. A patient with lithium toxicity may be more likely to benefit from hemodialysis when there is impaired renal clearance because of heart failure or liver or kidney disease. Those for which there is some consensus regarding effectiveness of extracorporeal therapy are listed in Table 51-4 with their important characteristics. Peritoneal Dialysis Properties Clearance rates for peritoneal dialysis are significantly less than for hemodialysis and are rarely adequate to obtain significant toxin removal. Most small molecules will cross the membrane close to their concentration in the serum. The sieving coefficient (S) is the ratio of the concentration in the ultrafiltrate to that in the serum. S ¼ Cðf Þ=CðpÞ Where C(f) is concentration in ultrafiltrate and C(p) is concentration in plasma. The sieving coefficient is usually close to 1 for small, nonprotein-bound molecules. The Cl is proportional to the sieving coefficient and the ultrafiltration rate: Clearance rate ¼ ultrafiltration rate  sieving coefficient Thus toxin removal depends on high rates of ultrafiltration. The extraction ratio for most toxins approaches 1, and the Cl is therefore mostly determined by the Q b. To estimate the concentration of the agent listed, the osmolar gap divided by 10 is multiplied by the factor listed in the table for the specific alcohol. It is important to remember that a low gap does not always imply a low risk of intoxication. First, the gap will underestimate serum levels in some people who start out with a low serum osmolarity. It is recommended that k is estimated at 80% of the manufacturer defined urea clearance rate to avoid overstating achievable clearances. Toxins in which hemodialysis is likely more effective include ethanol, methanol, ethylene glycol, isopropyl alcohol, salicylates, and lithium. Other drugs such as theophylline, phenytoin, carbamazepine, valproic acid, and phenobarbital have a higher degree of protein binding and may benefit from hemoperfusion compared with hemodialysis. They all have low molecular weights, are hydrophilic, have small Vd, and rapidly equilibrate with the intravascular space. Ethanol toxicity usually does not require hemodialysis because most patients will recover with supportive measures alone. An increase in the osmolar gap of 10 mOsm/L would be expected to be caused by a concentration of the drug listed in the table.
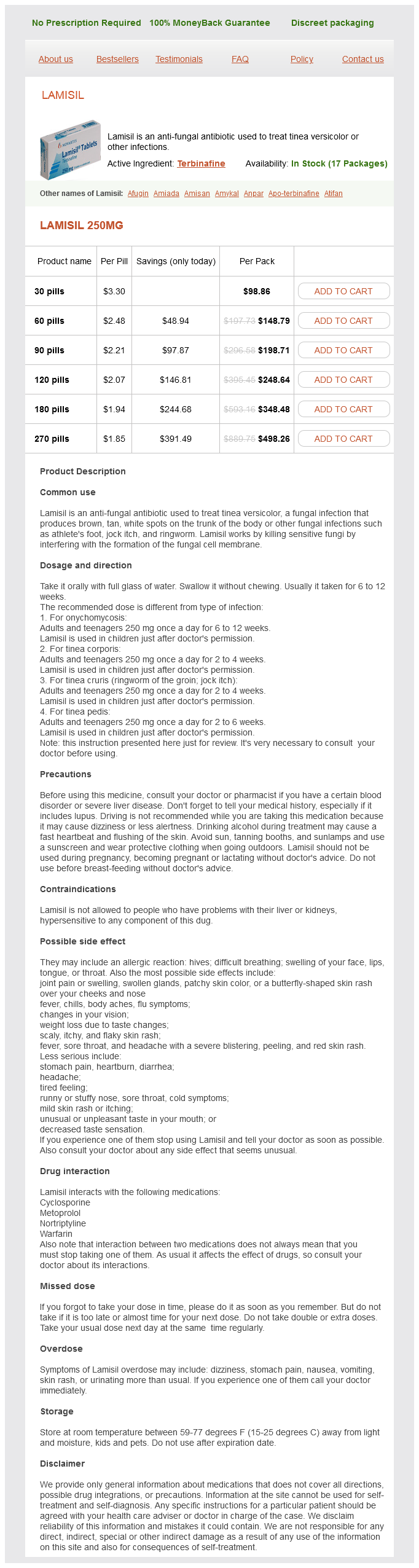
Terbinafine Dosage and Price
Lamisil 250mg
- 30 pills - $98.86
- 60 pills - $148.79
- 90 pills - $198.71
- 120 pills - $248.64
- 180 pills - $348.48
- 270 pills - $498.26
In these cases antifungal uk discount terbinafine 250 mg with visa, the same preoperative and postoperative principles as hernia repair apply. Abdominal Wall Edema Similar to genital edema, abdominal wall edema is usually a complication of a late dialysate leak. The incidence of abdominal wall edema is not well-defined in the literature; however, it is believed to occur less frequently than hernias. Abdominal wall edema may be difficult to detect clinically because it may present with nonspecific signs and symptoms. These include diminished effluent returns and weight gain because of dialysate accumulating in tissues of the abdominal wall. Other presenting features include abdominal asymmetry or increased abdominal girth. Patients with suspected abdominal wall edema should be examined while standing to better detect any abdominal asymmetry. Inspection of the abdomen may reveal it to look pale and boggy with indentations made by the waistband of underpants or the catheter itself. Investigating abdominal wall edema uses the same imaging studies as for genital wall edema. Again, it is important to let the patient ambulate for at least 2 hours after the instillation of the dye/isotope to facilitate its movement into the abdominal wall. The principles of management of abdominal wall edema are similar to those of genital edema (see previous discussion). Should this fail to occur, surgical intervention to close the defect is the risk factors for the development of leaks are similar to those for hernia development. However, early leaks can be the result of not placing a secure purse-string sutures around the deep cuff of the catheter. Along with dialysate, bowel can also migrate along the processus vaginalis into the scrotum, leading to a concurrent and often occult indirect inguinal hernia. The diagnosis of genital edema is usually obvious as it is quite painful and distressing for the patient. That being said, it is important to rule out other processes that may lead to local inflammation, particularly in males, such as epididymitis. Sometimes, the patient may misinterpret the development of genital edema as indicative of general fluid overload and attempt to ultrafilter more fluid. They may complain of diminished effluent return, which in this case is the result of ongoing dialysate leak. The subsequent scan, if positive, will show the movement of dialysate through a patent processus vaginalis or abdominal wall defect into the scrotum or labia. The risk factors for this condition are similar to those of hernia and have been highlighted previously. Typically pericatheter leaks are clinically obvious, presenting as wetness around the catheter exit site, or wetness of the exit-site dressing. If this fails to abrogate the leak, then the catheter should be removed and reinserted at a different site. The source of the leak is where the catheter exits the peritoneal cavity, so exit-site stitches will only mask the problem. While dialysate leak at the exit site increases the risk of peritonitis or tunnel infection, the use of prophylactic antibiotics is usually not warranted unless there are signs of obvious infection. It has been speculated that two factors, possibly occurring concurrently, may be involved in hydrothorax development. These are 1) diaphragmatic defects combined with a large pleuroperitoneal pressure gradient and 2) abnormalities in lymphatic drainage. Diaphragmatic Defects Combined with a Pleuroperitoneal Gradient To allow the flux of dialysis fluid from the peritoneal cavity into the pleural space, a defect in the diaphragm, acting as a source of communication between the two spaces, must be present. However, it is not enough to have a defect; a pressure gradient must also exist between the two compartments to create a driving force for the movement of fluid. Fluid will continue to move into the pleural space until there is equalization of pressure between the two compartments or there is an impediment to further movement. It has been postulated that a valvelike defect in the diaphragm or the action of the hepatic capsule to tamponade backflow of dialysate from the pleural to peritoneal space may be such impediments. The nature of the underlying defect may explain why some individuals develop hydrothorax with their first-ever infusion of dialysis fluid. Prevention of Dialysate Leaks Preventive strategies to reduce the incidence of dialysate leaks have not been formally studied. Steroid use should be minimized and sirolimus discontinued before catheter insertion. Autopsy studies have revealed localized absence of muscle fibers in the hemidiaphragm, which are replaced with a disordered network of collagen. Moreover, when hydrothorax has been investigated by surgery, "blisters" or "blebs" have sometimes been noted on the pleural surface of the diaphragm. While plausible, this mechanism cannot explain all cases of hydrothorax formation. Therefore, abnormalities in phrenic lymphatic drainage likely play a contributing rather than causal role in hydrothorax formation. Other reported symptoms include pleuritic chest pain, diminished effluent volume, hypotension, and even weight gain as a result of decreased ultrafiltration. Sometimes patients may complain of worsening dyspnea despite using more hypertonic dialysate exchanges.
© 2025 Adrive Pharma, All Rights Reserved..