General Information about Tenormin
Like any treatment, Tenormin may trigger unwanted effects in some individuals. Common unwanted effects could embody dizziness, lightheadedness, fatigue, and nausea. These normally subside because the body adjusts to the medicine. However, if the unwanted effects persist or turn out to be extreme, it is necessary to inform the doctor.
Aside from managing high blood pressure, Tenormin can be prescribed to cut back the heart price in cases of tachycardia (rapid coronary heart rate) and atrial fibrillation (irregular heartbeat). By blocking the beta receptors within the coronary heart, the medication helps slow down the center price and enhance its regularity. This may be useful for people with heart situations or those who experience episodes of speedy or irregular heartbeats.
Tenormin comes in pill type and is often taken a few times a day, relying on the power prescribed by the physician. It is necessary to take the medicine as directed and never skip or miss doses, as this will affect its effectiveness. It is also advisable to verify blood pressure and heart fee regularly while taking Tenormin to observe its results.
Another condition that Tenormin is used to deal with is angina, which is chest ache caused by reduced blood move to the heart muscle. Angina may occur when the heart muscle doesn't obtain enough oxygen-rich blood as a result of narrowed or blocked arteries. Tenormin helps to chill out and widen the blood vessels, allowing more oxygen-rich blood to reach the guts, thereby reducing the frequency and severity of angina episodes.
High blood strain, or hypertension, is a common situation that affects approximately one-third of adults worldwide. It is also identified as the 'silent killer' because it could haven't any symptoms and go undetected for years, but can result in severe health problems similar to coronary heart attack, stroke, and coronary heart failure. Tenormin is used to treat hypertension by enjoyable the blood vessels, allowing blood to circulate more easily and reducing the strain on the guts.
Tenormin, also known by its generic name atenolol, is a generally prescribed medicine for the treatment of hypertension, reduction of heart rate, and angina. It belongs to a class of medication known as beta blockers, which work by blocking the effects of adrenaline on the physique's beta receptors. This results in a decrease within the workload of the heart, resulting in a discount in blood strain and coronary heart fee.
In some instances, Tenormin may not be suitable for people with certain medical situations, such as asthma, diabetes, and heart issues. It is essential to inform the physician of any pre-existing situations or drugs being taken before beginning Tenormin.
In conclusion, Tenormin is a broadly prescribed beta blocker for the therapy of hypertension, reduction of coronary heart fee, and administration of angina. It works by blocking the effects of adrenaline on the physique's beta receptors, resulting in a decrease in blood stress and coronary heart fee. While typically considered a secure and effective treatment, it's essential to observe the doctor's instructions and often monitor blood stress and heart price whereas taking Tenormin.
Nonlinear regression is used to fit a monoexponential blood pressure medication classifications purchase tenormin online now, biexponential, or triexponential curve to the resulting concentration-versus-time data. An algebraic relationship exists between the exponential decay curves and a one-, two-, or three-compartment pharmacokinetic model. The fundamental parameters of the compartment model are the volumes of distribution (central, rapidly equilibrating, and slowly equilibrating peripheral volumes) and clearances (systemic, rapid, and slow intercompartment). The central compartment (V1) represents a distribution volume and includes the rapidly mixing portion of the blood and first-pass pulmonary uptake. The peripheral compartments are made up of tissues and organs that show a time course and extent of drug accumulation (or dissipation) different from that of the central compartment. In the threecompartment model, the two peripheral compartments may roughly correspond to splanchnic and muscle tissues (rapidly equilibrating) and fat stores (slowly equilibrating). The sum of the compartment volumes is the apparent volume of distribution at steady state (Vdss) and is the proportionality constant relating the plasma drug concentration at steady state to the total amount of drug in the body. The intercompartment rate constants (k12, k21, and so on) describe the movement of drug between the central and peripheral compartments. The elimination rate constant (k10) encompasses processes acting through biotransformation or elimination that irreversibly removes drug from the central compartment. I, Dosing scheme as a function of time; k10, rate constant reflecting all processes acting to remove drug irreversibly from the central compartment; k, intercompartment rate constants; V1, central compartment volume, usually expressed in liters or liters per kilogram. Despite their physiologic flavor, compartment models are simply mathematic transformations of the polyexponential disposition functions computed from observed plasma concentrations. Thus physiologic interpretation of volumes and clearances (with the possible exception of systemic clearance and Vdss [the algebraic sum of the volumes]) is entirely speculative. The last reason behind the popularity of these models is that they can be used to design infusion regimens. In the usual pharmacokinetic study, I(t) is known, the dose that is given the patient, and C(t) is measured, the concentrations over time. Deconvolution is similar to division, but of functions rather than simple numbers. Unfortunately, such a solution might require some negative infusion rates, which are obviously impossible. It assumes that after a bolus injection there is complete mixing within the central compartment such that the peak concentration occurs precisely at time 0. It actually takes approximately 30 to 45 seconds for the drug to make its transit from the venous injection site to the arterial circulation. The equilibration rate constants between the central and peripheral compartments were calculated using the following equations: k12 = Cl2 ÷ V1, k21 = Cl2 ÷ V2. The elimination rate constant was calculated using the following equation: k10 = Cl1 ÷ V1. Cl1, Clearance of central compartment; Cl2, clearance of peripheral compartment; V1, distribution volume of central compartment; V2, distribution volume of peripheral compartment. Early phase pharmacokinetics but not pharmacodynamics are influenced by propofol infusion rate. For most drugs used in anesthesia, the plasma is not the biophase and thus even after the drug has reached the arterial circulation, a further delay occurs before a therapeutic effect is observed. The reason is that additional time is required for the drug to be transported to the target organ, penetrate the tissue, bind to a receptor, and induce intercellular processes that ultimately lead to the onset of drug effect. This delay between peak plasma concentration and peak concentration at the effect site is called hysteresis. The time course of the plasma concentration and effect-site concentration are simulated using pharmacokinetic and pharmacodynamic models. The plasma concentration versus effect curve forms a counterclockwise hysteresis loop. This loop represents the plasma concentration, which is not the site of drug effect. Using nonlinear mixed-effect modeling, the hysteresis is minimized to reveal the effect-site concentration versus clinical effect relationship. The concentration of drug in the biophase cannot be measured because it is usually inaccessible, at least in human subjects. The time course of drug effect can be calculated by using rapid measures of drug effect. Knowing the time course of drug effect, the rate of drug flow in and out of the biophase (or effect site) can be calculated with the use of mathematic models. As such, the time course of the plasma concentration and the measured effect can be linked using the concept of the effect compartment, developed by Hull16 and Sheiner. For any concentration in this virtual compartment, a corresponding assumed effect is observed. This relationship between the effect-site concentration and effect is usually nonlinear and static. If the plasma concentration is maintained at a constant level, then the model assumes that, at equilibrium, the effect-compartment concentration equals the plasma concentration. For neuromuscular blocking agents, the response from peripheral nerve stimulation. Various authors have used the T1% (percentage change of the T1 response compared with baseline T1 response during supramaximal stimulus) derived from electromyogram to measure the drug effect of newer drugs such as rocuronium19 and cisatracurium.
A comparison of glycopyrrolate and atropine during reversal of nondepolarizing neuromuscular block with neostigmine arrhythmia specialist tenormin 50 mg with mastercard. The duration of impairment of autonomic control after anticholinergic drug administration in humans. The effects of reversal of neuromuscular blockade on autonomic control in the perioperative period. Anticholinesterase drugs stimulate phosphatidylinositol response in rat tracheal slices. Effects of neostigmine and glycopyrrolate on pulmonary resistance in spinal cord injury. Chemical encapsulation of rocuronium bromide by a cycledextrin-based synthetic host. Cyclodextrin-derived host molecules as reversal agents for the neuromuscular blocker rocuronium bromide. Reversal of neuromuscular blockade and simultaneous increase in plasma rocuronium concentration after the intravenous infusion of the novel reversal agent Org 25969. The efficacy and safety of sugammadex for reversing postoperative residual neuromuscular blockade in pediatric patients. Efficacy, safety, and pharmacokinetics of sugammadex for the reversal of rocuroniuminduced neuromuscular blockade in elderly patients. Reversibility of rocuroniuminduced profound neuromuscular block with sugammadex in younger and older patients. Correlation between cardiac output and reversibility of rocuronium-induced moderate neuromuscular block with sugammadex. Safety and efficacy of sugammadex for the reversal of rocuronium-induced neuromuscular blockade in cardiac patients undergoing noncardiac surgery. The use of rocuronium in a patient with cystic fibrosis and end-stage lung disease made safe by sugammadex reversal. Multicentre, parallel-group, comparative trial evaluating the efficacy and safety of sugammadex in patients with end-stage renal failure or normal renal function. Efficacy, safety and pharmacokinetics of sugammadex 4 mg kg-1 for reversal of deep neuromuscular blockade in patients with severe renal impairment. Pharmacokinetics of sugammadex in subjects with moderate and severe renal impairment. Neuromuscular blocking drugs and their antagonists in patients with organ disease. Randomized comparison of sugammadex and neostigmine for reversal of rocuronium-induced muscle relaxation in morbidly obese undergoing general anaesthesia. Sugammadex ideal body weight dose adjusted by level of neuromuscular blockade in laparoscopic bariatric surgery. Early reversal of profound rocuronium-induced neuromuscular blockade by sugammadex in a randomized multicenter study. Reversal of rocuroniuminduced neuromuscular block by the selective relaxant binding agent sugammadex. Reversal of profound vecuronium-induced neuromuscular block under sevoflurane anesthesia. Reversal of profound rocuronium block monitored in three muscle groups with sugammadex in ponies. Reversal of profound neuromuscular block by sugammadex administered three minutes after rocuronium. Reversal of rocuroniuminduced neuromuscular blockade with sugammadex compared with neostigmine during sevoflurane anaesthesia. Reversal of rocuronium-induced neuromuscular block with sugammadex is faster than reversal of cisatracurium-induced block with neostigmine. Reversal of rocuroniuminduced neuromuscular block with the novel drug sugammadex is equally effective under maintenance anesthesia with propofol or sevoflurane. A randomized, doseresponse study of sugammadex given for the reversal of deep rocuronium- or vecuronium-induced neuromuscular blockade under sevoflurane anesthesia. Reversal of rocuroniuminduced neuromuscular blockade with sugammadex in pediatric and adult surgical patients. Sugammadex used to successfully reverse vecuronium-induced neuromuscular blockade in a 7-month-old infant. A two-year-old patient who received readministration of rocuronium for re-operation 30 minutes after sugammadex reversal. Sugammadex, A selective reversal medication for preventing postoperative residual neuromuscular blockade. Sugammadex reversal of rocuroniuminduced neuromuscular block in Caesarean section patients. Rocuronium and sugammadex for rapid sequence induction of obstetric general anaesthesia. Sugammadex reversal of rocuronium-induced neuromuscular blockade in two types of neuromuscular disorders. Reversal of neuromuscular blockade with sugammadex in patients with myasthenia gravis. Feasibility of full and rapid neuromuscular blockade recovery with sugammadex in myasthenia gravis patients undergoing surgery-a series of 117 cases.
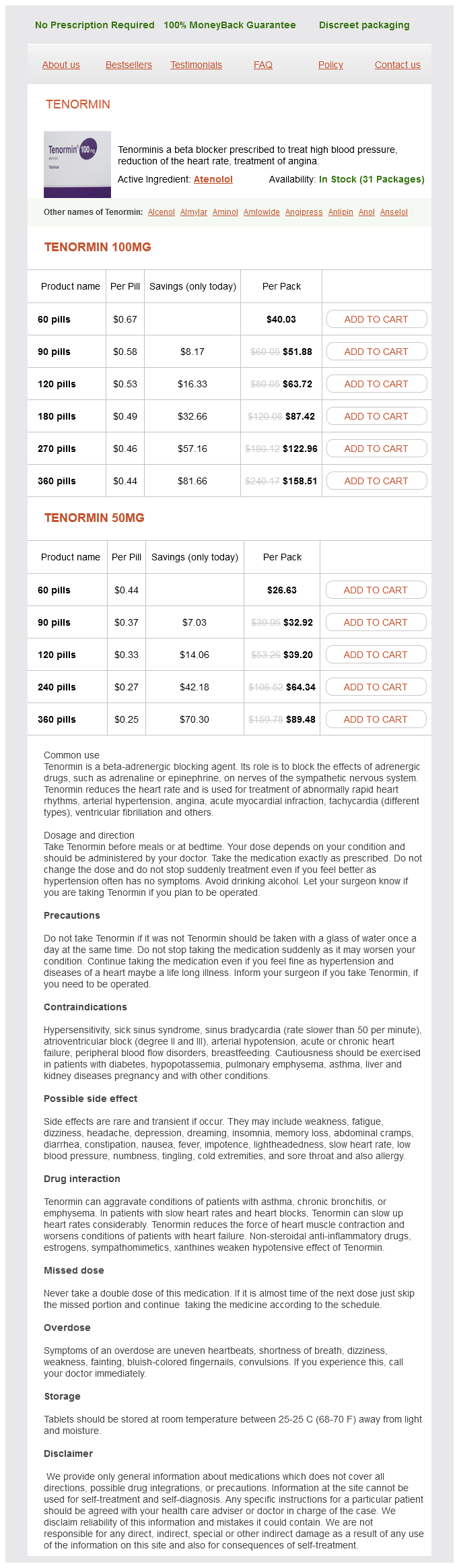
Tenormin Dosage and Price
Tenormin 100mg
- 60 pills - $40.03
- 90 pills - $51.88
- 120 pills - $63.72
- 180 pills - $87.42
- 270 pills - $122.96
- 360 pills - $158.51
Tenormin 50mg
- 60 pills - $26.63
- 90 pills - $32.92
- 120 pills - $39.20
- 240 pills - $64.34
- 360 pills - $89.48
Pulmonary compliance is increased by decreased functional residual capacity and is often further decreased in the Trendelenburg position hypertension cdc purchase tenormin 100 mg visa, due to patient-positioning straps across the chest. In patients under general anesthesia, these pulmonary changes result in higher airway pressures. Changes to the mechanical ventilator settings can compensate for some of the respiratory changes. However, with patient body habitus and variations in positioning, the higher airway pressures, and changes to minute ventilation are too great to safely continue in the steep Trendelenburg position. Testing the position for patient tolerance after anesthetic induction and completed positioning, prior to the initiation of the surgical procedure, is recommended. Trendelenburg is contraindicated in patients with increased intracranial pressures. Shoulder braces should be avoided to prevent brachial plexus compression injuries. Consideration of the impact of positioning on intracranial pressure is important, as it may not only affect intraoperative positioning but also may have consequences on site selection for central line placement. Frequently, femoral vein site selection is preferred in patients with severely elevated intracranial pressure in order to avoid exacerbating intracranial hypertension with patient position changes during line placement. Prolonged head-down positioning can also lead to swelling of the face, conjunctiva, larynx, and tongue, with an increased potential for postoperative upper airway obstruction. The Trendelenburg position increases intraabdominal pressure and displaces the stomach placing the patient at a higher risk for aspiration. Endotracheal intubation is often preferred in order to prevent aspiration of gastric contents. Care must be taken to prevent patients in steep head-down positions from slipping cephalad on the surgical instruments. Beanbag pads become rigid when suction is applied to set the shape, and their use in the Trendelenburg position has been associated with brachial plexus injuries. This position is increasingly popular because of the growing number of laparoscopic surgeries requiring this position. As mentioned earlier, any position where the head is above the heart reduces cerebral perfusion pressure and may also cause systemic hypotension. If invasive arterial pressure monitoring is used then the arterial pressure transducer should be zeroed at the level of the Circle of Willis. Complications of the Supine Position the base of the surgical table is asymmetric. This risk is higher with obese patients and when the table is in the Trendelenburg position. The surgical table weight limits are significantly different when the table is reversed and should be strictly observed. Back pain is common in the supine position because the normal lumbar lordotic curvature is often lost. General anesthesia with muscle relaxation and neuraxial block increases the risk of back pain further due to loss of tone in the paraspinous muscles. Patients with extensive kyphosis, scoliosis, or a history of back pain may require extra padding of the spine or slight flexion at the hip and knee. Peripheral nerve injury (discussed later in this chapter) is a complex phenomenon with multifactorial causes. Arm abduction is limited to less than 90 degrees when supine because when the arm is raised the head of the humerus rotates caudad and stretches the plexus. Shoulder braces should be avoided; they may cause direct compression of the plexus medially between the clavicle and first rib or laterally below the head of the humerus. Abduction of the arm should be avoided when in a steep head-down position if shoulder braces or a beanbag holds the shoulders. The correct position of "candy cane" supports is well away from the lateral fibular head. The fingers are at risk for compression when the lower section of the bed is raised. The foot section of the surgical table is lowered and sometimes removed from the end of the table. The legs should be raised together; simultaneously, the knees and hips are flexed. Padding of the lower extremities is critical, particularly over bony prominences, to prevent compression against the leg supports. The peroneal nerve is particularly prone to injury as it lies between the fibular head and compression from the leg support (see the peripheral nerve injury section of this chapter). When the foot of the table is raised at the end of the procedure the fingers near the open edge can get crushed. For this reason, the recommended position of the arms is on armrests far from the table hinge point. When the legs are elevated, venous return increases, causing a transient increase in cardiac output and, to a lesser extent, cerebral venous and intracranial pressure in otherwise healthy patients. In addition, the lithotomy position increases intraabdominal pressure and causes the abdominal viscera to displace the diaphragm cephalad, reducing lung compliance and potentially resulting in a decreased tidal volume. As with the supine position, the curvature of the lumbar spine is lost in lithotomy and can put the patient at risk of back pain. Compartment syndrome is caused by increased tissue pressure within a fascial compartment due to tissue ischemia, edema, and rhabdomyolysis. Inadequate arterial inflow (from lower extremity elevation) and decreased venous outflow (due to direct compression or excessive hip flexion) elevates the risk of compartment syndrome for patients in lithotomy.
© 2025 Adrive Pharma, All Rights Reserved..