General Information about Super Levitra
Super Levitra is a medicine specifically designed to treat each ED and PE in males. It contains a mixture of two active components - Vardenafil and Dapoxetine. Vardenafil is a sort of treatment called a phosphodiesterase type 5 (PDE5) inhibitor, which works by stress-free the muscular tissues within the partitions of blood vessels, growing blood move to the penis, and allowing for a agency and long-lasting erection. Dapoxetine, however, is a selective serotonin reuptake inhibitor (SSRI), which is used to treat PE by delaying ejaculation.
One of the advantages of utilizing Super Levitra is that it's confirmed to be effective in the treatment of each ED and PE. Clinical research have proven that it considerably improved the ability to achieve and maintain an erection, in addition to increase the time to ejaculation. This makes it the ideal choice for males who are suffering from both situations, eliminating the need for multiple medications.
Super Levitra comes in a 80 mg tablet, with each tablet containing 20 mg of Vardenafil and 60 mg of Dapoxetine. It is normally taken orally, with or without meals, roughly 20-30 minutes earlier than participating in sexual exercise. Its effects can last for up to eight hours, giving men enough time to get pleasure from a quantity of sexual encounters.
Erectile dysfunction (ED) and premature ejaculation (PE) are two frequent sexual problems that can tremendously have an effect on a man's high quality of life. ED, also referred to as impotence, is the inability to achieve or preserve an erection enough for sexual intercourse. PE, then again, is when a man ejaculates too quickly, usually earlier than or shortly after penetration, leaving both companions unsatisfied. These circumstances could cause emotional misery, relationship problems, and even result in low self-esteem. Luckily, there's a answer - Super Levitra.
Super Levitra can be recognized for its fast onset of motion, allowing men to experience its results quickly after taking the treatment. This is especially helpful for spontaneous sexual exercise, where planning forward is not all the time an option. Additionally, it has a low threat of unwanted effects, with the most common being headache, dizziness, and nausea. As with any treatment, it is essential to consult with a well being care provider before taking Super Levitra to make sure it's secure for you, especially in case you have any underlying health situations or are taking different medicines.
In conclusion, Super Levitra is a extremely efficient and fast-acting medicine for treating both ED and PE. Its mixture of Vardenafil and Dapoxetine presents a two-in-one solution, making it a convenient and cost-effective option for men with each situations. With its proven outcomes and low threat of unwanted effects, Super Levitra supplies a chance for males to regain their sexual confidence and improve their overall well-being. If you're struggling with ED and PE, talk to your physician about Super Levitra and take step one towards a satisfying and satisfying intercourse life.
Patients Taking Steroids for Other Reasons Perioperative Stress and the Need for Corticoid Supplementation erectile dysfunction treatment alprostadil buy 80 mg super levitra overnight delivery. The adrenal responses of normal patients 32 · Anesthetic Implications of Concurrent Diseases 1011 to the perioperative period, as well as the responses of patients taking steroids for other diseases, indicate the following: 1. Perioperative stress is related to the degree of trauma and the depth of anesthesia. Deep general or regional anesthesia delays the usual intraoperative glucocorticoid surge to the postoperative period. A few patients with suppressed adrenal function will have perioperative cardiovascular problems if they do not receive supplemental steroids perioperatively. Although a patient who takes steroids on a long-term basis may become hypotensive perioperatively; glucocorticoid or mineralocorticoid deficiency is seldom the cause. Longer duration and higher home steroid dose increase the likelihood of deficiency. Giving these patients steroid coverage equivalent to 100 mg of hydrocortisone perioperatively has little risk. The animals were then randomly allocated to groups that received subphysiologic (one-tenth of the normal cortisol production), physiologic, or supraphysiologic (10 times the normal cortisol production) doses of cortisol for 4 days preceding abdominal surgery (cholecystectomy). The group given subphysiologic doses of steroid perioperatively had a significant increase in postoperative mortality. Death rates for the physiologic and supraphysiologic replacement groups were the same and did not differ from the rate for sham-operated controls. Death in the subphysiologic replacement group was related to severe hypotension associated with a significant decrease in systemic vascular resistance and a reduced left ventricular stroke work index. Filling pressures of the heart were unchanged when compared with those in control animals. Despite the low systemic vascular resistance, the animals did not become tachycardic. All these responses are compatible with the previously documented interaction of glucocorticoids and catecholamines, and thus suggest that glucocorticoids mediate catecholamine-induced increases in cardiac contractility and maintenance of vascular tone. The investigators used a sensitive measure of wound healing involving accumulation of hydroxyproline. All treatment groups, including the group given supraphysiologic doses of glucocorticoids, had the same capacity for wound healing. Furthermore, perioperative administration of supraphysiologic doses of corticosteroids produced no adverse metabolic consequences. This study confirmed long-standing intuitive impressions concerning patients who had inadequate adrenal function as a result of either underlying disease or administration of exogenous steroids-inadequate replacement of corticosteroids can lead to addisonian crisis and increased mortality, whereas the administration of supraphysiologic doses of steroids for a short time perioperatively can be safe. It is clear that inadequate corticosteroid coverage can cause death, but what is not so clear is what dose of steroid should be recommended for replacement therapy. Yong and colleagues reviewed the randomized controlled trials for a Cochrane Systemic Review and reported only two trials involving 37 patients that met the inclusion criteria. The authors concluded that they were unable to support or refute the use of supplemental perioperative steroids for patients with adrenal insufficiency during surgery. Because the risk is low and the benefit is high, physicians should consider providing supplementation for any patient who has received steroids within a year. The morning plasma cortisol level does not reveal whether the adrenal cortex has recovered sufficiently to ensure that cortisol secretion will increase adequately to meet the demands of stress. Inducing hypoglycemia with insulin has been advocated as a sensitive test of pituitary-adrenal competence, but it is impractical and is probably a more dangerous practice than simply administering glucocorticoids. If the plasma cortisol concentration is measured during acute stress, a value of greater than 25 g/dL assuredly (and a value >15 g/dL probably) indicates normal pituitary-adrenal responsiveness. In another test of pituitary-adrenal sufficiency, the baseline plasma cortisol level is determined. A lesser response usually indicates pituitary-adrenal insufficiency, possibly requiring perioperative supplementation with steroids. Good correlation exists between the severity and duration of the operation and the response of the adrenal gland. In a study of 20 patients during major surgery, the mean maximal concentration of cortisol in plasma was 47 g/dL (range, 22-75 g/dL). During minor surgery, the mean maximal concentration of cortisol in plasma was 28 g/dL (range, 10-44 g/dL). Although the precise amount required has not been established, we usually intravenously administer the maximum amount of glucocorticoid that the body manufactures in response to maximal stress. Unless infection or some other perioperative complication develops, we decrease this dose by approximately 50%/day until the standard home dose is resumed. For major surgical procedures, we usually give 50 mg every 6 hours to 100 mg every 8 hours. Again unless a complication develops, this is decreased 50%/day until the standard home dose is resumed. Rare complications of perioperative steroid supplementation include aggravation of hypertension, fluid retention, inducement of stress ulcers, and psychiatric disturbances. Two possible complications of short-term perioperative supplementation with glucocorticoids are abnormal wound healing and an increased rate of infections. This evidence is inconclusive, however, because it relates to short-term glucocorticoid administration and not to long-term administration of glucocorticoids with increased doses at times of stress. In contrast to a deleterious effect of perioperative glucocorticoid administration on wound healing in rats, a study involving primates suggested that large doses of glucocorticoids, administered perioperatively, do not impair sensitive measures of wound healing. Information on the risk of infection from perioperative glucocorticoid supplementation is also unclear as there are no controlled trials addressing these effects. In many studies of long-term use by patients and supplementation, no increased risk of serious infections was reported with longterm use of steroids alone. Data indicate that the risk of infection in a patient taking steroids on a long-term basis is real, but whether perioperative supplementation with steroids increases that risk is not clear.
Global Blood Flow Monitoring Techniques (Noninvasive) Intravascular Tracer Compounds erectile dysfunction treatment in sri lanka 80 mg super levitra purchase otc. Shown are computer tomographic images of a patient 90 minutes after onset of a left middle cerebral artery stroke. The site of the occlusion in coronal (A) and axial (B) planes is indicated by a red arrow. Panel C shows the arterial inflow function and venous outflow function derived by repeated imaging of the passage of radiopaque contrast through a volume element (voxel) representative of arterial and venous territory, respectively. The A2 segment of the anterior cerebral artery is typically chosen as a voxel for the arterial inflow function and the superior sagittal sinus for the venous outflow function. Based on these functions, blood flow, volume, and flow kinetics can be calculated for other areas of the image. The cerebral blood flow map (D) shows symmetrical flow in both hemispheres, with warmer colors indicating areas of higher flow consistent with grey matter. Blood volume (E) is symmetrical as well, but the time to the peak concentration of contrast (F) is significantly delayed for brain affected by the stroke. The degree of oxygen extraction by an organ can be monitored by following the oxygen saturation of the mixed venous blood that drains that organ. In the case of the brain, jugular bulb venous oxygen saturation (Sjvo2) is believed to measure the degree of oxygen extraction by the brain and to represent the balance between cerebral oxygen supply and demand. To monitor Sjvo2, a fiberoptic catheter is placed in a retrograde fashion into the jugular bulb through the internal jugular vein under fluoroscopic guidance. Correct tip placement is crucial to minimize admixture of extracranial venous blood. Several theoretical limitations of the technique must be borne in mind to interpret Sjvo2 values and trends properly. Although nearly all blood from the brain drains via the jugular veins, intracranial mixing of venous blood is incomplete and may result in differences between right-sided and leftsided measurements. Because Sjvo2 represents the balance between supply and demand, interpretation of the absolute value of Sjvo2 must take the clinical circumstances into account. Cerebral oximetry is a noninvasive technique that, similar to Sjvo2, uses reflectance oximetry to measure the oxygen saturation of the tissues underneath the sensor. The light passes not only through parts of the frontal brain, but also through the overlying skull and scalp. Contamination of the oximetry signal by extracranial blood sources is a serious concern, although the use of two sensing diodes with different distances from the light source within one sensor patch and adjustments of the algorithm of the oximeter may minimize this problem. The captured Doppler signals originate from the right middle, right anterior, and left anterior cerebral arteries. By convention, flow toward the probe is displayed as a waveform above the baseline. Because 66% to 80% of the cerebral blood volume is venous blood, cerebral oximetry determines predominantly "local venous oxygen saturation. First, adequacy of global cerebral perfusion is inferred from measurements over the frontopolar brain. Second, normative data on normal values or expected changes for cerebral oximetry are largely absent, but preoperative application of the sensors allows the start of a trend in conjunction with a neurologic baseline examination. The real problem is that the lower limit for acceptable regional oxygen saturation is unknown in a large population of patients. Tissue-Level Blood Flow Monitoring Techniques (Invasive) Tissue-level monitoring for the brain is by definition invasive. All monitors in current clinical or research use are implanted through a burr hole, extend either into the white matter or ventricular system, and typically use a bolt for stabilization. They all share a 1% to 2% risk of bleeding, infection, or ischemia owing to the implantation procedure. When these monitors were first developed, there was considerable debate regarding the optimal placement of the device given such limited spatial resolution. Thermal diffusion blood flow measurement and laser Doppler flow measurement are experimental and not in widespread clinical use. Tissue Partial Pressure of Oxygen Monitoring Localized monitoring of tissue Po2 is based on an oxygensensitive electrode originally described by Clark. Currently available catheter-based electrodes placed into the subcortical white matter provide stable recording conditions over long periods. The electroencephalographer can accurately identify consciousness, unconsciousness, seizure activity, stages of sleep, and coma. In the absence of significant changes in anesthetic technique, the electroencephalographer also can accurately identify inadequate oxygen delivery to the brain (from either hypoxemia or ischemia). Evoked potentials are electrical activity generated in response to either a sensory or a motor stimulus. Measurements of evoked responses may be made at multiple points along an involved nervous system pathway. The evoked responses are generally smaller than other electric activity generated in nearby tissue (muscle or brain) and are readily obscured by these other biologic signals. Motor-evoked responses are generally larger and commonly do not require averaging. The signals are very small, and each recording electrode records information both directly beneath the electrode and information volume conducted from deeper tissue. Alternatively, subdermal needle electrodes may be used, particularly when sterile application of an electrode close to a surgical field is necessary. When electrodes are applied directly to the surface of the brain, impedance is minimized by close electrode contact and saturation of the area with an electrolyte solution. Based on 10% or 20% of these distances, recording electrodes are placed systematically over the frontal (F), parietal (P), temporal (T), and occipital (O) regions at increasing distances from the midline. Left-sided electrodes are given odd number subscripts, and right-sided electrodes are given even number subscripts.
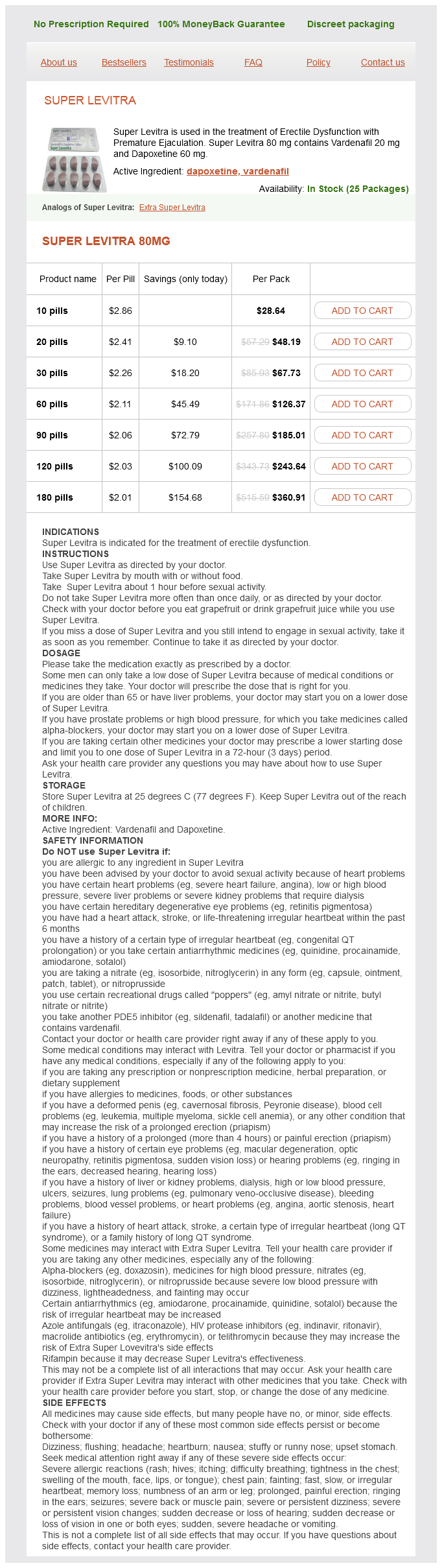
Super Levitra Dosage and Price
Super Levitra 80mg
- 10 pills - $28.64
- 20 pills - $48.19
- 30 pills - $67.73
- 60 pills - $126.37
- 90 pills - $185.01
- 120 pills - $243.64
- 180 pills - $360.91
The mechanism responsible for this likely involves relatively greater stimulation of muscarinic receptors in the sinus node erectile dysfunction hormones purchase super levitra 80 mg with mastercard, thus suppressing the sinus mechanism and allowing the emergence of the atrioventricular node as the pacemaker. The incidence of junctional rhythm is greater after a second dose of succinylcholine, and may be prevented by prior administration of dTc. Under stable anesthetic conditions, succinylcholine decreases the threshold of the ventricle to catecholamine-induced dysrhythmias in monkeys and dogs. Circulating catecholamine concentrations increase fourfold, and K+ concentrations increase by one third, following succinylcholine administration in dogs. The possible influence of drugs such as digitalis, tricyclic antidepressants, monoamine oxidase inhibitors, exogenous catecholamines, and anesthetic drugs such as halothane, which may lower the ventricular threshold for ectopic activity or increase the arrhythmogenic effect of the catecholamines, should also be considered. Ventricular escape beats may also occur as a result of severe sinus bradycardia and atrioventricular nodal slowing secondary to succinylcholine administration. The incidence of ventricular dysrhythmias is further increased by the release of K+ from skeletal muscle as a consequence of the depolarizing action of the drug. The drug stimulates cholinergic autonomic receptors on both sympathetic and parasympathetic ganglia45 and muscarinic receptors in the sinus node of the heart. With large doses of succinylcholine, these effects may become positive,46 causing tachycardia. The clinical manifestation of generalized autonomic stimulation is the development of sinus bradycardia, junctional rhythms, and ventricular dysrhythmias. Clinical studies have described these dysrhythmias under various conditions in the presence of the intense autonomic stimulus of tracheal intubation. It is not entirely clear whether the cardiac irregularities are caused by the action of succinylcholine alone or by the added presence of extraneous autonomic stimulation. An in vitro study using ganglionic acetylcholine receptors subtype 34 expressed in Xenopus laevis oocytes suggested that succinylcholine at clinically relevant concentrations had no effect on the expressed receptors. Stimulation of cardiac muscarinic receptors in the cardiac sinus node causes sinus bradycardia. This side effect is particularly problematic in individuals with predominantly vagal tone, such as in children who have not received atropine. Sinus bradycardia can occur in adults and appears more commonly after a second dose of the drug administered approximately 5 minutes after the initial dose. This slight increase in K+ is well tolerated by most individuals and generally does not cause dysrhythmias. With activation of the acetylcholine channels, movement of Na+ into the cells is accompanied by movement of K+ out of the cells. Patients with renal failure are no more susceptible to an exaggerated response to succinylcholine than are those with normal renal function. Should severe hyperkalemia occur, it can be treated with immediate hyperventilation, infusion of 500-1,000 mg calcium chloride or calcium gluconate over 3 minutes intravenously, and 10 units of regular insulin in 50 mL of 50% glucose for adults or, for children, 0. Kohlschütter and associates found that four of nine patients with severe abdominal infections had an increase in serum K+ levels of as much as 3. Stevenson and Birch described a single, well-documented case of a marked hyperkalemic response to succinylcholine in a patient with a closed head injury without peripheral paralysis. Three weeks after injury, three of the patients studied in this series, who had especially severe injuries, became markedly hyperkalemic with an increase in serum K+ of more than 3. Birch and coworkers also found that the prior administration of 6 mg of dTc prevented the hyperkalemic response to succinylcholine. Additionally, patients with conditions that result in the proliferation of extrajunctional acetylcholine receptors, such as upper or lower motor denervation, immobilization, burn injuries, and neuromuscular disease, are likely to have an exaggerated hyperkalemic response following the administration of succinylcholine. Some of these disease states include cerebrovascular accident with resultant hemiplegia or paraplegia, muscular dystrophies, and Guillain-Barré syndrome. The hyperkalemia following administration of succinylcholine may be severe enough that cardiac arrest ensues. For a review of succinylcholine-induced hyperkalemia in acquired pathologic states, see Martyn and Richtsfeld. For instance, coughing, vomiting and maximal forced lid closure may induce increases in intraocular pressure that are 3-4 times greater (60-90 mm Hg) than those induced by succinylcholine administration. Finally, should a patient become too lightly anesthetized during intraocular surgery, succinylcholine should not be given to immobilize the patient. This is not surprising because more coordinated abdominal skeletal muscle activity. This may be related to the minimal or absent fasciculations from succinylcholine in these young patients. Meakin and associates suggested that the high incidence of spasm in children may result from inadequate dosage of succinylcholine. Although an increase in tone of the masseter muscle may be an early indicator of malignant hyperthermia, this finding is not consistently associated with that syndrome. When the muscle relaxant cross-links with IgE, degranulation and release of histamine, neutrophil chemotactic factor, and platelet-activating factor occur. The release of these mediators can induce cardiovascular collapse, bronchospasm, and skin reaction. The cross-reactivity is related to the common structural features of these drugs, all of which contain quaternary ammonium ions. Increased Intracranial Pressure Succinylcholine has the potential to increase intracranial pressure. Other investigators have found that myalgias following outpatient laparoscopic surgery (and atracurium administration) occur even in the absence of succinylcholine.
© 2025 Adrive Pharma, All Rights Reserved..