General Information about Super Avana
In conclusion, Super Avana is a safe and effective medicine for men suffering from erectile dysfunction and premature ejaculation. Its unique mixture of Avanafil and Dapoxetine make it a handy and reliable option for those trying to enhance their sexual performance. If you might be experiencing these sexual issues, speak along with your doctor to see if Super Avana is the right therapy choice for you.
Super Avana comes in tablet kind, and the beneficial dosage is one pill per day, taken half-hour earlier than sexual activity. This makes it a handy and discreet possibility for males who need to enhance their sexual performance. It can additionally be necessary to note that Super Avana should not be taken with alcohol, as it could possibly enhance the danger of unwanted side effects and reduce the effectiveness of the treatment.
Super Avana is not suitable for everyone and may only be taken after consulting a health care provider. It is particularly necessary to speak with a healthcare professional if you're taking any other drugs or have underlying health situations.
Erectile dysfunction (ED) and premature ejaculation (PE) are two common sexual disorders that affect millions of men worldwide. These conditions can have a big impact on a person's self-esteem and relationship with their companion. Fortunately, there are medications out there to treat these conditions, together with Super Avana.
As with any medication, there could additionally be unwanted facet effects associated with taking Super Avana. These can include complications, dizziness, nausea, and flushing. However, these side effects are normally delicate and short-term, and may be managed by adjusting the dosage or talking to a healthcare professional.
In addition to its effectiveness in treating ED and PE, Super Avana has also been proven to extend sexual satisfaction in males. A examine printed in the Journal of Sexual Medicine found that men taking Super Avana reported a significant improvement in their overall sexual satisfaction, compared to those taking a placebo.
The mixture of those two ingredients in Super Avana makes it a novel and effective treatment for both ED and PE. This implies that males with each conditions can profit from taking just one treatment, instead of having to take multiple medicine.
Super Avana is a prescription medicine that is specifically designed to deal with male erectile dysfunction. It is a combination drug that contains Avanafil and Dapoxetine. Avanafil is a PDE-5 inhibitor that helps to chill out the blood vessels within the penis, growing blood circulate and allowing for a prolonged and sustained erection. Dapoxetine, on the other hand, is a selective serotonin reuptake inhibitor (SSRI) that helps to delay ejaculation and improve control over ejaculation.
One of the primary advantages of Super Avana is the extended length of action. While other erectile dysfunction medicines might final for just some hours, Super Avana can present as much as 6 hours of improved sexual performance. This gives males extra management over their sexual expertise and permits for extra spontaneity in their intimate relationships.
This is equivalent to a needing to invite 1 erectile dysfunction ginseng 160 mg super avana purchase with amex,904 women to screenings over 10 years to prevent one breast cancer death. In addition, estimates of overdiagnosis in this group range from 10% to 40% of diagnosed invasive cancers. Mammographic screening and mortality from breast cancer: the Malmo mammographic screening trial. Randomised trial from the Breast Cancer Screening Working Group of the Swedish National Board of Health and Welfare. The Swedish two county trial of mammographic screening for breast cancer: recent results and calculation of benefit. The Canadian National Breast Screening Study-1: breast cancer mortality after 11 to 16 years of follow-up. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. Randomized study of mammography screening-preliminary report on mortality in the Stockholm trial. Screening Women at High Risk There is interest in creating risk profiles as a way of reducing the inconveniences and harms of screening. It might be possible to identify women who are at greater risk of breast cancer and refocus screening efforts on those most likely to benefit. Risk factors for breast cancer include the following: Extremely dense breasts on mammography or a first-degree supplemental imaging and biopsies. Few studies have assessed the association between these factors and death from breast cancer; however, reproductive factors and breast density have been shown to have limited influence on breast cancer mortality. Unfortunately, when to begin and the optimal frequency of screening have not been defined. The fact that mammography screening has increased the incidence of localized disease without a significant change in metastatic disease at the time of diagnosis suggests that there is some degree of overdiagnosis. The risk of overdiagnosis is greatest at the first screening3 and varies with patient age, tumor type, and grade of disease. In the United States, about 10% of all women screened for breast cancer are called back for additional testing, and less than half of them will be diagnosed with breast cancer. Mucinous and lobular tumors and rapidly growing tumors tend to blend in with normal breast architecture. It has been estimated that annual mammographies will cause up to 1 case of breast cancer per 1,000 women screened from age 40 to age 80 years. It has yet to be determined whether supplemental imaging reduces breast cancer mortality in women with increased breast density. Although it continues to be strongly advocated by some, systematic reviews have concluded that the evidence is currently insufficient to recommend for or against this approach. A mammography will not detect all breast cancers, and some breast cancers detected with mammographies may still have a poor prognosis. When abnormal findings cannot be resolved with additional imaging, a biopsy is required to rule out the possibility of breast cancer. The physician and patient should take into account individual risks and concerns before deciding to screen. The desire to examine the entire colon led to the use of a barium enema and the development of fecal occult blood tests. With the development of fiber optics, flexible sigmoidoscopies and, later, colonoscopies were employed. Screening examinations of the colon and rectum can find cancer early, but also find precancerous polyps. Randomized trials have demonstrated that endoscopic polypectomies reduce the incidence of colorectal cancer by about 20%. With 13 years of follow-up, the annual screened arm had a 33% relative reduction in colorectal cancer mortality compared to the usual care group. Flexible sigmoidoscopies are, of course, limited to an examination of the rectum and sigmoid colon. A prospective randomized trial of once-only flexible sigmoidoscopies demonstrated a 23% reduction in colorectal cancer incidence and a 31% reduction in colorectal cancer mortality after a median 11. It is estimated that flexible sigmoidoscopies can find 60% to 80% of cancers and polyps found by colonoscopies. The colonoscopy has become the preferred screening method of many, although there have been no prospective, randomized trials of colonoscopy screening. Perhaps the best support for colonoscopy screening is indirect evidence from the Minnesota Colon Cancer Control Study, which required that all participants with a positive stool blood test have diagnostic imaging of the entire colon. In the Minnesota study, more than 40% of those screened annually eventually received a colonoscopy. One can also make the argument that the sigmoidoscopy studies indirectly support the efficacy of colonoscopy screening, although it can be argued that embryologic and epidemiologic evidence indicate that the right and left colon are biologically distinct and, therefore, the mortality benefits from sigmoidoscopies do not constitute proof that a colonoscopy would similarly reduce mortality from proximal colon lesions. In studies involving repeat colonoscopies by a second physician, 21% of all adenomas were missed, including 26% of 1 to 5 mm adenomas and 2% of adenomas 10 mm or more in length. The cost of the procedure and the limited number of physicians who can do the procedure are also of concern. The rate of extracolonic findings of uncertain significance is high (15% to 30%), and each one must be evaluated, thereby contributing to additional expense and potential morbidity. The long-term, cumulative radiation risk of repeated colonography screenings is also a concern.
They target the activated endothelium directly and inhibit multiple angiogenic proteins erectile dysfunction signs 160 mg super avana order mastercard. The limitation to indirect inhibitors is that, over time, tumor cells may acquire mutations that lead to increased expression of other proangiogenic proteins that are not blocked by the indirect inhibitor. This may give the appearance of drug resistance and warrants the addition of a second antiangiogenic agent, one that would target the expression of these upregulated proangiogenic proteins. An increased Ang2/Ang1 ratio correlates with tumor angiogenesis and poor prognosis in many cancers, thus making the angiopoietins an attractive therapeutic target. Angiopoietin inhibitors are currently under investigation in the preclinical and clinical setting. The involvement of integrin in tumor angiogenesis was demonstrated in studies that show the -4 subunit of integrin promoting endothelial migration and invasion. However, all three integrin inhibitors have proven to be largely ineffective in various early and late stage cancer trials. Other approved drugs that also inhibit angiogenesis as a secondary function, such as thalidomide, are discussed in greater detail in another section of this textbook and are presented in Table 28. The frequency of vascular-related adverse events appeared to be higher with ziv-aflibercept than bevacizumab treatment when compared across trials. Median survival and the time to radiologic progression were nearly 3 months longer for patients treated with sorafenib than for those given placebo. Common adverse events include diarrhea, rash/desquamation, fatigue, handÂfoot skin reaction, alopecia, and nausea/ vomiting. In addition, a decrease in left ventricular ejection fraction and severe hypertension were also more commonly reported in the sunitinib arm. Grade 3 or 4 treatment-emergent adverse events were reported in 56% versus 51% of patients on sunitinib versus placebo, respectively. Pazopanib exhibited in vivo and in vitro activity against tumor growth, and early clinical trials demonstrated potent antitumor and antiangiogenic activity. The most frequent adverse events with axitinib were diarrhea (all grade), hypertension (all grade), fatigue, decreased appetite, nausea, and dysphonia. Moreover, hypertension, nausea, dysphonia, and hypothyroidism were more common with axitinib, whereas palmarÂplantar erythrodysesthesia, alopecia, and rash were more frequent with sorafenib. Manageable toxicities included diarrhea, palmarÂplantar erythrodysesthesia, decreased weight and appetite, nausea, and fatigue. The most common adverse events that were grade 3 or higher and related to regorafenib were handÂfoot skin reaction, fatigue, diarrhea, hypertension, and rash or desquamation. The most common adverse reactions that occurred were rash, asthenia, mucositis, nausea, edema, and anorexia. Rare, but serious adverse reactions associated with temsirolimus included interstitial lung disease, bowel perforation, and acute renal failure. The most common grade 3/4 adverse reactions were infections, dyspnea, fatigue, stomatitis, dehydration, pneumonitis, abdominal pain, and asthenia. The recommended ramucirumab dose and schedule is 8 mg/kg administered as a 60-minute intravenous infusion every 2 weeks. Based on current evidence, with a few exceptions, effective therapy will probably rely on a combinatorial approach that involves targeting multiple pathways simultaneously. Moreover, a number of studies have shown that antiangiogenic agents in combination with chemotherapy or radiotherapy result in additive or synergistic effects. Several models have been proposed to explain the mechanism responsible for this potentiation, keying in on the chemosensitizing effects of antiangiogenic therapy. Biomarkers of tumor angiogenesis activity are important to guide clinical development of these agents and to select patients most likely to benefit from this approach. Although there are currently no validated biomarkers for clinically assessing the efficacy of or selecting patients who will respond to antiangiogenic therapies, a number of candidate markers, including tissue, imaging, and circulating biomarkers, are emerging that need to be prospectively validated. Another model addresses the use of antiangiogenic drugs to slow down tumor cell repopulation between successive cycles of cytotoxic chemotherapy. In fact, a preclinical study in murine tumor models demonstrated that the administration of sunitinib markedly reduced chemotherapy-induced bone marrow toxicity, suggesting that the sequential treatment regimen (delivery of antiangiogenics followed by chemotherapy) showed superior survival benefits compared with the simultaneous administration of two drugs. Furthermore, an additional challenge is to determine the optimal dose and duration of antiangiogenic drugs as well as the impact of drug sequencing in combination regimens. If validated, these findings could help identify which subgroup of patients should receive antiangiogenic therapy and could lead the way to possible future tailoring of individualized antiangiogenic therapy. This resistance involves the reactivation of tumor angiogenesis and increased expression of other proangiogenic factors. Dormancy of micrometastases: balanced proliferation and apoptosis in the presence of angiogenesis suppression. A model of human tumor dormancy: an angiogenic switch from the nonangiogenic phenotype. Persistence of microscopic human cancers in mice: alterations in the angiogenic balance accompanies loss of tumor dormancy. Oncogenes and tumor angiogenesis: the question of vascular "supply" and vascular "demand". Inhibition of Dll4 signalling inhibits tumour growth by deregulating angiogenesis. However, resistance to these drugs eventually occurs, implicating the existence of additional pathways mediating resistance to antiangiogenic therapies. Moreover, tumor cells bearing genetic alterations of the p53 gene may display a lower apoptosis rate under hypoxic conditions, which might reduce their reliance on vascular supply and, therefore, their responsiveness to antiangiogenic therapy. Other possible mechanisms for acquired resistance include tumor vessels becoming less sensitive to antiangiogenic agents, tumor regrowth via rebound revascularization, and vessel cooption.
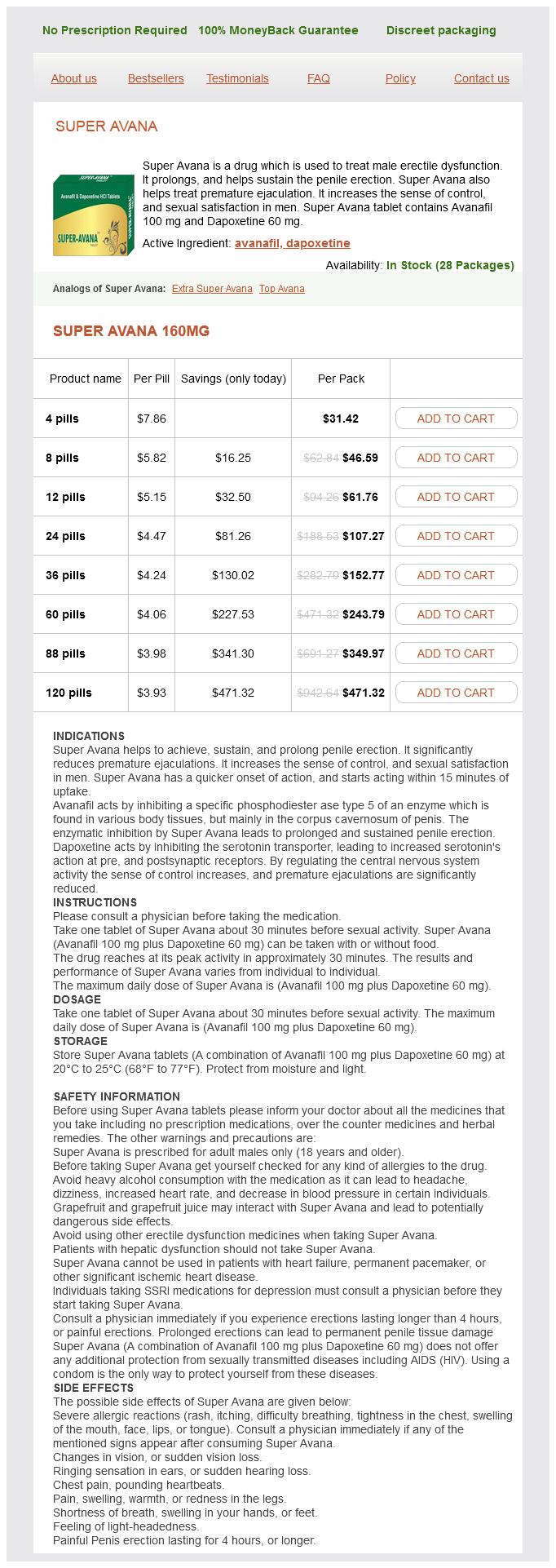
Super Avana Dosage and Price
Super Avana 160mg
- 4 pills - $31.42
- 8 pills - $46.59
- 12 pills - $61.76
- 24 pills - $107.27
- 36 pills - $152.77
- 60 pills - $243.79
- 88 pills - $349.97
- 120 pills - $471.32
Palliative treatment is usually delivered in a smaller number of larger radiation fractions (see the section titled Fractionation) because the desire to simplify the treatment for a patient with limited life expectancy outweighs the somewhat increased potential for late side effects statistics for erectile dysfunction super avana 160 mg order visa. The most common method of achieving accelerated fractionation is to give a standard fraction to the entire field in the morning and to give a second treatment to the boost field in the afternoon (called concomitant boost). As in standard radiation, the boost would be given by extending the length of the treatment course; this concomitant boost approach can shorten treatment from 7 weeks to 5 weeks in head and neck cancer. Hyperfractionation is defined as the use of more than one fraction per day separated by more than 6 hours (see the section titled Biologic Aspects of Radiation Oncology), with a dose per fraction that is less than standard. Hyperfractionation is expected to produce fewer late complications for the same acute effects against both rapidly dividing normal tissues and tumors. Pure hyperfractionation might give 1 Gy twice a day, so that the total dose per day would be 2 Gy, and thus be equal to standard fractionation. The overall effect is to increase the acute toxicity (which resolves) and tumor response, while not increasing the (dose-limiting) late toxicity, which can improve cure rate. Both accelerated fractionation and hyperfractionation have been demonstrated in a meta-analysis to be superior to standard fractionation in the treatment of head and neck cancer with radiation alone. Hypofractionation might be expected to cause more late toxicity for the same antitumor effect than standard or hyperfractionation. In the past, this approach was reserved for palliative cases, with the sense that a modest potential for increased late toxicity was not a major concern in patients with limited life expectancy. Standard fractionation for radiation therapy is defined as the delivery of one treatment of 1. This approach produces a fairly well-understood chance of tumor control and risk of normal tissue damage (as a function of volume). By altering the fractionation schemes, one may be able to improve the outcome for patients undergoing curative treatment or to simplify the treatment for patients receiving palliative therapy. Two forms of altered fractionation have been tested for patients undergoing curative treatment: accelerated fractionation and hyperfractionation. Accelerated fractionation emerged from analyses of the control of head and neck cancer as a function of dose administered and total treatment time. Although these are discussed in detail in later chapters as part of comprehensive discussions of organ toxicity, it is worth making some general comments here from the perspective of how radiation biology relates to the clinical toxicities. The term radiation toxicity is used to describe the adverse effects caused by radiation alone and radiation plus chemotherapy. Although this latter toxicity would be better labeled as combined modality toxicity, the pattern typically resembles a more severe form of the toxicity produced by radiation alone. Adverse effects from radiation can be divided into acute, subacute, and chronic (or late) effects. Acute effects tend to occur in organs that depend on rapid self-renewal, most commonly the skin or mucosal surfaces (oropharynx, esophagus, small intestine, rectum, and bladder). This is due to radiation-induced cell death that occurs during mitosis, so that cells that divide rapidly show the most rapid cell loss. It seems likely that normal tissue stem cells are relatively resistant to radiation compared with the more differentiated cells, because these stem cells survive to permit the normal mucosa to reepithelialize. Acute side effects typically resolve within 1 to 2 weeks of treatment completion, although occasionally these effects are so severe that they lead to consequential late effects, as described later. Because lymphocytes are exquisitely sensitive to radiation, there has been considerable investigation into the effects of radiation on immune function. In contrast to mucosal cell killing, which requires mitosis, radiation kills lymphocytes in all phases of the cell cycle by apoptosis, so that lymphocyte counts decrease within days of initiating treatment. These effects do not tend to put patients at risk for infection, because granulocytes, which are chiefly responsible for combating infections, are relatively unaffected. Two acute side effects of radiation do not fit neatly into these models relating to cell kill: nausea115,116 and fatigue. Nausea is usually associated with radiation of the stomach, but it can sometimes occur during brain irradiation or from large-volume irradiation that involves neither the brain nor the stomach. Irradiation typically produces fatigue, even if relatively small volumes are irradiated. It seems likely that the origins of both of these abscopal effects of radiation. Radiation can also produce subacute toxicities in the form of radiation pneumonitis and radiation-induced liver disease. The risk of radiation pneumonitis and radiation-induced liver disease is proportional to the mean dose delivered. Attempts to determine the genomic basis of radiation sensitivity, beyond the known rare genetic defects such as ataxia telangiectasia, have not yet been successful. Two theories for the origin of late effects have been put forth: late damage to the microvasculature and direct damage to the parenchyma. Although the vascular damage theory is attractive, it does not account for the differing sensitivities of organs to radiation. Late complications can also be divided into two categories: consequential and true late effects. The best example of a consequential late effect is fibrosis and dysphagia after high-dose chemoradiation for head and neck cancer. Here, late fibrosis or ulceration appears to be the result of the mucosa becoming denuded for a prolonged time period. Late consequential effects are distinct from true late effects, which can follow a normal treatment course of self-limited toxicity and a 6-month or more symptom-free period. Examples of true late effects are radiation myelitis, radiation brain necrosis, and radiation-induced bowel obstruction.
© 2025 Adrive Pharma, All Rights Reserved..