General Information about Serophene
Serophene is primarily used for treating ovulatory dysfunction in girls who're struggling to conceive. It is prescribed for girls who usually are not ovulating or have irregular ovulation cycles, which may forestall pregnancy. This drug works by growing the levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estrogen in the physique. These hormones are needed for the development and release of eggs from the ovaries, increasing the possibilities of being pregnant.
Like any medicine, Serophene can have potential unwanted effects. The most typical unwanted effects skilled by girls taking this drug embrace sizzling flashes, headaches, temper swings, breast tenderness, nausea, and bloating. These unwanted aspect effects are normally mild and resolve on their own. In rare circumstances, Serophene can lead to extra extreme unwanted effects, such as ovarian hyperstimulation syndrome (OHSS), which may cause severe pain and swelling in the stomach, shortness of breath, and decreased urination. OHSS is a rare but serious situation that requires quick medical consideration.
It is crucial to notice that Serophene can improve the chances of having twins or multiples, which might come with potential problems during being pregnant and childbirth. This risk is comparatively low, around 5-10%, however it is nonetheless essential to debate with the physician and pay consideration to the potential consequences.
Serophene, also recognized as Clomiphene, is a drugs generally used for treating female infertility. This drug is a selective estrogen receptor modulator (SERM) and works by stimulating the production of hormones which may be important for ovulation. In this article, we will explore the makes use of, mechanism of motion, and potential unwanted facet effects of Serophene.
In conclusion, Serophene is a useful drug in the remedy of female infertility. It works by stimulating ovulation, increasing the probabilities of conception. While it can have some potential unwanted aspect effects, they're often delicate and manageable. Women who have been battling ovulation-related infertility can profit from Serophene, however it's important to use it under the supervision of a physician to attenuate potential dangers.
Serophene is a prescribed medication and will solely be used underneath a doctor's supervision. Women who're pregnant, have liver illness, or have a history of blood clots shouldn't take this medicine. Certain drugs, corresponding to anti-estrogens, may interact with Serophene, so it's crucial to tell the doctor of some other medicines being taken.
Serophene is taken orally, usually starting on the third, fourth, or fifth day of the menstrual cycle. The dosage may range relying on the person's response and the physician's recommendation. A typical remedy cycle with Serophene lasts for 5 days, and a lady is suggested to have intercourse across the time of ovulation, which is often 5 to 9 days after the final dose. The doctor could monitor the remedy with blood checks and ultrasounds to verify for ovulation and regulate the dosage accordingly.
The effectiveness of Serophene varies relying on the underlying explanation for infertility. It is handiest in girls who have polycystic ovary syndrome (PCOS), a hormonal dysfunction that affects ovulation. Studies have proven that Serophene has helped about 80% of women with PCOS to ovulate, and approximately 40% to 45% have gone on to turn into pregnant. It can be useful for girls with ovulation problems due to other causes, corresponding to weight-related issues, thyroid dysfunction, or hypothalamic amenorrhea.
The mucosa in the region of the frontonasal ostium is inverted nasally menopause 8 months no period 50 mg serophene purchase with amex, and the drainage opening is blocked with pinna conchal cartilage on one side covered by overlapping perichondrium and fixed with fibrin glue. Through this three-layered closure, the frontal sinus is securely isolated from the nasal cavity and the ethmoidal cells, respectively, and growth of mucosa into the sinus with the associated risk of mucocele formation is prevented. Abdominal harvested fat is placed by pieces into the frontal sinus, held together with fibrin glue, until the sinus cavity is completely filled. Finally, the periosteal bone lid is replaced and fixed with absorbable threads, wire sutures, or miniplates. At the end of the operation, the scalp flap is flipped back into place, two suction drainages are inserted, and the coronal incision is closed with single-stitch sutures. If reconstruction of the bony forehead is needed, many different grafts and implants can be used. There are autogenous bone and cartilage grafts, such as rib, scapula, iliac crest, calvarial bone (inner and outer table), and calvarial bone pedicled at the temporalis muscle. There are also alloplastic materials, such as titanium mesh or plates, polymethyl methacrylate, porous polyethylene, ceramic (hydroxyapatite, carbonated apatite), and biocement (Bioverit). In our experience, autogenous calvarial bone has been proven to be the most suitable material for the anterior frontal sinus wall. Usually, the graft is taken more anteriorly and medially if a flat portion of bone is required, and more laterally and posteriorly if a curvilinear piece is needed. For the transfer of calvarial bone grafts, three techniques exist: splitthickness calvarial graft, single-table calvarial graft, and calvarial bone flap. Patients should be followed at 3-month intervals in the first year to examine for instability, resorption, and infection of the reconstructed region. Indications Malignant anterior skull base tumors without and with intradural extension. Complications Infection of the calvarial graft has been reported as occurring in 1. The periorbit is dissected from superior, medial, and lateral walls and can be exposed back to the apex. The outline of the opening needs to be planned depending on the size of the frontal sinus and the extent of the tumor. Osteotomies are performed by an oscillating saw across the frontal bone, down to and along the orbital roofs, down the medial orbital wall, and along the nasomaxillary grooves just anterior to the lacrimal crest. Using chisels, the nasofrontal segment, including the whole frontal sinus, is elevated under direct vision, freeing the dura. Therefore, the dura over both frontal lobes is incised, followed by ligation of the sagittal sinus and dissection of the falx cerebri, which is finally cut. Subsequently, one has a good view over the olfactory grove with both olfactory bulbs and the tumor. With frontal lobe protection by surgical dressing, exposure can be extended down to the optic chiasm. Tumor removal is then performed by osteotomies of the anterior skull base laterally at the junction to the orbital roof and caudally at the planum sphenoidale under direct vision and protection of the Subcranial Approach According to Raveh the subcranial approach was first introduced by Raveh et al for treatment of traumatic disruption of the anterior skull base and published in 1981. This is accomplished by dural detachment from below with practically no frontal lobe retraction, the avoidance of facial incisions, and adequate dealing with the paranasal sinuses, especially cranialization of the frontal sinus. Caudal and lateral tumor extensions involving the nasal cavity, maxillary sinus, soft palate, and epipharynx are exposed by the same subcranial anterior route, obviating the need for conventional transfacial approaches, such as lateral rhinotomy and midfacial degloving. After complete exposure, osteotomies, and intracranial dissection, tumor removal can be achieved en bloc rather than in a piecemeal fashion. For reconstruction of the skull base defect, we recommend several layers of fascia lata (at least two, best three). The first layer of the simultaneously harvested fascia lata is tacked under the edges of the dura and carefully sutured in place. The repaired dural defect is then covered with a second layer of fascia applied against the entire undersurface of the ethmoidal roof, sella, and sphenoidale area. If the medial orbital walls have to be reconstituted, either fascia lata or Tutoplast fascia lata can be used. If the canthal ligaments have to be fixed, this can be accomplished by placing two nonabsorbable threads through both medial canthal ligaments, running underneath the nasofrontal segment. When the tumor involves the nasal bone or other fronto-orbital segments, a split calvarial bone graft can be used for reconstruction. Before replacing the osteotomized nasofrontal bone segment, the posterior frontal sinus wall is removed, as well as the mucosa of the entire frontal sinus. The bone segment is then repositioned in its original anatomical place and fixed using prebent titanium plates. The closure of the scalp is performed in the same way as the osteoplastic frontal sinus approach. Postoperative Care Postoperatively, patients are immediately transferred to the intensive care unit for 24 hours. Patients should be followed at 3-month intervals in the first year and then on a regular basis for at least 5 years. Postoperative radiotherapy or chemoradiation can start 6 weeks postoperatively at the earliest. Esthesioneuroblastoma and adenoid cystic carcinoma have the most favorable prognosis, with positive 5-year, disease-specific survival rates. However, in adenoid cystic carcinoma, the prognosis is determined mainly by distant metastases and slow perineural spread that diminish disease-specific survival to 40% after 15 years. Malignant melanomas show, along with undifferentiated carcinomas, the worst prognosis. Possibly also T3 tumors might be removable endonasally if they only superficially infiltrate the lamina papyracea and periorbit or the cribriform plate and dura, respectively. The same principle applies to T4a tumors if they have grown only marginally into the frontal sinus or have infiltrated the sphenoid sinus without major bony destruction.
After adjustment for established breast cancer risk factors seven hills womens health center trusted serophene 25 mg, these mortality ratios fell to 1. Trends in Incidence and Mortality Incidence rates of breast cancer have steadily increased in the United States since the 1930s, when formal record keeping began in Connecticut, until 2000. Increases have occurred in all age groups since 1935, although the magnitude of increase has been greater for older women. Between 1975 and 2000, incidence rates among black women younger than 50 years increased by 22% compared to a cumulative increase of 10% for white women younger than 50 years (8). Among women 50 years and older, the cumulative increase was 40% for both black and white women. Between 2001 and 2004, incidence rates of breast cancer decreased by approximately 3. Between 2005 and 2009, incidence rates among white women have remained relatively constant; while among black women incidence rates have increased. Several studies have examined whether the increase in breast cancer incidence in the United States has been due to the increasing use of screening mammography (3136). Because screening causes at most a transient increase in incidence, and because its use was limited before the 1980s, it can explain little of the long-term increase between the 1930s and the 1980s. However, during the 1980s, the Geographic Variation in the United States Breast cancer incidence and mortality rates vary within the United States, although to a much smaller degree than among countries. These findings suggest that the increase in use of screening mammography accounts for part of the recent increase in breast cancer incidence (34,37). The continued increase in breast cancer rates during the 1990s may be due in part to increased use of hormone replacement therapy, obesity, and mammography screening. Since 2005, breast cancer rates have plateaued in the United States, Canada, Australia, and parts of Europe (3). Trends in breast cancer mortality are of major public health interest, but their interpretation is complex because they reflect the combined effects of trends in underlying risk of breast cancer, changes in screening practices, and effectiveness of treatment. Also, the divergence between breast cancer incidence and mortality rates began in the United States even before the use of mammography or chemotherapy. Further, mortality rates lag behind changes in breast cancer incidence, screening, and treatment by at least 5 to 10 years (42). Age-adjusted mortality rates in the United States were relatively stable between the 1950s and the mid-1980s, when an overall decline was first noted (37). Rates through the 1990s declined somewhat more (3% decline per year) (8,43), perhaps because of enhanced treatment and screening. From 1973 to 1995, the cumulative decline in mortality rates for white women younger than 60 years has been more than 20%, with much of this decline occurring since 1988. In contrast to these trends among younger white women, mortality rates for white women 60 years and older increased slowly during the 1970s and 1980s, although since the late 1980s, mortality has also begun to decline in this group (37,42). The trends in breast cancer mortality among black women have been unfavorable; between the 1970s and 1990, mortality rates increased for black women in all age groups (42), and only recently is there evidence of a decline, but to a lesser extent than what is observed in white women. Some of the recent increases in incidence in high-risk populations may be due to greater use of mammography, as in the United States. Breast cancer incidence rates have nearly doubled in recent decades in traditionally low-risk countries such as Japan (4,9) and Singapore (5) and in the urban areas of China (46). Dramatic changes in lifestyle in such regions brought about by growing economies, increasing affluence, and increases in the proportion of women in the industrial workforce have had an impact on the population distribution of established breast cancer risk factors, including age at menarche and fertility, as well as nutritional status (47). These changes have resulted in a convergence toward the risk factor profile of Western countries (47). Trends in breast cancer mortality around the world have largely paralleled the trends in incidence. Between the 1970s and 1990s mortality increased in both high-risk and lower risk populations, although since the 1990s mortality has declined moderately in the United Kingdom, the Netherlands, and Sweden, similar to the decline observed in the United States (3,48,49). As in the United States, some of the downturn in mortality in these countries may be due to more widespread use of screening mammography, adjuvant chemotherapy during the 1980s (48,50), and more recently targeted therapies (51). Countries with mortality rates that are still increasing tend to be those with the lowest mortality (48). For instance, Russian Federation, Republic of Korea, and Japan all have breast cancer mortality rates that are continuing to increase (3). Thus, a convergence of breast cancer mortality rates may be occurring internationally, in part reflecting an international convergence of reproductive and behavioral risk factors (48). Surveillance Epidemiology, and End Results Program, Cancer Incidence and Mortality Statistics. An underlying concept is that ovarian hormones initiate breast development and that subsequent monthly menstrual cycles induce regular breast cell proliferation. The onset of puberty is marked by a surge of hormones that induce regular breast cell proliferation. This pattern of cell division terminates with menopause, as indicated by cessation of ovulation and menstrual periods. The significant inverse association seen in this study may be related to the young age of the cohort and thoroughness of investigation of the cause of infertility in this group of health professionals. Pregnancy and Age at First Full-term Pregnancy Nulliparous women are at increased risk of breast cancer compared to parous women. This risk is evident after age 40 to 45 years, but not for breast cancer diagnosed at younger ages. In the majority of epidemiologic studies, a younger age at first full-term pregnancy predicts a lower lifetime risk of breast cancer (52). The reduction in risk following pregnancy compared to nulliparous women is not immediate but takes approximately 10 to 15 years to manifest (62).
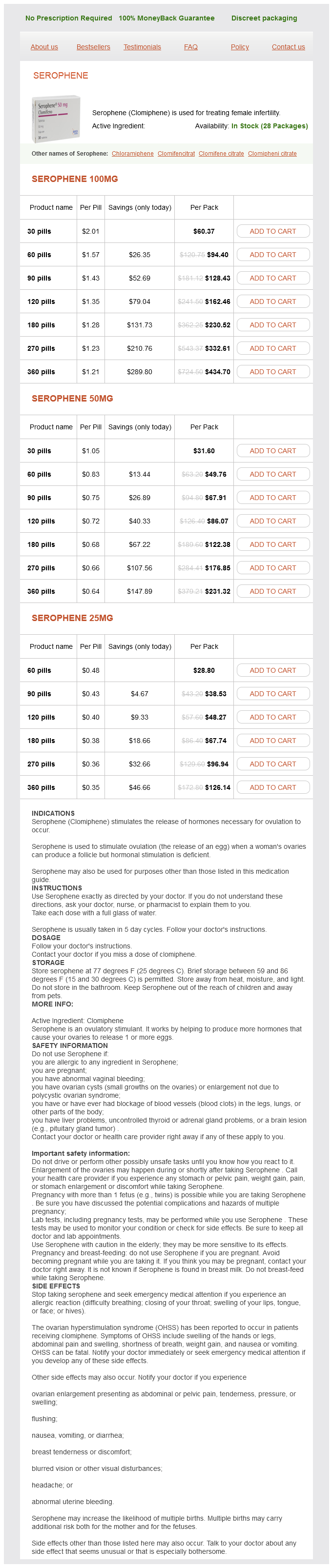
Serophene Dosage and Price
Serophene 100mg
- 30 pills - $60.37
- 60 pills - $94.40
- 90 pills - $128.43
- 120 pills - $162.46
- 180 pills - $230.52
- 270 pills - $332.61
- 360 pills - $434.70
Serophene 50mg
- 30 pills - $31.60
- 60 pills - $49.76
- 90 pills - $67.91
- 120 pills - $86.07
- 180 pills - $122.38
- 270 pills - $176.85
- 360 pills - $231.32
Serophene 25mg
- 60 pills - $28.80
- 90 pills - $38.53
- 120 pills - $48.27
- 180 pills - $67.74
- 270 pills - $96.94
- 360 pills - $126.14
Over the years breast cancer walks 2014 purchase serophene online, we have developed a protocol for orbital infection that has been adopted across the hospital. Our most recent audits have shown a substantial improvement in the quality of care. All children are admitted under the care of the otolaryngology team and treated with intravenous antibiotics, according to local microbiology advice, and nasal decongestants. The differentiation between preseptal and deep orbital cellulitis is difficult based on clinical observation, and clinical presentation may not always reflect underlying disease severity. In fact, only a minority of children are exposed to the radiation dose of a scan with this protocol. Some small abscesses may settle with conservative treatment, but this is only safe if the child is able to cooperate with regular, frequent, and detailed assessments of vision to monitor for deterioration. Orbital collections can be drained endoscopically by exenterating the ethmoids, defining the lamina papyracea, and then removing this plate of bone as widely as possible to expose the orbital periosteum. If the surgeon does not feel an endoscopic procedure is safe, external drainage via the Lynch-Howarth medial canthal incision is an option. Obviously, this has the disadvantage of a facial scar, but the advantage of an easier procedure. The ethmoids can be exenterated at the time of drainage, and the maxillary antrum can be irrigated. Children should be followed up after orbital infection, as fat necrosis in the orbit can lead to enophthalmos and diplopia. It is not unusual for them to insert foreign bodies into various orifices, including the nose. Presentation may be with a witnessed insertion or a visible foreign body, but in many cases the original insertion goes unnoticed, and presentation is with 1 to 2 weeks of foul-smelling unilateral nasal discharge. Such a discharge is almost always due to a foreign body, although in rare cases it can be due to persistent sinus infection or unilateral choanal atresia. Separation of the septum cartilage from the perpendicular plate has to be avoided. If necessary, resection of a crista septi or a deviating basal rim of the cartilaginous septum can be done without harming nasal development. The septospinal ligament anchors the septum in the midline and contributes to forward growth of the maxilla. The treatment of choice of a juvenile angiofibroma invading the pterygomaxillary fossa is a. None of the above Key Points · Guidelines for rhinosurgery should differentiate for children and adult patients. It should be noted that the poor wound-healing capacity of the septodorsal cartilage may intervene with restoring normal growth. Preseptal infection can be reliably distinguished from postseptal infection on clinical grounds. Which of the following is true in the management of a 13-year-old boy with recent-onset left-sided nasal obstruction, facial pain, and epistaxis Which of the following is correct in the management of congenital midline nasal dermoids A vertical incision on the nasal dorsum is the most cosmetic approach for surgery. Adolescent growth patterns of the bony cartilaginous framework of the nose: a cephalometric study. Persistent pattern of variations of the human nasal septum: implications for stress and trauma illustrated by a 20. The influence of nasal osteotomies and septum surgery on the growth of the rabbit snout. The influence of reimplantation of rotated or crushed autologous septal cartilage on nasal growth; an experimental study in rabbits. Normal and abnormal nasal growth after partial submucous resection of the cartilaginous septum. Rhinochirurgie bei Kindern: Entwicklungsphysiologische- und chirurgische Aspekte der wachsende Nase. Controlling incision-induced distortion of nasal septal cartilage: a model to predict the effect of scoring of rabbit septa. Facial Plast Surg 1986;3:225234 V Rhinology: the Multidisciplinary Interface References 661 28. Comparison of different chondrocytes for use in tissue engineering of cartilage model structures. Differences in cartilage forming capacity of expanded human chondrocytes from ear and nose and their gene expression profiles. The role of the nasopharyngeal airway for obstructive sleep apnea in syndromic craniosynostosis. Predictive factors for success after transnasal endoscopic treatment of choanal atresia. Pediatric meningoencephaloceles and nasal obstruction: a case for endoscopic repair. Role of propranolol in the therapeutic strategy of infantile laryngotracheal hemangioma. Nasal rinsing with hypertonic solution: an adjunctive treatment for pediatric seasonal allergic rhinoconjunctivitis. Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: systematic review of randomised controlled trials. Intranasal corticosteroids versus topical H1 receptor antagonists for the treatment of allergic rhinitis: a systematic review with meta-analysis. Long-lasting effect of sublingual immunotherapy in children with asthma due to house dust mite: a 10-year prospective study. Optimal management of nasal congestion caused by allergic rhinitis in children: safety and efficacy of medical treatments. A review of outcomes following inferior turbinate reduction surgery in children for chronic nasal obstruction.
© 2025 Adrive Pharma, All Rights Reserved..