General Information about Seroflo
When utilizing Seroflo, it is essential to comply with the prescribed dosages and directions from a healthcare professional. Some widespread unwanted side effects similar to headache, sore throat, and nausea may occur, but these are normally mild and momentary. In uncommon circumstances, more severe unwanted effects corresponding to problem breathing, chest ache, or irregular heartbeat might happen, in which case quick medical consideration should be sought.
Seroflo has shown to be extremely effective in stopping and treating asthma attacks. In addition to its long-acting results, it also helps to minimize back the necessity for different drugs that sufferers could also be taking to control their signs. This can considerably enhance the quality of life for individuals affected by bronchial asthma, as they will go about their day by day activities without being restricted by their condition.
In conclusion, Seroflo is a extremely effective treatment for the prevention and remedy of asthma and other chronic respiratory conditions. Its mixture of two lively components offers long-lasting aid for sufferers and improves their general quality of life. With correct usage and monitoring, Seroflo helps individuals to handle and control their signs, allowing them to lead a more active and fulfilling life.
Fluticasone is a synthetic corticosteroid that works by reducing inflammation and swelling in the airways. It helps to stop bronchial asthma attacks and reduces the frequency and severity of signs corresponding to wheezing, coughing, and shortness of breath. Salmeterol on the other hand, is a long-acting beta-agonist that helps to open up the airways by enjoyable the muscular tissues round them. This allows the particular person to breathe extra easily, especially throughout an asthma assault.
Moreover, Seroflo is appropriate for both youngsters and adults, making it a reliable choice for the entire household. It can be out there in different strengths, permitting for personalized dosages depending on the severity of the situation. This makes it an efficient treatment possibility for a variety of patients with numerous respiratory conditions.
Seroflo is a novel combination of those two medications, providing a powerful and helpful therapy choice for patients with chronic respiratory conditions. It is especially useful for many who have difficulty managing their signs with only one medicine or for many who need frequent rescue inhaler use.
One of the key advantages of Seroflo is its long-acting effects. Unlike most inhalers which have short-term benefits, Seroflo can provide aid for as a lot as 12 hours after a single dose. This implies that sufferers can use it twice a day, once within the morning and as quickly as in the evening, to maintain their signs beneath control all through the day and evening. This helps in offering a consistent and convenient treatment for those with busy schedules.
Seroflo is a medicine that mixes two energetic ingredients, Fluticasone and Salmeterol, in an inhaler form. It is usually used for the prevention and remedy of asthma and chronic lung ailments. This inhaler supplies efficient aid for individuals who suffer from respiratory issues, permitting them to manage and management their signs.
Leukocytes allergy shots hurt generic seroflo 250 mcg overnight delivery, in particular neutrophils, provide the first line of defense during acute inflammation. In this chapter, we analyze the structure and function of primary and secondary lymphoid organs and their involvement in general and specific defensive actions. Components of the lymphatic system the lymphatic system includes primary and secondary lymphoid organs. We discussed in Chapter 6, Blood and Hematopoiesis, that hematopoietic stem cells divide to produce two specialized stem cells: lymphoid stem cell, which generates B and T lymphocytes, and a myeloid stem cell, which gives rise to leukocytes, erythrocytes, megakaryocytes, and macrophages. B lymphocytes (B cells) differentiate in the bone marrow, When activated outside the bone marrow, B cells differentiate into antibody-secreting plasma cells. T lymphocytes (T cells) differentiate in the thymus into cells that can activate other cells of the immune system (helper cells) or kill bacteria- or virus-infected cells (cytolytic or cytotoxic cells). Major cells participating in immune reactions B cells Lymphocytes Bone-marrow derived Differentiate in bone marrow Helper T cells T cells Bone marrow-derived Differentiate in the thymus Cytolytic T cells Macrophages Monocyte-derived Accessory cells (Antigen-presenting cells) Dendritic cells Monocyte-derived Follicular dendritic cells Lymph node-derived 4. The lymphatic system is widely distributed because pathogens can enter the body at any point. The main function of the lymphoid organs, as components of the immune system, is to protect the body against invading pathogens or antigens (bacteria, viruses, and parasites). The basis for this defense mechanism, or immune response, is the ability to distinguish self from nonself substances. T cells, subdivided into two categories: helper T cells and cytolytic or cytotoxic T cells. T cells Box 10-A Toll-like receptors respond to cell-bound antigens presented by specific molecules. After leaving the two primary organs (bone marrow and thymus), mature B and T cells circulate in the blood until they reach one of the various secondary lymphoid organs (lymph nodes, spleen, and tonsils). B and T cells can leave the bloodstream through specialized venules called high endothelial venules, so called because they are lined by tall endothelial cells instead of the typical squamous endothelial cell type. The accessory cells include two monocyte-derived cell types: macrophages and dendritic cells. An example of a dendritic cell is the Langerhans cell found in the epidermis of the skin. A third type, the follicular dendritic cell, is present in lymphatic nodules of the lymph nodes. Follicular dendritic cells differ from ordinary dendritic cells in that they do not derive from a bone marrow precursor. Before we start our discussion of the origin, differentiation, and interaction of lymphocytes and accessory cells, we need to define the characteristics of the immune system. Then, we will be able to integrate the structural aspects of each major lymphatic organ with the specific characteristics of the immune responses. Innate or natural immunity of the newborn is the simplest mechanism of protection. It does not require previous exposure to a pathogen and elicits rapid responses by macrophages and dendritic cells. We discuss later in this chapter that the complement system, consisting of serum proteins, membrane-bound regulators and receptors, is also a key mechanism of innate defense triggered rapidly upon infection. Adaptive or acquired immunity develops when an individual is exposed to a pathogen with the aims of eliminating the pathogen as well as the generation of immunologic memory. Types of immunity Innate or natural immunity (Toll-like receptors and complement system) Immunity Humoral immunity (antibody-mediated: plasma cells) Adaptive or acquired immunity Cell-mediated immunity (T cells, B cells and antigen-presenting cells) nity conferred by serum or lymphocytes transferred from an immunized individual to another individual who has not been exposed or cannot respond to a pathogen. The transfer of maternal antibodies to the fetus is a form of passive immunity that protects newborns from infections until they can develop active immunity. Properties of adaptive or acquired immunity Acquisition of immunity Passive immunity Maternal antibodies transferred across the placenta to fetus Antibodies of immunized animals (rabies, tetanus) Antitoxins (diphtheria) Active immunity (post disease) T cells necessary to select lymphocytes (clonal selection) from a vast repertoire of cells bearing antigen-specific receptors generated by a mechanism known as gene rearrangement. You can regard adaptive immunity as the perfection of innate or natural immunity because it recognizes vital components of the microorganism utilizing a limited number of pattern-recognition receptors expressed on all cells of a given type (nonclonal) and independent of immunologic memory. Adaptive or acquired immunity involves two types of responses to an antigen (or pathogen): 1. The first response is mediated by antibodies produced by plasma cells, the final differentiation product of B cells as we have seen in Chapter 4, Connective Tissue. This response is known as humoral immunity and operates against antigens located outside a cell or bound to its surface. When antibodies bind to an antigen or toxins produced by a pathogen, they can facilitate the phagocytic action of macrophages or recruit leukocytes and mast cells to take advantage of their cytokines and mediators, respectively, and strengthen a response. Humoral immunity results in persistent antibody production and production of memory cells. An intracellular pathogen is not accessible to antibodies and requires a cellmediated response, or cell-mediated immunity. T cells, B cells, and antigen-presenting cells are the key players in cell-mediated immunity. A consequence of adaptive or acquired immunity is the protection of the individual when a second encounter with the pathogen occurs. This protection is specific against the same pathogen and, therefore, adaptive or acquired immunity is also called specific immunity. Passive immunity is a temporary form of immu- Both humoral and cell-mediated immunity developed against foreign pathogens have the following characteristics: 1.
The hard palate is lined by a keratinizing stratified squamous epithelium similar to that of the free margins of the gums allergy symptoms red skin purchase seroflo with amex. A submucosa is present in the midline but absent in the area adjacent to the gums. Collagenous fibers in the submucosa bind the mucosa to the periosteum of the hard palate, enabling the mucosa to resists shear forces and compression. Areas of fat and glandular tissue cushion the mucosa to protect nerves and blood vessels of the hard palate. The soft palate and uvula are lined by a nonkeratinized stratified squamous epithelium extending into the oropharynx where it becomes continuous with the pseudostratified ciliated columnar epithelium of the upper respiratory tract. Tongue the anterior two thirds of the tongue consist of a core mass of skeletal muscle oriented in three directions: longitudinal, transverse, and oblique. The posterior one third displays aggregations of lymphatic tissue, the lingual tonsils. The dorsal surface of the tongue is covered by a specialized mucosa consisting of a nonkeratinized stratified squamous epithelium supported by a lamina propria associated with the muscle core of the tongue. Their ducts open into the crypts and furrows of the lingual tonsils and circumvallate papillae, respectively. Each lingual papilla is formed by a highly vascular connective tissue core and a covering layer of stratified squamous epithelium. Foliate papillae (leaf-shaped), rudimentary in humans but well developed in rabbits and monkeys. Taste buds are barrel-shaped epithelial structures containing chemosensory cells called gustatory receptor cells. Gustatory receptor cells are in synaptic contact with the terminals of the gustatory nerves. Circumvallate papillae are located in the posterior part of the tongue, aligned in front of the sulcus terminalis. The circumvallate papilla occupies a recess in the mucosa and, therefore, it is surrounded by a circular furrow or trench. The sides of the circumvallate papilla and the facing wall of furrow contain several taste buds. Each taste bud, depending on the species, consists of 50 to 150 cells, with its narrow apical ends extending into a taste pore. Precursor cells give rise to supporting cells (or immature taste cells) which, in turn, become mature taste receptor cells. The basal portion of a taste receptor cell makes contact with an afferent nerve terminal derived from neurons in the sensory ganglia of the facial, glossopharyngeal, and vagus nerves. The taste receptor cell has neurotransmitter-containing vesicles in the basal region of the cytoplasm. Basal cells give rise to immature taste, or supporting, cells that mature into the functional mature taste cells. Depolarization causes an action potential and the release neurotransmitter that activate gustatory afferent nerve terminals. The facial nerve carries the five taste sensations; the glossopharyngeal nerve carries sweet and bitter sensations. When a sweet tastant diffuses through the taste pore of a taste bud, it interacts with type 1 receptors (designated T1R) present in the apical microvilli of the taste receptor cells. An influx of Na+ within taste cells causes depolarization of the taste receptor cells. The salty taste of Na+ is detected by direct influx of Na+ through membrane ion channels to depolarize the plasma membrane. The pulp chamber opens at the apical foramen into the bony alveolar process by the root canal. Blood vessels, nerves, and lymphatics enter and leave the pulp chamber through the apical foramen. Secreted signaling molecules, activin A, fibroblast growth factor, and bone morphogenetic proteins, mediate the interaction between the dental epithelium and the mesenchyme during tooth morphogenesis. The permanent dentition is preceded by a set of 20 deciduous teeth, also called milk or baby teeth. Deciduous teeth appear at about 6 months of age and the entire set is present by age 6 to 8 years. The deciduous teeth are replaced between ages 10 and 12 by the 32 permanent teeth. Each of the several types of teeth has a distinctive shape and function: incisors are specialized for cutting; canines, for puncturing and holding; and molars, for crushing. The outer surface of the root is covered by another calcified tissue called cementum. The dentin forms the bulk of the tooth and con- Odontoblasts differentiate from mesenchymal cells of the dental papilla under the control of the inner enamel epithelium. Odontoblasts are active secretory cells that synthesize and secrete type I collagen and noncollagenous material, the organic components of the dentin. The apical cell domain is embedded in predentin, a nonmineralized layer of dentin-like material. The apical domain projects a main apical cell process that becomes enclosed within a canalicular system just above the junctional complexes linking adjacent odontoblasts. A well-developed rough endoplasmic reticulum and Golgi apparatus as well as secretory granules are found in the apical region of the odontoblast. When procollagen is released from the odontoblast, it is enzymatically processed to tropocollagen, which aggregates into type I collagen fibrils.
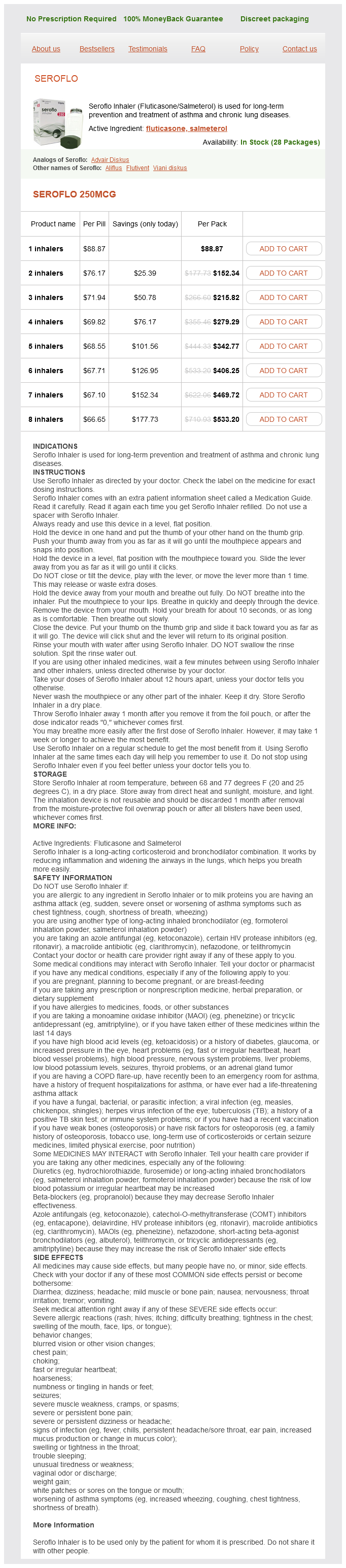
Seroflo Dosage and Price
Seroflo 250mcg
- 1 inhalers - $88.87
- 2 inhalers - $152.34
- 3 inhalers - $215.82
- 4 inhalers - $279.29
- 5 inhalers - $342.77
- 6 inhalers - $406.25
- 7 inhalers - $469.72
- 8 inhalers - $533.20
The X-linked form of this disease is caused by a mutation of a gene encoding a membrane protein of peroxisomes allergy treatment on the nhs purchase seroflo with american express. Development of unmyelinated nerves Unmyelinated nerve fibers Some axons are unmyelinated. Each Schwann cell is able to house a number of axons occupying individual invaginations of its cytoplasm. With such an arrangement, the Schwann cell cannot wrap around individual axons and no myelin is produced. The entire axolemma of such axons is freely exposed to the interstitial tissue, and axons are partially protected by a basal lamina surrounding the supportive Schwann cell. Nerve impulses along these axons travel continuously and, therefore, less rapidly than saltatory conduction. A typical pathologic finding is the presence of symmetrical demyelinated lesions in the central pons. Virus-induced demyelination can be observed in progressive multifocal encephalopathy caused by an opportunistic viral infection of oligodendrocytes in patients with immunodeficiency. Pathogenesis of multiple sclerosis Myelinated axons stained blue with Luxol fast blue Myelin Multiple sclerosis Multiple sclerosis is a demyelinating disorder characterized by episodes of neurologic dysfunction, separated in time, caused by lesions of the white matter, separated in space. Two reactive astrocytes (Creutzfeldt cells) with several nuclear fragments are seen (hematoxylineosin, H&E). Pathology: Neurodegenerative diseases Degenerative processes of specific groups of neurons of the brain cause movement disorders, dementia syndromes, and autonomic perturbations. Axonal transport defects caused by microtubule disorganization and increased phosphorylation of neurofilaments prevent binding of motor proteins for cargo transport. Consequently, accumulation of vesicles, mitochondria and neurofilaments in the perikaryon determines neuronal dysfunction and axonal atrophy. Amyotrophic lateral sclerosis Normal spinal cord (hematoxylin-eosin stain) Central canal Dorsal horn Gray matter Dorsal root ganglion Dorsal root ganglion Amyotrophic lateral sclerosis (Luxol fast blue stain) From Damjanov I, Linder J: Pathology: A Color Atlas, St. Demyelinization Symmetrical loss of myelinated fibers in a section of spinal cord (crossed cerebrospinal tracts) from a patient with amyotrophic lateral sclerosis. In addition, axonal transport defects, caused by microtubule disorganization and increased phosphorylation of neurofilaments, prevent binding of motor proteins for cargo transport. Consequently, vesicles, mitochondria and neurofilaments accumulate in the perikaryon determining neuronal dysfunction and axonal atrophy. The clinically signs are overactive tendon reflexes, Hoffmann sign (digital reflex: flexion of the terminal phalanx of the thumb following nipping of the nail), Babinski sign (extension of the great toe and abduction of the other toes after plantar stimulation), and clonus (Greek klonos, a tumult; muscle contraction and relaxation of a muscle in rapid succession). Lateral sclerosis refers to the hardness to palpation of the lateral columns of the spinal cord in autopsy specimens. Lateral sclerosis is caused by an increased number of astrocytes (astrocytic gliosis) following the degeneration and loss of motor neurons. They are involved in regulated intramembrane proteolysis: membrane proteins first shed their ectodomains by membrane-anchored proteases (sheddases), releasing the extracellular domains. Then, the membrane-retained fragment can be cleaved within the transmembrane domains to release hydrophobic peptides (such as amyloid-) into the extracellular space. The accumulation of plaques in the extracellular space consisting of amyloid (Greek amylon, starch; eidos, resemblance) fibrils containing -amyloid (A) peptide. Historically, amyloidosis was observed in the mid19th century as iodide or Congo redstained deposits in organs of patients who died from this condition. Amyloid fibrils represent the loss of function of normally soluble, functional peptide and proteins as well as the self-assembly of toxic intermediates. Keep in mind that the protective mechanisms against amyloid formation include the housekeeping ubiquitinproteasome and autophagy systems, which prevent the formation and accumulation of misfolded and aggregated polypeptide chains. Soluble tau and microtubule associated proteins Cyclin-dependent kinase 5 Microtubule Destabilized microtubules impair axonal transport 256 8. Microglial phagocytosis signaling Removal of dying or dead neurons by apoptosis or necrosis during development, inflammation, and neuropathologic conditions involve the phagocytic activity of microglial cells, the resident macrophages of the brain and spinal cord. Microglial cells sense phagocytosis recognition signals, such as phospholipid phosphatidylserine translocated by phosphatidylserine translocases from the inner leaflet of the plasma membrane to the cell surface. Phosphatidylserine marks stressed, dying or dead neurons for removal, thus enabling microglial receptors and opsonins to engulf whole dead neurons or parts of stressed neurons within hours. Microgliosis is the massive microglial response to tissue damage that can be reparative or destructive (called reactive microgliosis). In addition, vascular injury (ischemia) and parenchymal inflammation (activated microglia and reactive astrocytes) enhance the effects of A peptidecontaining plaques in the brain. Alterations in the stabilizing function of tau, a microtubule-associated protein, result in the accumulation of twisted pairs of tau in neurons. In normal neurons, soluble tau promotes the assembly and stability of microtubules and axonal vesicle transport. It is characterized clinically by parkinsonism, defined by resting tremor, slow voluntary movements (hypokinetic disorders), and movements with rigidity. This disease is pathologically defined by a loss of dopaminergic neurons from the substantia nigra and elsewhere. Ependyma and choroid plexus Choroid plexus Choroid epithelium, formed by cuboidal cells linked by tight junctions with apical microvilli, infolding of the basal plasma membrane, and abundant mitochondria. Lumen (third ventricle) Ependymal epithelium, formed by cuboidal cells linked by desmosomes, with apical microvilli and cilia and abundant mitochondria.
© 2025 Adrive Pharma, All Rights Reserved..