General Information about Secnidazole
Secnidazole is an antimicrobial bactericide that belongs to the nitroimidazole class of drugs. It is an artificial spinoff of metronidazole, another commonly used antibiotic. Secnidazole has a extensive range of uses, significantly within the treatment of bacterial and protozoal infections.
In conclusion, secnidazole is an effective antimicrobial bactericide that's broadly used in the treatment of various bacterial and protozoal infections. It provides a broad spectrum of activity and is well-tolerated by most sufferers. However, it is essential to use this medication as directed and full the full course of remedy to make sure successful restoration. As with any treatment, people ought to seek the assistance of their healthcare supplier before starting secnidazole treatment.
One of the key benefits of using secnidazole is its excessive efficacy in opposition to multiple kinds of bacteria and protozoa. This makes it a versatile antibiotic and a very good choice for treating numerous infections. Secnidazole also has an extended half-life in comparison with different antibiotics, that means that it stays within the physique for an extended period, permitting for much less frequent dosing.
Intestinal amoebiasis, also recognized as amoebic dysentery, is another situation for which secnidazole is regularly prescribed. This an infection is brought on by the protozoan species Entamoeba histolytica and is frequent in creating international locations with poor sanitation. Secnidazole has proven to be highly efficient in treating intestinal amoebiasis, as it targets and kills the parasite responsible for the infection.
One of the principle uses of secnidazole is within the treatment of urogenital infections such as urethritis and vaginitis. These circumstances are attributable to micro organism or protozoa infecting the urinary or reproductive tracts. Secnidazole works by inhibiting the growth and unfold of these microorganisms, ultimately leading to their elimination and the resolution of symptoms.
Another situation that secnidazole is prescribed for is giardiasis, a typical diarrheal illness attributable to the protozoan Giardia lamblia. This an infection can be prevalent in areas with poor sanitation and can be simply transmitted by way of contaminated water or meals. Secnidazole is an effective treatment possibility for giardiasis, because it targets and eliminates the parasite from the digestive tract.
In addition to intestinal amoebiasis, secnidazole can be generally used within the treatment of liver amoebiasis. This much less widespread form of amoebic infection is brought on by the identical protozoan species however impacts the liver as an alternative of the intestines. Secnidazole, along with other drugs, is usually used to eradicate the parasite from the liver and prevent additional damage.
It is important to take secnidazole as prescribed for the total length of treatment, even if symptoms enhance. This ensures full eradication of the an infection and helps stop the event of antibiotic resistance. It can be necessary to note that secnidazole does not protect in opposition to sexually transmitted infections, and extra measures ought to be taken to stop their unfold.
Secnidazole is mostly well-tolerated, with few reported unwanted aspect effects. Common unwanted effects embrace nausea, vomiting, and complications. However, these are sometimes mild and resolve on their own. In some rare circumstances, extra severe unwanted effects corresponding to allergic reactions might occur, and patients ought to seek medical consideration if these occur.
The second symptoms yeast infection women order secnidazole 1 gr visa, and most commonly used diagnostic criteria were established in 2003 entitled the Rotterdam criteria and were defined as any two of the three following: oligo and/or anovulation, clinical and/or biochemical signs of hyperandgrogenism, and polycystic ovaries [7]. As noted in the introduction, the Rotterdam criteria are the most commonly utilized diagnostic criteria, though it is recommended to always clearly define the criteria used in research studies. As more research into the syndrome is undertaken and our understanding advances, so too the definition will likely continue to evolve. Polycystic ovaries are ubiquitous and are often found in normal women of younger age [40]. This morphology is primarily established through transvaginal ultrasound and has been defined based on the Rotterdam criteria as the presence of at least 12 follicles measuring 29 mm within a single ovary or ovarian volume greater than 10 mL. This has been colloquially described as a "black pearl necklace" secondary to the often times peripheral location of the preantral follicles with increased amounts of central ovarian stroma. They first noted an amalgam of symptoms including obesity, hirsutism, and chronic anovulation, but since then we have adopted both biochemical and radiographic imaging to assist in diagnosis [3]. Ethnic, and presumably underlying genetic, differences in population may result in the presence of hyperandrogenenemia without clinical signs of hyperandrogenism [55]. The ovary is the preferential source of testosterone, and it is estimated that 75% of circulating testosterone originates from the ovary (mainly through peripheral conversion of prohormones by liver, fat, and skin, but all through direct ovarian secretion). Androstenedione, of both adrenal (50%) and ovarian (50%) origin, is the only circulating androgen that is higher in premenopausal women than in men, yet its androgenic potency is only 10% of testosterone. A circulating total testosterone level was found to be the best hormonal correlate of the combined syndrome of hyperandrogenic chronic anovulation and polycystic ovaries [57]. However, good correlations and similar precision have been noted between these assays [60]. After puberty and stimulated by the increased androgens, some of these hairs (mainly midline hair) are transformed into coarser, pigmented terminal hairs. A similar mechanism may explain the increase in acne with puberty, with increased sebum production by the sebaceous glands. One of the central paradoxes is that androgens can exert opposite effects (vellus to terminal, terminal to vellus), depending on the site of the hair follicle [61]. It is important to note that factors other than androgen action may contribute to the development of hirsutism. Hirsutism and acne, however, are heterogeneous and common disorders, similar to polycystic ovaries. There are, for instance, ethnic differences in target tissue sensitivity to circulating androgens and intracellular androgens [64], such that marked androgen excess may not manifest as hirsutism [55]. Methodology of the assessment of hirsutism and response to treatment have been poorly validated [65]. Hirsutism scores are notoriously subjective [66], though further evaluation has shown an acceptable agreement among well-trained independent observers [67]. Even the most frequently utilized standard of subjective hirsutism scores, the modified Ferriman-Gallwey score, relies excessively on nonmidline, nonandrogen dependent body hair to make the diagnosis [68], though this is considered the gold standard [69]. A sum of these 9 scores with a value greater than 8 is generally used as the cutoff indicative of hirsutism, though ethnic differences make this poorly generalizable. Also, hirsutism is frequently idiopathic and accompanied by normal circulating androgen levels [64], although other studies with more thorough examination have shown idiopathic hirsutism to be rare (<10% of a hirsute population) [71]. The cause of this vaginal bleeding may be physiologic (postovulatory withdrawal bleed) or pathologic. How infrequent should the menstrual bleeding be to qualify as "chronic anovulation" and how do you classify persistent anovulatory bleeding There is no consensus here, but general guidelines are 68 spontaneous episodes of vaginal bleeding per year and cycle intervals greater than 35 days is considered prolonged. One of the most common prevailing theories about the etiology of type 2 diabetes proposes that the primary pathogenetic defect is peripheral insulin resistance, resulting in compensatory hyperinsulinemia. Over time there is beta cell dysfunction, leading to inadequate secretion of insulin and ultimately to beta cell exhaustion, and the development of frank type 2 diabetes. There are data supporting hyperinsulinemia as a potential cause and treatment strategy of hyperandrogenemia V. This theory is further validated in studies that have attempted to correct hyperinsulinemia and observe the downstream effects, which have shown improvement. The largest study to date evaluating correction of hyperinsulinemia showed an improvement in ovulation rate and clinical signs of hirsutism [70]. A large meta-analysis showed an improvement of induced ovulation with treatment of the insulin resistance with metformin with an odds ratio of 3. In a Cochrane database systematic review evaluating multiple types of insulin sensitizing agents, they showed these medications were successful in improving insulin sensitivity and reduced hyperandrogenemia [79]. HbA1c is a hematologic test used to detect the average glycemic index of a red blood cell over a 3-month period. It is currently used as a measure of chronic glycemic control in diabetes treatment, but also in the diagnosis of prediabetes (HbA1c > 5. At steady state, the amount of glucose infused is equal to the amount of glucose utilized by the tissues and can be used as an index of sensitivity to insulin. The more glucose that is infused, the greater the sensitivity to insulin and vice versa. In this test, a bolus injection of glucose is given and blood is very frequently sampled for glucose and insulin levels. Minimal model analysis is then applied to the glucose and insulin levels obtained, and an insulin sensitivity index is derived.
Nonetheless medications 1800 order secnidazole line, with stringent quality control and confirmation of stenosis by an independent observer (see later), duplex sonography is now the most common way that carotid stenosis severe enough to warrant surgery is diagnosed. There are no standard and commonly used definitions for the ultrasound appearance of plaques (soft, hard, calcified, etc. Therefore, although unstable and ulcerated plaques are more likely to be symptomatic than stable plaques with fibrous caps, the ultrasound inaccuracy compromises any study of the relationship between plaque characteristics on duplex sonography and the risk of later stroke, and so the selection for carotid surgery. Despite all these limitations, duplex sonography is a remarkably quick and simple investigation in experienced hands, and it is neither unpleasant nor risky. Very rarely, the pressure of the Doppler probe on the carotid bifurcation can dislodge thrombus, or cause enough carotid sinus stimulation to lead to bradycardia or hypotension. The same conceivably applies to the various arterial compression maneuvres that may be carried out during transcranial Doppler or extracranial Doppler sonography, and any such compression should be avoided in patients who may have carotid bifurcation disease. Reliable duplex sonography in a laboratory with stringent quality control, with any carotid stenosis confirmed by an independent observer, is now generally the best way to diagnose stenosis that is severe enough for carotid endarterectomy to be worthwhile. It requires a large dose of intravenous contrast to outline the arterial lumen, there is Xray exposure, and may underestimate stenosis. This approach allows a rapid evaluation of cerebral perfusion by generating maps of cerebral blood volume, cerebral blood flow, time to peak, and mean transient time. Common (open arrow), internal carotid stenosis (arrow), and external carotid arteries and branches (arrowheads). The main advantage of noninvasive methods over catheter angiography is there is no serious procedural risk, and they can usually be done very quickly. Although an early systematic review of prospective studies of the risks of catheter angiography in patients (a) (b) 326 6 What caused this transient or persisting ischemic event While the stenosis is clearly "severe," it is not possible to measure its exact extent because of the "flow gap" (arrow) distal to the lesion. Also it should be noted that most studies counted all strokes that occurred within 24 hours of angiography as procedural complications. Given that the risk of stroke shortly after presentation with symptomatic carotid stenosis and prior to endarterectomy is about 0. Little is known, however, in terms of incidence and implications of silent cerebral ischemia associated with conventional angiography. In contrast to pharmaceutical products, new diagnostic or imaging strategies are not subject to stringent regulatory control, and no standards are set for validation. Given that the available techniques of carotid imaging use completely different source data to estimate stenosis, that there is major variation in carotid bifurcation anatomy between individuals, and between the sexes, translation of measurements of stenosis from one technique to another is not at all straightforward. Although several hundred studies of carotid imaging have been published over the last two decades, most are undermined by poor design, inadequate sample size, and inappropriate analysis and presentation of data. Several studies have concluded that individual noninvasive methods could not substitute for catheter angiography as the sole preendarterectomy imaging technique because of the frequency with which the degree of stenosis was misclassified [228]. However, recent work has shown that the risk of stroke is at least as high, and possibly higher in the first few weeks after the event [230]. It is not clear that vascular surgery has much to offer other than in the rather special situation of subclavian steal. However, there are an increasing number of reports of angioplasty and stenting of atherothrombotic stenoses of the vertebral or proximal basilar arteries, but this remains investigational. Although asymptomatic subclavian steal is quite common (reversed vertebral artery flow detected by ultrasound or vertebral angiography), symptomatic subclavian steal is less common, presumably because collateral blood flow to the brainstem is enough to compensate for the reversed vertebral artery blood flow distal to ipsilateral subclavian stenosis or occlusion. It is only this sort of symptomatic patient who may require surgery and therefore who has to accept the risk of any preceding angiography. Innominate artery steal is even rarer, with retrograde vertebral artery flow distal to innominate rather than subclavian artery occlusion. The goldstandard imaging used to be catheter angiography because ultrasound and other noninvasive methods were neither specific nor sensitive enough to rely on [231]. Other potential indications for angiography include suspicion of any of the following. An aneurysm of the extra or intracranial circulation large enough to contain thrombus which might embolize to the brain or eye. This is very rare, but surgery may be required to clip or remove an aneurysm, or anticoagulation might be indicated. Fibromuscular dysplasia although whether and how it should be treated is not at all clear. Cerebral vasculitis, which can be associated with beading and narrowing of cerebral arteries, although this is neither a specific nor sensitive feature. This diagnosis is better made by serological tests, extracranial tissue biopsy (renal, skin, etc. Moyamoya syndrome is exceedingly rare and any treatment possibilities are severely limited. The base of the skull looked at from above (eyes at the top of the diagram) to illustrate the transtemporal and the transforaminal cranial sonographic windows and typical waveforms obtained from the major intracranial arteries. It is very safe, although during tests involving compression of the carotid artery it is conceivable that emboli can be released from an underlying atheromatous plaque, and bradycardia can occur. However, the patient has to keep reasonably still; the examination can take as long as an hour; the skull is impervious to ultrasound in 510% of cases, more with increasing age and in females, but less if intravenous echocontrast is used; exact vessel identification may be difficult, but colorflow realtime imaging makes this easier; spatial resolution is poor; diagnostic criteria vary; and the technique is not always accurate in comparison with cerebral catheter angiography [232,233]. It is also used for monitoring during carotid endarterectomy, the diagnosis of patent foramen ovale, risk stratification and treatment in sickle cell disease, and perhaps in helping define stroke risk there are four other possible indications: display of intracranial arterial occlusion and stenosis; assessment of cerebrovascular reactivity; and acceleration of clot lysis following treatment with a thrombolytic agent in acute ischemic stroke [235]. However, at present, this information is of limited clinical relevance although it may aid in selection of patients for recanalization. Emboli detection Transcranial Doppler sonography can also be used to assess cerebrovascular reactivity, i.
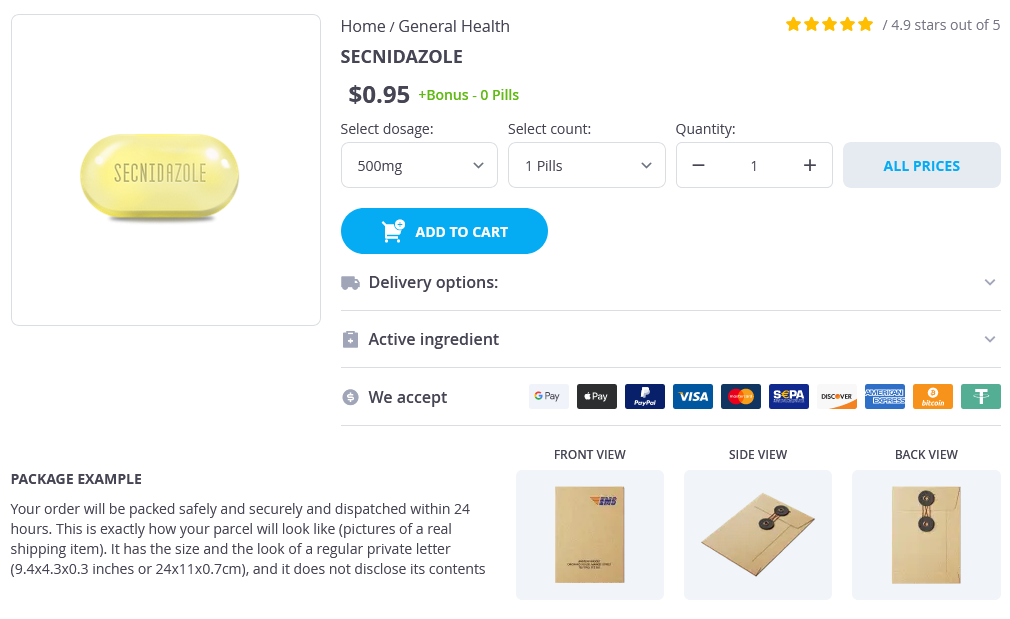
Secnidazole Dosage and Price
Secnidazole 500mg
- 1 pills - $1.05
Secnidazole 1gr
- 12 pills - $40.95
- 24 pills - $64.95
- 36 pills - $78.95
- 60 pills - $111.95
- 120 pills - $155.95
They are often associated with hypotony and may develop in the early postoperative period after ophthalmic surgery treatment resistant depression safe secnidazole 1gr. Hemorrhagic detachments are often dome shaped, involve multiple quadrants, and may be associated with breakthrough vitreous bleeding. Choroidal osteomas are benign, presumably acquired bony tumors that typically arise from the juxtapapillary choroid in young adults (more commonly in women) and are bilateral in 20%25% of cases. Ultrasonography reveals a high-amplitude echo corresponding to the bony plate and loss of the normal orbital echoes behind the lesion (acoustic shadowing). Choroidal osteomas typically enlarge slowly over many years and can decalcify with time. The etiology of these lesions is unknown, but chronic low-grade choroidal inflammation has been suspected (see Chapter 12). Choroidal hemangiomas (see Chapter 18) resemble the surrounding fundus in color and may appear to be lightly pigmented. These lesions, which are often associated with overlying cystic retinal degeneration, are hyperechogenic on ultrasonography and show a characteristic vascular pattern on fluorescein and indocyanine green angiography. The clinician can easily diagnose this condition by observing its coincidence with the vortex vein ampulla and by gently compressing the eye during indirect ophthalmoscopy, which causes the varix to deflate. Table 17-1 lists additional conditions to be considered in cases with amelanotic choroidal masses. Classification Melanomas of the ciliary body and choroid have been categorized by size in several different ways. Although a size classification based on tumor volume would be logical, no simple and reliable method for assessing tumor volume is available. Metastatic Evaluation the incidence of metastatic uveal melanoma is as high as 50% at 25 years after treatment for ciliary body or choroidal melanoma. However, metastatic disease at the time of initial presentation can be detected in less than 2% of patients. It is likely that many patients have undetectable micrometastases at the time of their primary treatment. The liver is the primary organ involved in metastatic uveal melanoma; in 90% of patients, liver involvement is the first manifestation of metastatic disease. Other relatively frequent sites, generally after liver metastasis, include the lungs, bones, and skin. In cases that were autopsied, liver involvement was found in 100% and lung involvement in 50% of patients with metastases. All patients require metastatic evaluation prior to definitive treatment of intraocular melanoma (Table 17-3). To determine whether the patient has any other medical conditions that contraindicate surgical treatment or need to be treated. If there is any question regarding whether the lesion in the eye is a metastatic tumor, the clinician should conduct a thorough medical evaluation to determine the site of primary malignancy. If metastatic disease is clinically present during the pretreatment evaluation, enucleation may be inappropriate. In order to detect metastatic disease at an early phase, metastatic evaluation is often performed on a serial basis for all patients with uveal melanoma. Metastatic evaluation should include a comprehensive physical examination and imaging of the lungs and liver. Liver function tests are usually performed; however, they have recently become less reliable in the evaluation of liver metastases because of increasingly common fatty liver disease and the widespread use of cholesterol-lowering statins, which may alter liver enzyme levels. Lung imaging is also usually performed at the time of diagnosis, although its yield is low. Possible novel blood markers for early detection of metastatic uveal melanoma are being explored. Biopsy is appropriate before the institution of any treatment for metastatic disease. The interval between the diagnosis of primary uveal melanoma and its metastasis depends on many clinical, histologic, cytogenetic, and molecular genetic factors. Surveillance options for patients with uveal melanoma following definitive management. Treatment For many years, management of posterior uveal melanomas was controversial for 2 reasons: (1) data on the natural history of untreated patients with posterior uveal melanoma were limited, and (2) there were insufficient data on patients who were matched for known and unknown risk factors and managed by different therapeutic techniques to assess the comparative effectiveness of those treatments. Currently, both surgical and radiotherapeutic techniques are used to treat posterior uveal melanoma. Significant controversy persists regarding the diagnosis and management of small choroidal melanomas. Lesions with any of the 5 main risk factors for growth (thickness >2 mm, subretinal fluid, symptoms, orange pigment, or tumor margin touching the optic nerve head), and all lesions with documented growth, should be considered for treatment. Short-term observation to verify growth of a suspected small uveal melanoma has traditionally been considered appropriate, especially when the tumor is located in the macular area. As mentioned earlier, a fine-needle aspiration or vitrectomy biopsy can be considered as an alternative. Observation of active and larger melanomas may be appropriate in very elderly patients and those with systemic illness who are poor candidates for any kind of therapeutic intervention. Enucleation Historically, enucleation has been the gold standard in the treatment for malignant intraocular tumors. A past hypothesis that surgical manipulation of eyes containing a melanoma would lead to tumor dissemination and increased mortality is no longer accepted.
© 2025 Adrive Pharma, All Rights Reserved..