General Information about Roxithromycin
Roxithromycin is an antibiotic generally used for treating varied infections attributable to bacteria. It belongs to the macrolide household of antibiotics and is a semi-synthetic derivative of the pure macrolide antibiotic erythromycin.
Aside from respiratory and STD infections, roxithromycin can additionally be used to deal with dental and gum infections corresponding to gingivitis and periodontitis. It can successfully kill the micro organism liable for these infections, decreasing inflammation and selling healing of the affected gums.
In conclusion, roxithromycin is a flexible antibiotic that is effective in treating a wide range of bacterial infections. Its capability to target several varieties of bacteria makes it a go-to choice for a lot of healthcare suppliers. However, like all drugs, it should be taken with warning and under medical supervision to ensure its optimum efficacy and prevent the event of resistance.
Roxithromycin is usually nicely tolerated, with minimal side effects. The most common ones reported include nausea, vomiting, and diarrhea. Some people may expertise allergic reactions similar to pores and skin rash, itching, and problem respiration.
One of the most common uses of roxithromycin is for the therapy of respiratory tract infections similar to bronchitis, pneumonia, and sinusitis. It is also efficient in treating upper respiratory tract infections like tonsillitis and pharyngitis. In addition, it can be used to deal with lower respiratory tract infections like persistent bronchitis and COPD exacerbations.
Roxithromycin has additionally been discovered to be helpful in treating some sexually transmitted diseases (STDs) attributable to chlamydia and mycobacterium avium complicated (MAC). It works by inhibiting the growth of micro organism, due to this fact stopping the infection from spreading and permitting the physique's natural immune system to fight off the remaining bacteria.
Furthermore, roxithromycin has been used in the treatment of bronchial asthma, significantly in instances where other antibiotics have failed. Some studies have proven that it could help in lowering irritation in the airways, leading to improved signs and lung function in asthmatic sufferers.
Another space the place roxithromycin has proven promise is in treating abdomen and intestinal infections. It has been discovered to be efficient in opposition to Helicobacter pylori, a type of micro organism generally associated with abdomen ulcers and gastritis. In combination with other medications, roxithromycin can be used to eradicate these bacteria and forestall the recurrence of abdomen and intestinal ulcers.
As with any treatment, it is essential to comply with the dosage and length prescribed by a healthcare skilled. Overuse or misuse can lead to the event of antibiotic resistance, making it tougher to treat infections in the future. It is also crucial to complete the total course of therapy even when signs improve, as stopping too soon can lead to a relapse of the an infection.
Once safe initial entry is conftrmed antibiotic with a c cheap 150 mg roxithromycin fast delivery, the area directly below the primary trocar entry site is evaluated for bleeding or other signs of entry trauma. Specifically, the liver surface, gallbladder, falciform ligament, stomach, omenrum, and right and left hemidiaphragms arc inspected. After T renddenburg positioning, bowel and omentum fall toward the upper abdomen to expose the retroperitoneal structures. Now free of intestines, the area directly beneath the initial entry site is examined again. Previously unappreciated trauma to this area from initial abdominal entry cnight then be seen. Most laparoscopic surgery is performed in an operating room with general aneschesia. Peritoneal pain created by the intraabdominal pneumoperitoneum merits this degree of anesthesia. Following anesthesia induction, the patient is placed in low lithotomy position to permit access to the cecvix and allow uterine manipulation. Even for anticipated short procedures, correct patient positioning is critical to help avoid patient nerve injury and to optimize surgeon ergonomics and access. A bimanual examination is completed to determine uterine inclination, which will direct uterine manipulator positioning, if used. For longer procedures, a Foley catheter may be required as a full bladder can obstruct the operating view or increase the risk of bladder injury. These include Veress needle insertion, direct trocar insertion, optical-access insertion, or open entry methods. A 5-mm or 10-mm umbilical port will house a suitable laparoscope for diagnostic examination. Generally, starting with a 5-mm incision and 5-mm laparoscope allows adequate viewing of the abdocninopelvic cavity. Once safe initial entry is confirmed, the abdomen is insuffiated to reach an intraabdominal pressure of 15 mm Hg or less. First, the uterus is retroflexed with the aid of the uterine manipulator to provide clear viewing of the anterior cul-de-sac. Next, the manipulator tilts the uterus up and to the right to permit left pelvic sidewall inspection. During this, endometriotic implants, peritoneal defects or windows, studding concerning for malignancy, adhesions, and fibrosis are sought. Of pelvic organs, both ureters are found coursing from the pelvic brim, along the lower pelvic sidewall, and to the cervix. To examine both fallopian tubes and ovaries, a surgeon places a blunt probe into the cul-desac and sweeps the probe forward and laterally. In doing so, the tubes and ovaries are lifted from the posterior cul-de-sac or ovarian fossa for inspection. However, bilateral lower quadrant locations may be desired if lysis of adhesions or greater tissue manipulation is required. Additional ports arc placed under direct laparoscopic guidance, as described in Chapter 41 (p. To prevent 1018 Atlas of Gynecologic Surgery diaphragmatic irritation from retained C02, manual pressure against the abdominal wall hc:lps expc:l remaining gas. During this process, all secondary cannulas are removed using laparoscopic visualli. This allows exclusion of bleeding from puncrured vessels that may have been tamponaded by these cannulas. Additionally, it prevents herniation of bowel or omentum up through the cannula track and into the anterior abdominal wall. Accordingly, potential bleeding sites are reinspected as the pneumoperitoneum is rdeased. Next, the primary cannula is removed while leaving the laparoscope in the abdomen. Last, the laparoscope is slowly removed to visualize the abdomen and primary entry site for any evidence of bleeding and to prevent viscera from being pulled into the port site. Skin incisions arc closed with a subcuticular stitch of 4-0 gauge dc:layed-absorbable suture. To prevent incisional hernia fonnation, fascial closure often is recommended whenever trocars measuring ~ 10 mm are employed (Lajer, 1997; Lambenz, 2017; Wc:lls, 2019). If open entry was used, the sutures originally placed in the fascia are unthreaded from the Hasson cannula. Each of these sutures is brought to the midline of the incision, and square knots are tied to close the fascial defect. Minimally Invasive Surgery lncrcaaingly, these dcvica are being removed in symptomatic paticna. If implants arc not ffCll sonographically, plain abdominal radiograph1 aui help identify devices that may have perfo. Moat interval procedures arc performed la~ aroacopically, and common optiona achieve tubal occlU41on by decaosurgkal c. Currcndy thcomical, suggcm:d adwntagcs arc fully daaibc:d io Chapters 5 and 35 (pp. If advanced bipolar coagulation device& are employed, surgical speed and ease arc balanced againat cost. Blood loss aod tolDpikadon rates arc comparable bctwecn the two (Kim, 2019-a; Powell, 2017; Wutbc:rg.
Women who have previously had a hysterectomy arc not usU:&lly good candidates beethoven virus roxithromycin 150 mg order fast delivery, because a complete resec-tion of a central recurrence involving the vaginal cuff would typic:ally require removal of both bladder and rcctosigmoid colon. The appropriate skin Incision ls made, the ahdomcn is a:plored, lymph noda are removed, and spaces are developed to ex. A swgcon then makes the final decision to leave the rec:twn intact and proa:cd with anterior pelvic aentc. Typic:ally, the lesion is small and lies above the levator ani muscle&, thus a perineal phase is not required. For this reason, placement of a myocutaneom flap fur vaginal n:construc:tion may be more problematic In these patients due to limited spaa: in the pelvis. Ideally, the operation i5 shorter and rest:Qration of bowd function ls more rapid. Surgeries for Gynecologic Malignancies 1181 Posterior Pelvic Exenteration Removal of the uterus, vagina, recwm, and par. The most common indication is a small postirradiatlon recurrence primarily involving the posterior wgina1 wall or coexisting with a rcctovagia. Pom:rior pelvic: aentera· tion is tr:chnically similar to a type Ill radial hystcn:aDmy but with the addition of rectosigmoid rcsec:tion and a more extended ·ec:tomy (Section 46-1, p. The appropriate skin inci· sion is made, the ahclomen is aplored, lymph 0 Uretenil Dissection. The sigmoid colon is divided with the mesentery and peritoneal attachments, as earlier described. As a result, placement of a myoc:utaneous flap for vaginal reconstruction may be more problematic: in such patients due to limited space i. However, posterior exenteration in a previously irradiated patient &equently raults In a contracted bladder and inttactahlc: urinary incontinence. The en~ specimen may then be placed on traction to 1182 Atlas of Gynecologic Surgery help avoid tension that might lead to anastomotic leaks. Last, creation of a straight tunnel through the abdominal wall helps prevent bowel kinking and obstruction. Less commonly, an otherwise irreparable postirradiation vesicovaginal fistula may warrant urinary diversion. Following cystectomy, an isolated resecced segment of bowel that maintains its mesenteric connection and vascular supply is used as the new urine reservoir. A stoma is crafted using one end of the bowel segment and an opening in the anterior abdominal wall. Various techniques are available co create such urinary conduits, and these are categorized as incontinmt divmions or continmt diversions. An incontinent diversion is the simplest to create, but postoperatively a patient must continuously wear an ostomy hag. These conduits arc often preferable for medically compromised patients, the elderly, and anyone with a shon life expectancy. Alternatively, a continent urinary reservoir can be created that is emptied by intermittent patient sdfcathcceri7. Of incontinent diversions, an ikal conduit has historically been the most common urinary diversion used in gynecologic oncology (Goldberg, 2006). However, this bowel segment and distal ureters invariably lie within a previously irradiated field. Conduit construction with radiation-damaged bowel may lead to higher rates of sccnosis or leakage at the ureteral anastomotic sites (Pycha, 2008). The transverse colon conduit is a successful alternative for previously irradiated patients (Segreti, 1996; Soper, 1989). Sigmoid conduits are generally less desirable due to preexisting radiation damage and proximity to a concurrent colostomy site. Electrolyte abnormalities such as chronic metabolic acidosis and hypokalemia are an associated risk. The basic principles of constructing an incontinent urinary conduit are the same, regardless of the intestinal segment used. Second, widecaliber uretcrointestinal anastomoses and ureteral scenting are essential to minimize the risk of anastomosis stenosis. The specific decision is whether to plan for an incontinent or continent urinary conduit. The type of conduit selected should be considered permanent, although later conversions are possible (Benezra, 2004). The final decision is then made regarding which type of incontinent conduit is best for the circumstances. If the distal ileum has the typical leathery, pale, mottled appearance of radiation injury, a conduit should be prepared from the transverse colon. Overlooking the imponance of this decision can lead to various otherwise preventable complications intraoperatively and postoperatively. The ileocecal junction is located, and the ileum is elevated co identify a bowel segment with the most mobility to reach the stoma site on the right side of the anterior abdominal wall. Ideally, the proximal end of the segment lies 25 to 30 cm from the ileocecal valve, which is a watershed area and necessary for absorption of bile salts and fu. Watershed ~ns in general receive dual blood supply from the very distal branches of two arteries and thereby are vulnerable to ischemia. At the sdected site, the mescntery is scored on each side with an electrosurgical blade to aid insertion of a hemostat directly beneath the bowd loop. This will mark the proximal end along the ileum that will eventually become the distal part of the conduit and will form the abdominal wall stoma.
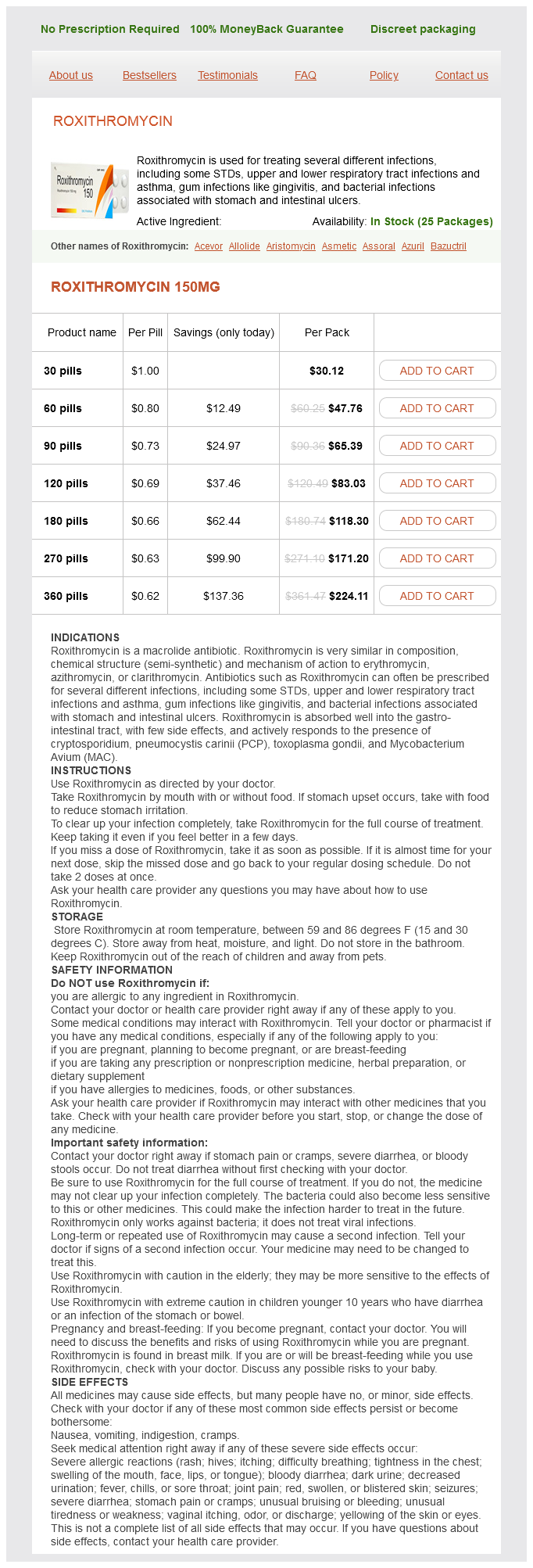
Roxithromycin Dosage and Price
Roxithromycin 150mg
- 30 pills - $30.12
- 60 pills - $47.76
- 90 pills - $65.39
- 120 pills - $83.03
- 180 pills - $118.30
- 270 pills - $171.20
- 360 pills - $224.11
The latter includes activation of vasoconstrictor lipoxygenase products virus 68 ny roxithromycin 150 mg purchase without a prescription, oxidative stress, and endothelin. The complexity of these relationships partly explains the failure of measuring any single clinical pathway to predict blood pressure responses to renal revascularization. Accelerated Hypertension and Pulmonary Edema Series of patients referred for renal revascularization in recent decades have included older patients with more widespread atherosclerotic disease than ever before. Patient demographics commonly include more women than men and a high prevalence of coronary disease, congestive cardiac failure, and known cerebrovascular disease. In some cases, suspicion arises regarding renal artery stenosis because of rapid acceleration of these processes, particularly the rapid increase in arterial pressure in a previously stable patient. In other cases, presenting symptoms include recent progression of hypertension followed by neurologic symptoms of an acute stroke. Some patients develop cycles of worsening congestive cardiac failure out of proportion to left ventricular dysfunction. When volume expanded, renal function may improve slightly at the price of hypertension and circulatory congestion. Sudden pulmonary edema partly reflects diastolic dysfunction precipitated by a rapid increase in afterload in addition to impaired sodium excretion as a result of renal hypoperfusion. During volume depletion, serum creatinine commonly rises with evidence of "prerenal" azotemia. This condition warrants recognition because several series indicate that cycles of symptomatic exacerbation, hospitalization, and mortality can be improved with successful renal revascularization. This shift in clinical practice means that many poststenotic kidneys are exposed to perfusion pressures less than the level of autoregulation during antihypertensive drug therapy. A corollary observation is an increased likelihood of those kidneys developing irreversible parenchymal injury. The precise mechanisms responsible for irreversible renal scarring in "ischemic" nephropathy have not been fully elucidated. Both intermittent local ischemia (shown on the left) and vasoconstrictormediated cytokine-mediated pathways (right) participate in this process. It also contributes to renal fibrosis by recruiting bone marrowderived fibrocytes, circulating cells that contribute to the pathogenesis of fibrotic diseases. Endothelins the endothelin peptides comprise a family of peptides produced and released from endothelial cells, which have potent and long-lasting vasoconstrictor effects on the renal microcirculation and modify tubular function. Tissue levels of endothelin-1 are increased in the stenotic kidney,21 and in fact in most forms of renal failure, and may persist for days after resolution of the initial injury. Chronic blockade of the endothelin Areceptor directly inhibits cellular growth and gene expression and, in ischemic acute renal failure, provides long-term functional and morphological benefits in experimental models. Renal blood flow, glomerular filtration rate, and redox status significantly improve in the swine stenotic kidney after endothelin A-receptor but not endothelin B-receptor blockade, implying that the former ameliorate renal injury in pigs with advanced renovascular disease. Conversely, thromboxane A2 is an endothelium-derived vasoconstrictor prostaglandin that is upregulated in kidneys with renovascular disease. Blockade of thromboxane A2 receptors thus improves urine volume, glomerular filtration rate, and renal plasma flow in ischemic kidneys and exerts a variety of beneficial effects that reduce the severity of ischemic damage. Oxidative Stress and Fibrosis A growing body of evidence implicates increased generation of reactive radical species as a mechanism for renal injury in renovascular disease. Increased oxidative stress can promote the formation of a variety of vasoactive mediators including endothelin-1, leukotrienes, and prostaglandin F2 isoprostanes, endogenous products of lipid peroxidation. Functionally, reactive oxygen species have been implicated in decreasing stenotic kidney blood flow and sustaining renovascular hypertension. In addition, reactive oxygen species are implicated in the pathogenesis of ischemic renal injury by causing lipid peroxidation of cell and organelle membranes and disrupting the structural integrity and capacity for cell transport and energy production, especially in the proximal tubule. Studies in humans confirm that oxidative stress contributes to the impairment in endothelium-dependent vasodilatation observed in patients with renovascular hypertension, which can be reversed with successful renal revascularization. It interacts with endothelin and several growth factors and cytokines in promoting progressive interstitial fibrosis primarily via its downstream effectors from the Smad family. Rapid restoration of blood flow to a poststenotic kidney can trigger "ischemiareperfusion injury," characterized by apoptosis, oxidative stress, inflammation, and calcium overload. This in turn favors formation of the mitochondrial permeability transition pore, a high conductance channel formed in the inner mitochondrial membrane. Opening of this pore facilitates release of cytochrome c and mitochondrial reactive oxygen species to the cytoplasm, initiating apoptosis and contributing to cellular oxidative stress. Inflammation Accumulating evidence indicates that inflammatory pathways are an important mediator of deleterious processes in the stenotic kidney. The poststenotic human kidney releases multiple markers reflecting active inflammation that translate to kidney injury and reduced function. Susceptible proximal tubule cells are primarily responsible for the pathophysiologic and clinical aspects of ischemic acute renal failure. Of central importance is disruption and dissociation of the actin cytoskeleton and associated surface membrane structures that occur rapidly and depend upon the severity and duration of ischemic injury. These alterations may be secondary to activation and relocation of the actin-associated protein actin depolymerizing factor/cofilin and 1 integrin to the apical membrane. The epithelial brush border may disappear, in association with apical membrane blebbing, interruption of cell-tocell junctions, and subsequently epithelial desquamation. Detachment of tubule cells and microvilli contributes to backleak of glomerular filtrate and formation of intraluminal aggregations of exfoliated cells, proteins, and glycoproteins like fibronectin, resulting in tubular obstruction. The functional ramifications of these changes are substantial in terms of tubular reabsorption, function of the intercellular tight junction, impaired cell-substrate adhesion, and integral membrane protein function. Tubulointerstitial Injury the severity of pathological tissue damage in the kidney beyond an atherosclerotic renal artery stenosis is an important determinant and predictor of renal functional outcome.
© 2025 Adrive Pharma, All Rights Reserved..