General Information about Rosuvastatin
In conclusion, rosuvastatin is a broadly prescribed treatment for reducing ldl cholesterol and triglycerides within the body. It has been confirmed to be efficient in lowering the chance of heart disease and different cardiovascular complications. However, it is essential to use it as prescribed and to observe a wholesome lifestyle, together with a balanced diet and regular exercise, for optimal outcomes. If used correctly, rosuvastatin can be an important software in sustaining wholesome cholesterol levels and stopping severe well being issues.
Rosuvastatin is available in pill kind and is usually taken as quickly as a day, with or with out meals. The dosage will differ relying on the individual and their medical condition. It is important to comply with the prescribed dosage and not to cease taking the treatment with out consulting a doctor, as this could result in a sudden increase in levels of cholesterol. Regular blood tests can also be required to watch cholesterol levels and verify for any potential unwanted side effects.
High ldl cholesterol, or hypercholesterolemia, is a common drawback that impacts hundreds of thousands of people worldwide. Cholesterol is a fatty substance discovered within the blood and is important for various bodily functions. However, when the levels of ldl cholesterol in the blood are too high, it may possibly lead to the formation of plaque in the arteries, which might narrow or block the move of blood and enhance the danger of heart illness. Triglycerides, on the opposite hand, are a sort of fats found within the blood and excessive ranges of it have additionally been linked to an elevated danger of heart illness.
Rosuvastatin works by slowing down the manufacturing of cholesterol within the liver, thus decreasing the amount of it within the blood. It also will increase the liver's capability to remove ldl cholesterol from the blood. As a outcome, the degrees of LDL (bad) cholesterol and triglycerides are lowered, while the degrees of HDL (good) ldl cholesterol are increased. This helps in stopping the buildup of plaque within the arteries and reduces the danger of heart illness.
Rosuvastatin, also identified by its brand name Crestor, is a popular medicine used for reducing high ranges of cholesterol and triglycerides in the body. It belongs to a bunch of medicine known as statins, which work by blocking the enzyme responsible for producing cholesterol within the liver. Rosuvastatin has proved to be extremely effective in lowering the risk of coronary heart disease, stroke and different cardiovascular issues.
Rosuvastatin may not be appropriate for everyone, and you will need to seek the guidance of a well being care provider earlier than starting the treatment. People with liver or kidney disease, diabetes, thyroid issues, or a history of alcohol abuse should use warning when taking rosuvastatin. It can also interact with sure medicines, so it's essential to inform a physician about all current medications, including over-the-counter medication, herbal dietary supplements, and nutritional vitamins.
Like any treatment, rosuvastatin could cause some side effects, though not everybody experiences them. Common unwanted side effects embrace headache, muscle pain, weak spot, nausea and stomach pain. In uncommon instances, it might also trigger extra severe unwanted effects corresponding to liver issues and muscle breakdown. It is important to inform a doctor if any unwanted effects are skilled, as they might want to adjust the dosage or change to a special medicine.
For a variety of reasons cholesterol oxidation eggs discount rosuvastatin online american express, patients often fail to provide accurate surgical histories. The physical examination is an excellent opportunity to review the abdominal and pelvic surgical history. The pelvic examination should assess for fluid in the vaginal canal, which can be collected and sent for creatinine levels [29]. The patient can also be asked to provide tampons or pads for creatinine evaluation. A urine specimen should be sent for urinalysis and culture to allow treatment of urinary tract infections prior to surgical repair. Special attention should be given to the vaginal cuff, anterior vaginal wall, and the cervical os. Irradiated patients may have friable lesions that present months and even years after their treatment. These lesions should be documented and subsequently biopsied to rule out the recurrence of malignancy [35,75]. However, smaller fistulas can be difficult to identify on physical exam and often require further investigation with examination under anesthesia, endoscopic evaluation, and imaging. If vaginal atrophy is present on exam, it should be treated preoperatively with topical vaginal estrogen to improve the quality of the vaginal epithelium to aid in surgical repair. A narrow introitus may warrant relaxing incisions at the time of repair to provide adequate access to the fistula [6]. Although the dye test is considered a routine diagnostic test for urogenital fistula, there are no large series to our knowledge that report the sensitivity or specificity of this test. The dye test is performed by filling the bladder with dilute methylene blue [77] or indigo carmine [39] solution (up to 300 mL). If the fistula is not seen, a tampon can be placed into the vagina, and the patient is asked to ambulate, and the vaginal packing is evaluated. If blue staining is noted, the pattern of staining can provide useful information about the possible location of the fistula. The blue dye test has been used in the literature to diagnose vesicouterine fistulas. Once the urine is noted to be orange, the bladder is emptied and filled with 300 mL of blue dye diluted in normal saline solution. A tampon or vaginal packing is placed and after ambulation, the packing is evaluated. Blue staining is suggestive of a concomitant vesicovaginal and/or urethrovaginal fistula. Endoscopic Evaluation Cystoscopy is a valuable diagnostic tool and should be performed in any patient presenting with suspected urogenital fistulas. Cystoscopy has been shown to be a sensitive test identifying 92%93% of genitourinary fistulas in two small series [42,76]. A guidewire or a 5 French open-ended ureteral catheter can be passed through the working port of the cystoscope and used to probe any suspicious appearing erythematous patches, areas of bullous edema, or granulation tissue. Cannulation of the fistulous tract can help the clinician determine the course of the urogenital fistulas. Fistula involvement of the bladder neck, external sphincter, and bladder trigone should be documented. Proximity to these vital structures may warrant concomitant bladder neck reconstruction, autologous pubovaginal sling, or ureteral reimplant, respectively. Cystoscopy under anesthesia should be performed when obstruction is present on ultrasound and upper tract involvement is suspected [23]. This allows the clinician to perform retrograde urography and place a ureteral stent in the same setting, if needed (see in the following text). If vaginal inspection does not demonstrate an obvious connection, placement of a guidewire through the cystoscope port through the fistula can identify the tract. Patients with a history of gynecological malignancy or pelvic irradiation should have biopsies of the fistula tract taken prior to repair to rule out recurrences and secondary malignancies [35]. If mesh is noted during endoscopic evaluation, operative notes should be reviewed to provide further information regarding the size and course of the mesh. The simultaneous use of vaginoscopy and cystoscopy has been described in the literature as a method for identifying difficult fistulous tracts [80]. We find this practice using a flexible cystoscopy extremely useful for a complete preoperative assessment of the fistula. In cases of small fistula tracts, dye can be used to fill the bladder (ureter or uterus) while simultaneously performing vaginoscopy to look for dye-stained egress of fluid. Imaging Imaging can be used to determine the number and location of the fistulous tracts. Imaging is also helpful when the clinician needs to confirm the diagnosis when it is in doubt. Voiding phase images can be added to evaluate for concomitant urethrovaginal fistulas. Ureterovaginal fistulas can be present in up to 12% of patients presenting with vesicovaginal fistulas. Partial ureteral obstruction in a patient with a suspected fistula is suggestive of an ureterovaginal fistula until proven otherwise [77]. If ureteral stents cannot be passed beyond the site of obstruction, a percutaneous nephrostomy tube should be placed to maximally drain the urinary system prior to operative repair.
As the aim of chemoprophylaxis is the prevention rather than the treatment of established infection cholesterol test results calculator rosuvastatin 10 mg order overnight delivery, regimens used should aim to achieve a high tissue concentration of the chosen antibiotics at the time of surgery when inoculation of the wound occurs. However, as this would mean the administration of intravenous antibiotics some hours prior to surgery, a more practical compromise is to give the first dose at the time of induction of anesthesia, with a further two doses in the first 24 hours postoperatively. In addition, prior to mesh augmentation surgery such as sacrocolpopexy, it is our practice to presoak the mesh in gentamicin solution prior to its use. If a patient does develop an infection, however, different antibiotics have to be used, such as vancomycin, which may not be as effective, has more side effects, and is more expensive than conventional therapy. Chlorhexidine gluconate 4% (Hibiscrub or Hydrex) for body and hand washing daily for 5 days. Alternatively, triclosan 2% (Aquasept) may be used in the event of a patient allergy. Mupirocin 2% nasal ointment (Bactroban Nasal) applied to the inside of the nostrils, using a gloved finger, three times daily for 5 days. Press the nostrils together for a few seconds to thoroughly spread the ointment over the insides of both nostrils. The hands must be decontaminated prior to donning gloves and disposable plastic apron. After contact with patients or patient environment, the gloves and apron must be removed while in the room and disposed of in the clinical waste bin, and the hands must be decontaminated before leaving the room or immediately upon exit. In high-risk cases, the hourly urine output is a sensitive measure of peripheral circulation. Analgesia 1073 Postoperative respiratory complications associated with wound pain may delay recovery [39]. Effective postoperative analgesia can facilitate recovery and reduce morbidity in surgical patients by blunting autonomic, somatic, and endocrine reflexes [40]. Postoperative pain is mediated via nociceptive, inflammatory, and neuropathic mechanisms and varies between individuals and different operative procedures. Multimodal postoperative analgesia addresses both different pain modalities and types of surgery [41]. Multimodal analgesia may also be opioid sparing and reduce opioid-related side effects, thereby facilitating patient recovery and ambulation [42]. Most hospitals usually have a local protocol for postoperative analgesia, which is initiated by the anesthetist. Vaginal Pack and Indwelling Catheter Care Indwelling urinary catheter and vaginal pack has been the standard practice after pelvic floor dysfunction surgery. The catheter is used to allow bladder emptying when natural voiding is difficult or impossible due to the presence of vaginal pack, pain, or soft tissue swelling. The duration of catheterization and vaginal packing has been reduced over the years, but there is no consensus on how to minimize complications, and practice varies. A trend toward increased hematoma and significant complications was seen in the no-pack group. As vaginal packing does no harm and may be of some benefit, it may be argued that packing should be recommended as routine clinical practice [44]. In a Cochrane study on short-term urinary policies following urogenital surgery in adults, no randomized studies were found comparing the use of urinary catheter versus no urinary catheter in patients following prolapse operations. Whether or not to use a particular policy concerning when to remove the urinary catheter and vaginal pack is usually a trade-off between the risks of morbidity (especially infection) and risks of recatheterization. In our practice, both the vaginal pack and indwelling catheter are usually removed in the morning, on the first day after surgery. Anticipation of Postoperative Voiding Problems Voiding difficulties may occur acutely following any pelvic surgery and after continence procedures in particular. Acute over distension of the bladder leads to damage of the detrusor syncytium with ischemic damage to the postsynaptic parasympathetic fibers. This may result in insidious deterioration of detrusor function and the onset of voiding dysfunction [46]. In suspected cases of acute urinary retention, an indwelling urethral catheter should be inserted immediately, although some authors prefer intermittent catheterization [48]. In women judged to be at high risk of retention, suprapubic catheterization may be a preferable option. This can be performed easily at the time of surgery and avoids the need for repeated urethral catheterization. Following removal of a catheter, close monitoring of fluid balance should be continued to prevent recurrent retention. As voiding difficulties are more common following continence procedures, it is important that women are counseled adequately. Even though perhaps only a minority of these women will need to self-catheterize, from the 1074 psychological standpoint, short-term voiding problems are much better dealt with when they have been anticipated. In other cases, sending patients home with a catheter (urethral or suprapubic) on free drainage for a week or two, followed then by a trial without catheter, is usually a successful strategy. Hemorrhage Intraoperative Hemorrhage Significant hemorrhage is very rare following urogynecological surgery. In the event of massive hemorrhage, it is important to monitor the coagulation status of the patient repeatedly during resuscitation to diagnose the onset of a consumptive coagulopathy. In cases of massive intraoperative bleeding complicated by coagulopathy, it may be very difficult to achieve hemostasis. In such situations, the use of pelvic packs for 48 hours may be the only option, although this necessitates a second laparotomy to remove the packs. Occasionally, embolization of actively bleeding blood vessels using interventional radiology techniques may be an effective alternative to surgery.
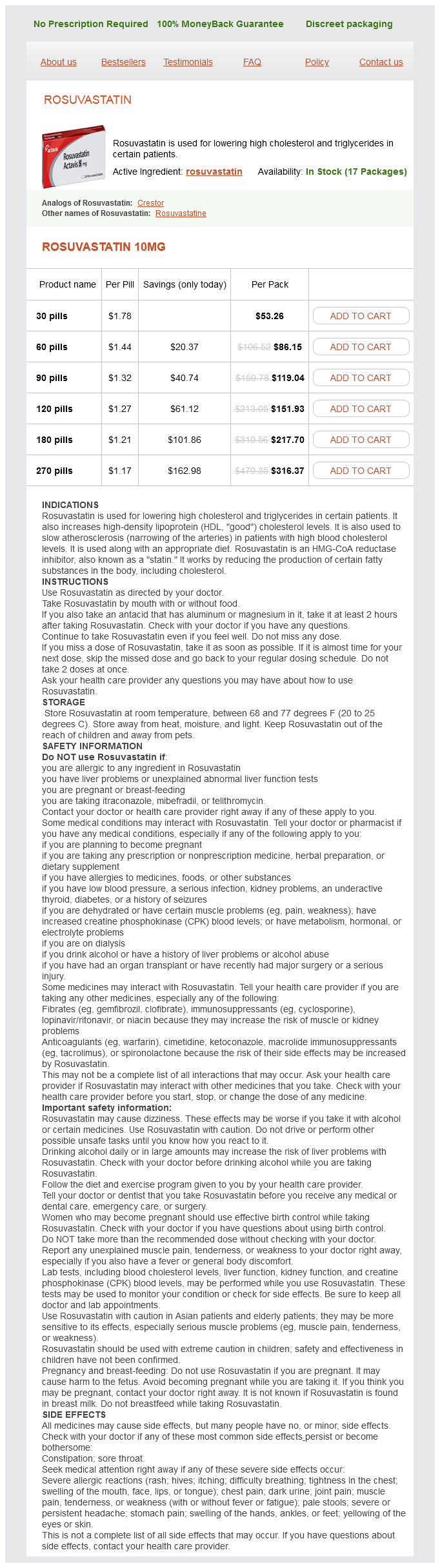
Rosuvastatin Dosage and Price
Rosuvastatin 10mg
- 30 pills - $53.26
- 60 pills - $86.15
- 90 pills - $119.04
- 120 pills - $151.93
- 180 pills - $217.70
- 270 pills - $316.37
Colporectocystourethrography (colpocystodefecography) [43]: this involves the instillation of radiopaque media into the bladder subway cholesterol chart cheap 10 mg rosuvastatin with mastercard, vagina, and rectum simultaneously for pelvic floor evaluation with images obtained during rest and straining. It is noninvasive, has excellent soft tissue contrast resolution without exposure to ionizing radiation, and allows the study of function of pelvic floor structures under different dynamic conditions such as increased Pabd during Valsalva [45,46]. Currently, the clinical value of these examinations is still under investigation with its impact on therapeutic decisions not yet fully evaluated. Bladder neck and cervical descent/mobility Position of bladder neck and cervix at rest and on Valsalva. Bladder neck or cervical descent >2 cm below this line with straining indicates weakness of the pelvic floor. If alternative landmarks are used in scientific papers, they should be clearly described. Pelvic floor measurements/levator defects: Assessment of the configuration of pelvic floor muscles, in particular, the levator ani. A: Urodynamic Stress Incontinence Definition: As noted in Section 3E(2d), this diagnosis by symptom, sign, and urodynamic investigations involves the finding of involuntary leakage during filling cystometry, associated with increased intra- 1802 abdominal pressure, in the absence of a detrusor contraction. Bladder Oversensitivity Definition: Bladder oversensitivity, a diagnosis made by symptoms and urodynamic investigations, is more likely to occur in women with symptoms of frequency and nocturia and a voiding diary showing a clearly reduced average voided volume. Also referred to as "increased bladder sensation" [3], bladder oversensitivity replaces the now obsolete term of "sensory urgency" [50,51]. As noted in Section 3D(3f), it can be defined as an increased perceived bladder sensation during bladder filling 1C(1) with specific cystometric findings of (1) an early first desire to void 3D(3b); (2) an early strong desire to void, which occurs at low bladder volume 3D(3d); (3) a low maximum cystometric bladder capacity 3D(4b); and (4) no abnormal increases in Pdet [50,51]. Specific bladder volumes at which these findings occur will vary in different populations. Definition: Voiding dysfunction, a diagnosis by symptoms and urodynamic investigations, is defined as abnormally slow and/or incomplete micturition [53]. Abnormal slow urine flow rates and abnormally high postvoid residuals, the basis of this diagnosis, are outlined in Sections 3A(10) and 3B(3). Further evaluation-pressureflow studies (voiding cystometry): Pressureflow studies are indicated to evaluate the cause of any voiding dysfunction. Some possible causes have been already defined: 3F(3b) detrusor underactivity, 3F(3c) acontractile detrusor, and 3G(2) bladder outflow obstruction. Acute retention of urine [3]: this is defined as a generally (but not always) painful, palpable, or percussible bladder, when the patient is unable to pass any urine when the bladder is full. The standardisation of terminology of lower urinary tract function: Report from the standardisation subcommittee of the International Continence Society. The standardization of terminology for researchers in female pelvic floor disorders. Definition and classification of urinary incontinence: Recommendations of the Urodynamic Society. Sexual function in women with/without urinary incontinence and or pelvic organ prolapse. Correlation of symptomatology with degree of pelvic organ support in a general population of women: What is pelvic organ prolapse Standardization of terminology of pelvic floor muscle function and dysfunction: Report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. The standardisation of terminology of nocturia: Report from the Standardization Subcommittee of the International Continence Society. Maximum and average urine flow rates in normal male and female populations-The Liverpool nomograms. Immediate postvoid residuals in women with symptoms of pelvic floor dysfunction: Prevalences and associations. Standardization of urethral pressure measurement: Report from the Standardization sub-committee of the International Continence Society. The cough game: Are there characteristic urethrovesical movement 1804 patterns associated with stress incontinence. A standardised ultrasonic diagnosis and an accurate prevalence for the retroverted uterus in general gynaecology patients. Magnetic resonance imaging in evaluating functional disorders of female pelvic floor. Magnetic resonance imaging of uterine version in a multi-ethnic, nulliparous, healthy female population. Has the true incidence of voiding difficulty in urogynecology patients been underestimated Is sensory urgency part of the same spectrum of bladder dysfunction as detrusor overactivity The distribution of pelvic organ support in a population of female subjects seen for routine gynaecologic health care. Recurrent urinary tract infections in women with symptoms of pelvic floor dysfunction. Dynamic assessment of pelvic floor and bony pelvis morphologic condition with the use of magnetic resonance imaging in a multi-ethnic, nulliparous, and healthy female population. This is a common symptom, the mechanism of which has not been adequately researched. It is uncertain whether it should be linked to 1A(2) (stress urinary incontinence) or 1A(3) (urgency urinary incontinence). Traditionally, seven episodes of micturition during waking hours have been deemed as the upper limit of normal, though it may be higher in some populations [7]. It is common to void during the night when sleep is disturbed for other reasons-for example, insomnia and lactation- this does not constitute nocturia [8]. The use of the word "sudden," defined as "without warning or abrupt," used in earlier definitions [2,8] has been subject to much debate. Other symptoms of female sexual dysfunction including (1) decreased sexual desire, (2) decreased sexual arousal, (3) decreased orgasm, and (4) abstention are less specific for female pelvic floor dysfunction and will not be defined here.
© 2025 Adrive Pharma, All Rights Reserved..