General Information about Rogaine 5
One of the great things about Rogaine 5% is that it's easy to make use of and suits into any day by day routine. It is available in a topical answer that's applied directly to the scalp twice a day, ideally within the morning and at night. The solution is shortly absorbed into the scalp and leaves no residue, making it handy to use alongside different hair products. It can also be protected to make use of with different hair therapies, similar to shampoos and styling merchandise.
The 5% answer of minoxidil in Rogaine works by dilating the blood vessels in the scalp, which permits more oxygen, vitamins, and blood circulate to achieve the hair follicles. This, in flip, helps to stimulate hair progress and extend the expansion part of the hair cycle. It also helps to reverse the shrinking of hair follicles attributable to DHT, permitting them to produce thicker and healthier hair strands.
Male sample baldness, also referred to as androgenetic alopecia, is a hereditary condition brought on by the hormone dihydrotestosterone (DHT). DHT attaches to the hair follicles and causes them to shrink, leading to thinner and finer hair until finally, the hair follicles stop producing hair altogether. This usually occurs on the highest of the pinnacle and might lead to partial or full baldness.
Rogaine 5% is suitable for males aged 18 years and above and is mostly well-tolerated with minimal side effects. Some users might experience delicate scalp irritation or dryness, but these can be simply managed through the use of a moisturizing shampoo or adjusting the frequency of utility. However, should you experience severe irritation or any other concerning unwanted effects, it's best to consult with a physician.
While Rogaine 5% is efficient, it does require constant use to see outcomes. Most customers see visible enhancements in hair progress after 4 months of continuous use, and full results can be seen after 12 months. It is important to note that once you stop using Rogaine 5%, the hair progress might reverse, and you might experience hair loss again. Therefore, it is suggested to use it as a long-term treatment for continued results.
Male sample baldness is a common condition that affects tens of millions of males worldwide, and Rogaine 5% is among the leading treatments for this type of hair loss.
In addition to its use for male sample baldness, Rogaine 5% has also been discovered to be effective in treating hair loss because of different causes, similar to chemotherapy, stress, and hormonal modifications. It can be protected to make use of for individuals with delicate pores and skin or those who have undergone hair transplant surgery.
Rogaine 5%, also recognized as minoxidil, was first accredited by the FDA in 1988 for the treatment of male pattern baldness. Since then, it has turn into a staple in lots of males's haircare routines and has been clinically confirmed to assist regrow hair and slow down the development of hair loss.
Rogaine 5% has been a game-changer for many males fighting hair loss. While it might not work for everybody, it's a clinically confirmed remedy that has helped tens of millions of males regain their confidence and obtain a fuller head of hair. It is definitely accessible and available over the counter, making it a convenient choice for anyone eager to attempt it. As with any medication or treatment, it is all the time best to seek the advice of with a physician earlier than use to determine if Rogaine 5% is best for you.
Complications Major complications of this procedure include urethrovaginal fistula formation androgen hormone kinetics rogaine 5 60 ml purchase on line, development of stress urinary incontinence, recurrence of the diverticulum, missing diverticula when multiple diverticula are present, and stricture of the urethra. B, Fingers hold diverticulum on traction, which aids in dissection and identification of ostium. C, After complete resection of the diverticulum, the urethra is closed with fine, interrupted extramucosal sutures. After diverticulectomy, recurrence that requires repeat excision occurs about 10% of the time. Risk factors for recurrence included proximal diverticulum, multiple diverticula, and previous pelvic or vaginal surgery, excluding previous diverticulectomy. Some with recurrent diverticulum will have persistent pain or discomfort with urination and even with complete excision those symptoms can remain. Stress incontinence development may be related to the dissection of the bladder neck and proximal urethra with injury to the urethral sphincter mechanism. If intrinsic sphincter deficiency results, the incontinence can be difficult to treat because of tissue compromise from repair. One study compared risk factors and determinants of urodynamic stress incontinence between smokers and nonsmokers using a case-control method (Bump, 1994). In this study, 71 smokers and 118 nonsmokers were compared following a complete urogynecologic evaluation. Smokers were found to have stronger urethral sphincters and generated a greater increase in bladder pressure with coughing, but similar findings with respect to urethral mobility and pressure transmission ratios were found when compared with nonsmokers. Approximately 5% of women will develop a symptomatic stone by the age of 70 years. These may be related to metabolic abnormalities, such as gout or errors of calcium metabolism, but usually relate to chronic infection and stasis of urine. Other risk factors for calculi in women include pregnancy, during which time the urinary tract becomes dilated and stasis is more common, a history of kidney stones or family history, certain medications, excessive vitamin C intake, low calcium intake, chronic diarrhea, and dehydration. Pain occurs on the side of the stone and varies from a dull ache to severe paroxysms of pain, called renal colic. Flank pain, lower abdominal pain, and groin pain can occur; the location can vary as the stone moves down the ureter with radiation of pain to the groin. Ultrasound misses small stones but is recommended for pregnant women and is increasingly recommended for initial screening as no radiation is used. Various treatment modalities are available, including observation with pain medications and fluids awaiting spontaneous passage, endoscopic removal, surgical removal, and destruction of the stone with laser or shockwave lithotripsy. The principal consideration, however, should be correction of the basic problem that caused the stone. Urgent intervention is necessary if the woman has fever, chills, nausea and vomiting, and pain uncontrolled by narcotics. Another area of interest involves racial and ethnic differences with respect to the presence of urinary incontinence. Black women with urinary incontinence have a different distribution of symptoms and different reasons for their incontinence than white women. Black women had a significantly lower prevalence of pure urodynamic stress incontinence than white women. The findings may possibly relate to differences in collagen and connective tissue. Several other studies have found a higher prevalence of urinary incontinence in nonHispanic white women and Mexican-Americen woman compared with rates in Asian and black women, although at least two studies have found no difference between racial or ethnic groups. Obesity has a strong association with incontinence and, for every five-unit increase in body mass index, the risk increases. These women reported a higher number of weekly incontinence episodes than women without depressive symptoms, as well as more bothersome symptoms and poorer quality of life (Melville, 2009). Epidemiologic studies have suggested increased risk with hysterectomy but short-term clinical studies have not, so more research is needed to clarify this issue. Vaginal childbirth and higher fetal weight are risk factors in younger women, but the effect diminishes in older women, possibly because the neuromuscular decline with aging becomes a more important factor. The prevalence of incontinence is significantly higher for women in nursing homes and women with cognitive impairment and poor mobility. When urine leakage is observed during a urodynamic study, with an increase in intraabdominal pressure and without a detrusor contraction, it is called urodynamic stress incontinence (Haylen, 2010). Stress urinary incontinence is a common condition for which nearly 14% of women in the United States will undergo surgery at some point (Wu, 2014). Injury, particularly trauma from obstetric delivery, has been implicated in stress incontinence. The odds ratio of stress urinary incontinence in parous compared with nulliparous women is threefold (Hansen, 2012); the odds ratio after vaginal compared with cesarean delivery is twofold (Lukacz, 2006). Meyer and colleagues studied 149 patients during pregnancy and 9 weeks postpartum. They found that 36% of women who were delivered by forceps and 21% who delivered spontaneously suffered from urinary incontinence (Meyer, 1998). Bladder neck mobility was significantly increased after all vaginal births, but bladder neck position at rest was only lowered in the forceps group. Considering other forms of pelvic floor trauma, Nygaard studied female American Olympic athletes and could not find a difference between the low-impact (swimmers) and high-impact (gymnasts, track and field performers) athletes with respect to the development of stress incontinence later in life (Nygaard, 1997). Because that support layer is attached to the pelvic wall via the arcus tendineus fascia pelvis and levator ani, the urethra is compressed by increases in abdominal pressure. Urethral hypermobility, which can be measured using a "Q-tip test," corresponds to the loss of the backstop support at the bladder neck. The Q-tip test involves placing a cotton swab into the urethra to the bladder neck and observing the angle that the urethra makes with the horizontal during a strain maneuver. A large excursion from the horizontal suggests defects in the supports of the urethra but not a specific urologic diagnosis.
These are discussed in the "Intrinsic Sphincter Deficiency" section of the chapter androgen hormone 17p order genuine rogaine 5 on-line. A maximum Q-tip excursion angle greater than 30 degrees suggests hypermobility and is associated with higher success rates after midurethral sling surgery. Urethral mobility can also be evaluated using the prolapse quantification system, visualization, palpation, or ultrasonography. Note how the levator ani muscles support the rectum, vagina, and urethrovesical neck. Also note how the endopelvic fascia next to the urethra attaches to the levator ani muscle; contraction of the levator muscle leads to elevation of the urethrovesical neck. Midurethral sling and urethral bulking agents will be discussed in more detail in the Surgical Management section. Stress incontinence may occur with injury to or degeneration of the urethral support system or urethral sphincter mechanism, and it is likely that most women with incontinence have elements of both problems. Bladder neck funneling, position, and hypermobility can be evaluated by perineal ultrasound. Although the clinical uses to date are limited, it is useful in studying the pelvic structures in continent and incontinent women, and it may have clinical applications in the future. Ultrasound examination of the urethral sphincter may also be helpful in measuring length, thickness, and striated muscle volume. Athanasiou and associates, using threedimensional ultrasound, have shown that women with stress urinary incontinence have significantly shorter, thinner, and smaller volumes of striated muscle in their urethras than continent women of comparable ages and parity (Athanasiou, 1999). Women with anterior vaginal wall prolapse often have urethral hypermobility but may or may not have stress incontinence. If they have stress incontinence, they must have some urethral sphincter compromise along with the hypermobility. It is also possible that the prolapse kinks off the urethra, thus maintaining continence, and that reduction of the prolapse will unmask occult stress incontinence. Prolapse reduction stress testing, in which the patient is asked to cough with a comfortably full bladder while the prolapse is reduced, can help predict which women are likely to have stress incontinence after prolapse surgery. Multichannel urodynamic testing should be reserved for women with complicated stress incontinence, such as unclear diagnosis, large urge component, or prior anti-incontinence surgery. All women should be offered conservative treatments first, and then surgery can be pursued if she fails or declines nonoperative treatments. The first-line treatment is pelvic floor muscle training directed toward the strengthening of the levator ani and pubococcygeal muscles, which affect the urethral closure mechanism. The woman can be instructed on how to contract these muscles by being told to attempt to stop the urinary stream while she is voiding. Importantly, after she learns which muscles to contract, she should perform the exercises at other times without any relationship to voiding because contracting her pelvic floor muscles during voiding could lead to voiding dysfunction. Pelvic muscle exercise success is improved with specific training by a health professional or physical therapist. Improvement in the muscular supports may be enough to overcome the anatomic weakness that originally led to the stress incontinence. Although these exercises have a number of modifications, one useful application is to teach the woman to contract these muscles slowly, 8 to 12 times, for a count of 6 to 8 seconds each, and to repeat this series for three sets daily. A meta-analysis of 12 randomized controlled trials found that at least 24 contractions a day for 6 weeks resulted in decreased incontinence episodes; more contractions did not result in additional improvement (Choi, 2007). Better efficacy was noted in younger women with stress incontinence than older women and women with mixed or urgency incontinence. A Cochrane Database review of pelvic floor muscle training analyzed 21 trials involving 1281 women (Dumoulin, 2015). Women who did pelvic floor muscle training were 8 times more likely to be cured and 17 times more likely to be cured or improved compared with the control group. With no serious adverse effects, pelvic floor muscle training should be offered as a first-line conservative management program for women with urinary incontinence. Many patients enjoy prolonged relief, even after stopping pelvic floor muscle exercises. Bø and Talseth studied 23 women who participated in a 6-month intensive pelvic floor muscle exercise routine and noted that 5 years later, 75% demonstrated no leakage during a stress test and 70% were satisfied with their continence (Bø, 1996). Of these patients, 70% were still exercising their pelvic muscles at least once weekly and demonstrated pelvic floor muscle strength. These authors noted improvement of incontinence, not only in patients with stress incontinence but also in those with urge and mixed urinary incontinence. It is important to ensure that the woman is aware of how to perform the exercises correctly. In a study by Bump and coworkers in which 47 women were given simple verbal or written instructions, 23 (49%) had an ideal Kegel effort signified by an increase in force of the urethral closure. However, 12 subjects (25%) were performing the technique poorly and in such a way that incontinence might be promoted (Bump, 1991). The authors recommended a demonstration approach rather than a written or verbal approach. This involves a set of cones of increasing weight that require pelvic muscle contraction to hold them within the vagina. Peattie and associates demonstrated an improvement in 70% of 30 premenopausal women with stress incontinence after only 1 month of exercise. A correlation was noted between decreased urine loss and the ability to retain cones of increased weight (Peattie, 1988).
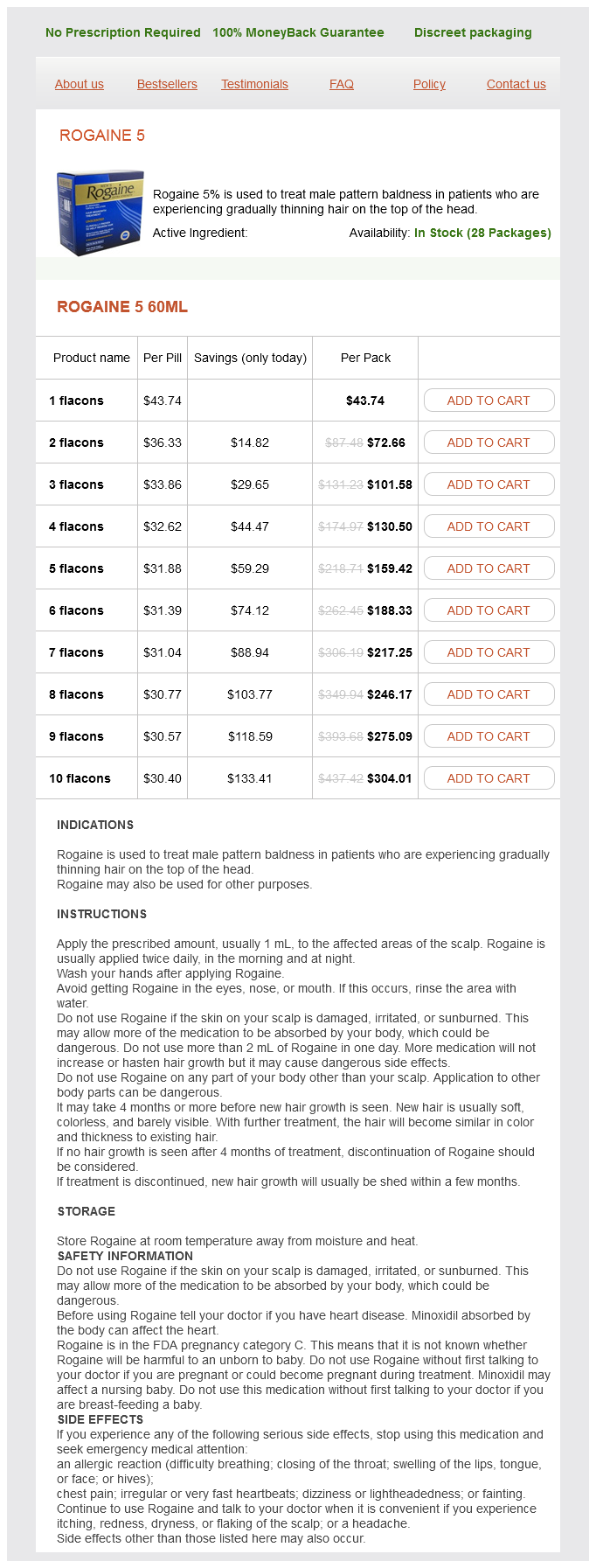
Rogaine 5 Dosage and Price
Rogaine 5 60ml
- 1 flacons - $43.74
- 2 flacons - $72.66
- 3 flacons - $101.58
- 4 flacons - $130.50
- 5 flacons - $159.42
- 6 flacons - $188.33
- 7 flacons - $217.25
- 8 flacons - $246.17
- 9 flacons - $275.09
- 10 flacons - $304.01
In this large prospective study mens health 10k glasgow purchase rogaine 5 online now, a gynecologic pathologist reviewed cases with a diagnosis of complex hyperplasia with atypia. One third of the cases were confirmed as complex atypical hyperplasia, one third were deemed to be "less than" complex atypical hyperplasia, and one third were considered endometrial cancers. This variability in diagnosis should be considered when determining treatment for these patients. Endometrial hyperplasia is believed to result from an excess of estrogen or an excess of estrogen relative to progestin, such as occurs with anovulation. Kurman and Norris introduced terminology that the World Health Organization has adopted to describe endometrial hyperplasias and their premalignant potential. There are two important separate categories: atypical hyperplasia and hyperplasia without atypia. In these categories, two subgroups are recognized: simple hyperplasia and complex hyperplasia (Table 32. Behavior of endometrial hyperplasia: a long-term study of "untreated" hyperplasias in 170 patients. Kurman and associates studied 170 patients with endometrial hyperplasia diagnosed by D&C at least 1 year before hysterectomy (Kurman, 1985). Overall, complex atypical hyperplasias had the highest risk of progression to carcinoma. Simple hyperplasia had a 1% rate of progression to cancer, complex hyperplasia without atypia had a 3% rate of progression to cancer, and complex atypical hyperplasia had a 29% rate of progression to cancer. In addition to possible progression to cancer, 40% of women who undergo hysterectomy for complex atypical hyperplasia have a concurrent endometrial cancer in their hysterectomy specimen. This high rate of cancer suggests that complex atypical hyperplasia may frequently be present with low-grade endometrial cancer and that endometrial sampling may not identify an endometrial cancer when admixed with a complex atypical hyperplasia. Clearly, there is a spectrum of histology that makes a definitive diagnosis of complex atypical hyperplasia difficult, and the clinician must be aware of this fact when planning management strategies. In younger patients, hyperplasia may develop during anovulatory cycles and may even be detected after prolonged periods of oligomenorrhea or amenorrhea. It can occur at any time during the reproductive years but is most common with abnormal bleeding in the perimenopausal period. Premenopausal women with irregular vaginal bleeding and postmenopausal women with any vaginal bleeding should be evaluated with an office endometrial sampling or a D&C. The office sampling instruments, such as a thin plastic Pipelle, are introduced through the cervical os into the endometrial cavity and can provide very accurate information (see Chapter 10). Many patients tolerate office endometrial sampling without an analgesic agent, but paracervical block can be an effective anesthetic aid, particularly in nulliparous women. Some patients benefit from an oral nonsteroidal antiinflammatory drug taken approximately 30 minutes before biopsy. Transvaginal ultrasonography has been evaluated as an adjunct for the diagnosis of endometrial hyperplasia and cancer. These studies have been performed in different populations, including asymptomatic postmenopausal women, women taking tamoxifen, and women presenting with postmenopausal bleeding. Langer and associates, in a study of 448 asymptomatic postmenopausal women, found a threshold of 5-mm endometrial thickness had only a 9% predictive value for detecting endometrial abnormalities (Langer, 1997). Its greater use was eliminating the diagnosis of neoplasia for those with thickness less than 5 mm (negative predictive value of 99%). These findings were confirmed in a literature review by Smith-Bindman and colleagues, who found that 96% of women with carcinoma had an abnormal ultrasound scan (endometrial thickness >5 mm). Conversely, 8% of postmenopausal women with an abnormal scan had no histologic abnormality, and the percentage grew to 23% for those on hormone replacement therapy. However, both of these studies were conducted in postmenopausal asymptomatic women. One case of hyperplasia and one of carcinoma were found, and most patients had atrophic endometrium. The authors concluded that the false-positive rate of transvaginal ultrasonography in this population was too high to warrant its use as a screening modality, and they recommended using irregular vaginal bleeding as an indication for endometrial sampling (Cecchini, 1996). Similarly, Love and associates found that endometrial thickness is not necessarily a useful guide for biopsy in tamoxifen. In the study by Barakat and colleagues, routine screening with transvaginal ultrasonography was not of value, and they concluded that sampling should be done if the patient experiences bleeding. In postmenopausal women with any vaginal bleeding, Gull and colleagues found that an endometrial stripe of less than 4 mm had a 100% negative predictive value (Gull, 2000). A finding of endometrial thickness less than 4 mm is a reasonable predictor of lack of endometrial pathology, even in a postmenopausal patient with bleeding. However, persistent vaginal bleeding should lead to endometrial sampling regardless of the ultrasound findings. Endometrial ablation is sometimes undertaken to control severe uterine bleeding (see Chapter 26). However, pathologic evaluation of the endometrium should be performed before ablation in order to rule out an underlying endometrial hyperplasia or cancer. For women with simple hyperplasia or complex hyperplasia without atypia, the risk of developing endometrial cancer is low, 1% and 3%, respectively. A diagnostic D&C can also be therapeutic, and progestins or combination oral contraceptive agents will likely be effective. For complex atypical hyperplasia, the risk of developing endometrial cancer may be 29%, and, as stated previously, a concurrent endometrial cancer may be present. Women who desire preservation of childbearing function are treated with high-dose progestin therapy, usually megestrol acetate 40 mg three times daily to four times daily. In these patients, the risk factors that led to the development of complex atypical hyperplasia are likely to remain.
© 2025 Adrive Pharma, All Rights Reserved..