General Information about Repaglinide
Overall, Repaglinide has turn out to be an necessary and widely prescribed medication within the management of kind 2 diabetes. It provides an effective option for people who are struggling to control their blood sugar ranges and may help to stop or delay the serious problems related to uncontrolled diabetes. However, you will need to take it as directed and to proceed monitoring blood sugar ranges to ensure its effectiveness. As with any medicine, you will want to focus on any concerns or potential interactions with a healthcare supplier.
Repaglinide, commonly known by its model name Prandin, is a drugs used in the administration of type 2 diabetes. It belongs to the class of drugs known as meglitinides, which work by stimulating the discharge of insulin from the pancreas to manage blood sugar ranges. It is an efficient and widely prescribed medication for individuals with sort 2 diabetes who're unable to manage their blood sugar ranges via diet and exercise alone.
In medical trials, Prandin has been proven to be effective in managing blood sugar levels in individuals with type 2 diabetes. It has also been discovered to be well-tolerated and has a low threat of side effects. It can be utilized by people of all ages, including these over the age of 65, and has not been found to have any important drug interactions with different generally prescribed medicines.
Prandin works by focusing on the beta cells within the pancreas, that are answerable for producing insulin. It stimulates these cells to produce and release more insulin, thus helping to lower blood sugar levels. Unlike some other diabetes medicines, Prandin doesn't cause the body to produce more insulin; as a substitute, it really works by increasing the amount of insulin that is already being produced.
One of the primary advantages of Repaglinide is that its results are short-lived, that means that it only stays in the body for a brief period of time. This is helpful for people who have meals at irregular times or who might skip meals, as Prandin may be taken nearer to mealtime than other diabetes medicines. However, this additionally implies that you will want to take the treatment persistently and not to miss doses.
In addition to being used alone, Prandin may also be prescribed together with different diabetes medications, corresponding to metformin. It can be especially helpful for people who usually are not capable of control their blood sugar ranges with metformin alone.
Prandin is normally taken orally, before every meal. The dosage will range depending on the person's blood sugar levels and other components. It is important to take this medicine as prescribed by a doctor, and by no means to regulate the dosage with out consulting a healthcare provider first. Prandin should be taken about quarter-hour earlier than a meal to allow enough time for it to begin working.
As with any medicine, Prandin does have potential unwanted effects. The most typical ones include low blood sugar ranges, also called hypoglycemia, and weight achieve. These unwanted facet effects may be managed with correct monitoring and changes to the dosage if essential. It is important to speak any modifications in unwanted effects or concerns with a healthcare supplier.
Type 2 diabetes is a continual situation by which the physique is unable to correctly make the most of the insulin it produces or is unable to provide enough insulin to control blood sugar levels. This ends in high blood sugar levels, which may lead to critical and doubtlessly life-threatening problems similar to heart illness, stroke, and nerve injury.
High levels of disease activity type 2 diabetes quiz questions order repaglinide 2 mg without a prescription, lupus nephritis, and the presence of the lupus anticoagulant each significantly increases the risk for prematurity and spontaneous abortion. Skin rashes commonly occur in pregnancy; facial blush, palmar erythema, and mild alopecia should be distinguished from a true lupus-related rash. Arthralgia, myalgia, and backaches are normal symptoms of pregnancy and can usually be managed conservatively with acetaminophen and physical therapy. True synovitis does not occur in normal pregnancy and can be related to a lupus flare. Mild anemia and thrombocytopenia are normal variants of pregnancy, but severe anemia and thrombocytopenia may be an indication of an immune-mediated process, such as immune-mediated thrombocytopenia or hemolytic anemia. The presence of leukopenia and lymphopenia should raise the suspicion of a systemic autoimmune process. In normal pregnancy, the glomerular filtration rate increases from 100 to 150 mL/min, with intravascular volume increasing by one third. Update on safety during pregnancy of biological agents and some immunosuppressive anti-rheumatic drugs. Of the three types of antiphospholipid antibodies, the lupus anticoagulant appears to be the strongest indicator of potential pregnancy complications. A positive first trimester lupus anticoagulant can be used to predict risk for poor outcomes. Although maternal thrombosis or severe or early preeclampsia can occur, it is common for the mother to be completely asymptomatic while trouble is brewing for the developing fetus. The pathogenesis behind the morbidity and mortality associated with antiphospholipid antibodies is not fully understood, but harm from antiphospholipid antibodies occurs at the level of the placenta from placental thrombosis, direct damage to the placenta by inflammation, or defective placentation. Antiphospholipid antibodies likely cause complement activation at the placenta; this in turn activates tissue factor, which leads to a burst of inflammation from neutrophils and oxidative stress. Other models suggest that fetal loss is caused by the binding of anti2-glycoprotein antibodies to trophoblast cells, which inhibits placental growth. Nevertheless, some rheumatologists prefer to prescribe low-dose aspirin for these patients. Women with a prior thrombosis are at high risk for recurrent thrombosis in pregnancy and pregnancy complications. Despite the risks associated with the presence of antiphospholipid antibodies, live births have been reported in more than 50% to 74% of such patients when treatment was initiated. Preeclampsia is defined as new-onset systolic blood pressure of more than 140 mm Hg or diastolic blood pressure of more than 90 mm Hg in the setting of proteinuria (more than 300 mg of protein per 24 hours) after the 20th week of pregnancy. Physiologically, some degree of proteinuria, up to 300 mg of protein over 24 hours, is considered a normal variant of pregnancy. If a woman had some proteinuria before pregnancy, even an increase to 1 g can occur in the absence of lupus nephritis. In a prospective study of pregnancy in women with lupus, 64% of those patients who had a history of nephritis (regardless of current glomerular filtration rates) experienced preeclampsia compared with 14% of patients without nephritis. Low-dose aspirin therapy throughout pregnancy has been shown to decrease preeclampsia and preterm birth in women at risk for these complications. Although studies of aspirin have not been conducted in lupus pregnancy, low-dose aspirin is a reasonable approach to prevent preterm birth and preeclampsia. The most common manifestation is a photosensitive rash that appears in the infant around 4 to 6 weeks after birth and occurs in up to 20% of infants born to mothers with the anti-Ro antibody. Although this can occur as the classic malar butterfly rash, more commonly it consists of nonscarring, large, circular macules over the face, trunk, and extremities. The rash usually disappears on its own but can be treated with topical corticosteroids. Hematologic abnormalities, including thrombocytopenia and neutropenia, and hepatic abnormalities such as asymptomatic transaminitis can occur in 10% to 15% of cases. These subclinical abnormalities often dissipate soon after delivery, and routine screening of newborns for these abnormalities is not recommended. The most serious but rare complication of neonatal lupus, however, is congenital heart block, believed to affect approximately 2% of offspring exposed to anti-Ro antibodies. Because congenital heart block usually develops between 18 and 24 weeks of gestation, some experts recommend serial fetal echocardiography during this period. Premature atrial contractions and even moderate pericardial effusions should be taken seriously because they may foreshadow the development of congenital heart block. If first- or second-degree heart block is detected, treatment with dexamethasone may be initiated immediately, with some small case series describing reversal of early heart block. The obstetrician should also be alerted to organ system complications that could impact delivery. For instance, in lupus patients with a history of avascular necrosis of the hips, a spontaneous vaginal delivery may cause musculoskeletal damage, in which case a planned cesarean section is warranted. Maternal breast milk production may be limited for mothers receiving high-dose steroids or in pregnancies that result in preterm birth. Decrease in pregnancy loss rates in patients with systemic lupus erythematosus over a 40-year period. Systemic lupus erythematosus and pregnancy outcomes: an update and review of the literature. The effect of lupus nephritis on pregnancy outcome and fetal and maternal complications. Has there been any progress made on pregnancy outcomes among women with pulmonary arterial hypertension
Inflammatory eye disease even developed for the first time in five patients while taking etanercept blood sugar 79 repaglinide 2 mg purchase on line. Total resolution of anterior uveitis was achieved with infliximab as the only antiinflammatory drug in all but one patient. Second, the repair tissue becomes ossified, which is made easier if inflammation is no longer present. Future studies need to show whether this assumption about the sequence of events is correct. Most data available are derived from studies that have tested infliximab, etanercept, or adalimumab for the treatment of psoriasis or psoriatic arthritis (see also Chapter 131) and Crohn disease. In Crohn disease, whereas infliximab and adalimumab were shown to be highly effective for different manifestations of active disease, etanercept failed to be superior to placebo in a controlled trial. Although juvenile forms normally occur initially with a predominance of peripheral manifestations (enthesitis and peripheral arthritis), the full picture of typical axSpA develops later in many juvenile patients. In two small open-label studies, both infliximab and etanercept showed good efficacy in patients with juvenile SpA or enthesitis-related arthritis. One recent double-blind placebo-controlled trial showed highly significant improvement in a variety of clinical parameters in the infliximab-treated group compared with the placebo group. Depending on the symptoms and progression of the arthritis, this patient could become a candidate for hip replacement. However, patients with axSpA are normally younger than those with the other two diseases and less frequently have been treated with glucocorticoids or immunosuppressive drugs. Thus, the number and severity of side effects can be expected to be at least no higher than in other chronic inflammatory diseases and might even be lower. However, implementation of the usual precautions for and contraindications to biologic therapy should be followed. Infections, including opportunistic infections, can occur in a small percentage of patients, and a small increase in risk for the development of lymphoproliferative disorders cannot be excluded at this stage. Allergic reactions occur, and neurologic events and congestive heart failure have been reported occasionally. The reduced flexibility in combination with osteoporosis of the spine as a consequence of lack of movement and local and systemic inflammation renders the spine susceptible to a variety of complications, including fracture and dislocation, sometimes even after minor trauma. Spinal instability can also occur as a consequence of a severe Andersson lesion (diskovertebral erosions and destruction). The three commonly performed procedures are opening-wedge osteotomy, polysegmental wedge osteotomy, and closing-wedge osteotomy. Atlantoaxial and atlantooccipital subluxation and spinal stenosis can be other reasons for surgical interventions. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Baseline radiographic damage, elevated acute-phase reactant levels, and cigarette smoking status predict spinal radiographic progression in early axial spondylarthritis. Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. Development and preliminary validation of the spondyloarthritis research consortium of Canada magnetic resonance imaging sacroiliac joint structural score. Combined spa-exercise therapy is effective in patients with ankylosing spondylitis: a randomized controlled trial. Evaluation of the efficacy of etoricoxib in ankylosing spondylitis: results of a fifty-two-week, randomized, controlled study. The efficacy of cyclooxygenase-2 inhibition by etoricoxib and naproxen on the axial manifestations of ankylosing spondylitis in the presence of peripheral arthritis. Retardation of ossification of the lumbar vertebral column in ankylosing spondylitis by means of phenylbutazone. Non-steroidal anti-inflammatory drugs reduce radiographic progression in patients with ankylosing spondylitis: a randomized clinical trial. Effect of non-steroidal anti-inflammatory drugs on radiographic spinal progression in patients with axial spondyloarthritis: results from the German Spondyloarthritis Inception Cohort. Benefits and risks of ankylosing spondylitis treatment with nonsteroidal antiinflammatory drugs. Efficacy of oral prednisolone in active ankylosing spondylitis: results of a double-blind, randomised, placebo-controlled short-term trial. Efficacy of sulfasalazine in patients with inflammatory back pain due to undifferentiated spondyloarthritis and early ankylosing spondylitis: a multicentre randomised controlled trial. No efficacy of subcutaneous methotrexate in active ankylosing spondylitis-a 16-week open-label trial. The comparative one-year performance of anti-tumor necrosis factor alpha drugs in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: results from a longitudinal, observational, multicenter study. Double-blind, randomised, placebo-controlled study of leflunomide in the treatment of active ankylosing spondylitis. A, six-month randomized, controlled, double-blind, dose-response comparison of intravenous pamidronate (60 mg versus 10 mg) in the treatment of non-steroidal anti-inflammatory drugrefractory ankylosing spondylitis. Assessment of short-term symptomatic efficacy of tocilizumab in axial radiographic spondyloarthritis: results of randomised, placebo-controlled trials. Different, response to rituximab in tumor necrosis factor blockernaive patients with active ankylosing spondylitis and in patients in whom tumor necrosis factor blockers have failed: a twenty-four-week clinical trial. Use of immunohistologic and in-situ hybridization techniques in the examination of sacroiliac joint biopsy specimens from patients with ankylosing spondylitis. Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial.
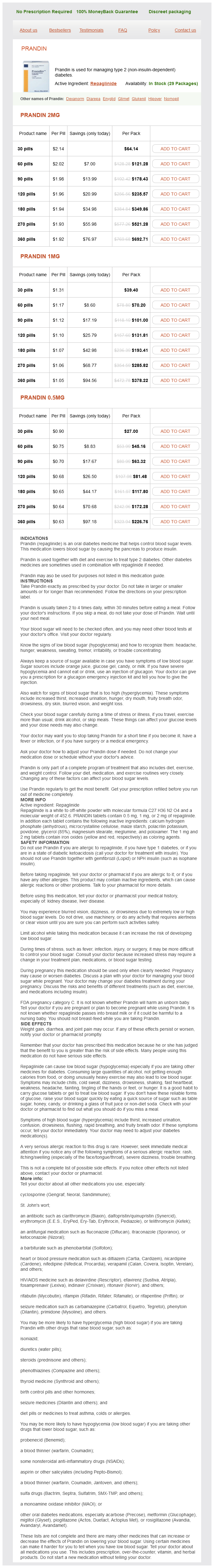
Repaglinide Dosage and Price
Prandin 2mg
- 30 pills - $64.14
- 60 pills - $121.28
- 90 pills - $178.43
- 120 pills - $235.57
- 180 pills - $349.86
- 270 pills - $521.28
- 360 pills - $692.71
Prandin 1mg
- 30 pills - $39.40
- 60 pills - $70.20
- 90 pills - $101.00
- 120 pills - $131.81
- 180 pills - $193.41
- 270 pills - $285.82
- 360 pills - $378.22
Prandin 0.5mg
- 30 pills - $27.00
- 60 pills - $45.16
- 90 pills - $63.32
- 120 pills - $81.48
- 180 pills - $117.80
- 270 pills - $172.28
- 360 pills - $226.76
Activation or injury of the endothelium can result in an imbalance of these substances and a proinflammatory diabetes insipidus glycosuria buy repaglinide with visa, procoagulant environment more susceptible to the actions of noradrenaline and endothelialderived vasoconstrictors. Epidemiologic studies consistently show higher prevalence in women, particularly between menarche and menopause, after which symptoms often abate. In addition, estrogen-only hormone replacement therapy has been linked with Raynaud attacks, and variations in blood flow according to the menstrual cycle have been described. However, the mechanisms by which hormones contribute to vascular tone are not fully understood. They demonstrated that attacks persist despite local analgesia of digital sympathetic nerves and to some extent after sympathectomy. Important symptoms to elucidate are photosensitivity, mouth ulcers, tightening of the skin, and dryness of eyes or mouth. A full physical examination should be directed to look for any obstructive vascular disease and for signs of associated autoimmune conditions. Look for signs of poor tissue nutrition such as trophic changes in the nails, hacks, or ulcers. Symptoms include numbness, coldness, and pain, which are secondary to ischemia that can be severe enough to result in digital ulceration, gangrene, and loss of digits. During the reactive hyperemic stage, patients experience an unpleasant burning sensation or tingling. The most severely affected patients may experience year-round restrictions in daily activity. The asymmetric involvement and the presence of telangiectasia point to a secondary cause. A decrease in pressure greater than 20 to 25 mm Hg after cold challenge is usually significant. First, the patient must be warm before the recordings with the starting digital pressure as near brachial pressure as can be achieved. Second, in premenopausal women, assessment should be avoided in midcycle because poor blood flow can occur at the time of ovulation. Third, all vasoactive medications should be stopped 24 hours before the test, and the test should be avoided when the patient is in the reactive hyperemic phase. Ideally, patients should not have had a vasospastic attack on the day of the test. Further imaging for suspected thoracic outlet syndrome includes thoracic outlet chest radiography or magnetic resonance angiography. Patients should be referred to secondary care if history, examination, or initial investigations give cause for concern. This technique involves direct visualization of the nail-fold capillary vessels by an experienced assessor using a digital camera attached to a computer. Initial treatment in mild disease is conservative, and drug treatment is best avoided. Education is important, and a specialist rheumatology nurse and occupational therapist can provide useful advice, as can patient self-help groups. Simple suggestions such as keeping the trunk warm and providing occupational therapy aids such as key holders to use when the fingers are numb can help. Electrically heated gloves and socks and chemical hand warmers are the perfect solution for some patients, though battery weight can make these unattractive. Calcium channel blockers Dihydropyridine calcium channel blockers, in particular nifedipine, in a long-acting preparation have now become the gold standard. The short-acting preparations produce violent vasodilatory side effects and last only a few hours; they should be avoided, if possible. Nifedipine has been found to be useful in decreasing the frequency and severity of vasospastic attacks and improves the objective measures of blood flow after cold exposure. These effects usually disappear with continued treatment; therefore, unless they are intolerable, the patient should persevere for at least 2 weeks before stopping. If side effects necessitate discontinuation, other calcium channel blockers such as amlodipine or lercanidipine can be tried. These showed a 33% and 35% reduction in severity of the attacks in primary and secondary disease, respectively, as well as a moderate reduction in the frequency of attacks. Inositol nicotinate (a nicotinic acid derivative) and naftidrofuryl oxalate (a mild peripheral vasodilator with a serotonin receptor antagonist effect) have produced some encouraging results in mild to moderate disease, as has thymoxamine. Another role of these medications is to use them as adjuncts to calcium channel blockade when adverse effects prevent the achievement of high dosage of the latter. Prostaglandin delivery through the skin has also been studied, but no transdermally applied prostaglandin has achieved license status as yet. This could be repeated every 6 weeks to cover the cold weather in severe cases, especially if associated with critical ischemia or digital ulceration, and should be given via a central line. Furthermore, in addition to the vasodilatory side effects in common with other drugs, the possibility of liver toxicity has to be considered, and the results of a current major trial are awaited. A recent metaanalysis of five studies supported effectiveness of this therapy and suggested that larger controlled trials with improved study design are warranted. Topical nitrates are one example where a number of small studies show positive results but robust evidence does not exist. This could be tried if hypotension is a problem with oral medication, but care should be taken that the drug is not transferred elsewhere.
© 2025 Adrive Pharma, All Rights Reserved..