General Information about Rebetol
Rebetol, additionally recognized by its generic name Ribavirin, is an antiviral treatment that's specifically designed to treat continual hepatitis C. It belongs to a category of medication called nucleoside analogs, which work by stopping the virus from reproducing in the body. This drug is often utilized in mixture with other medications, similar to interferon alpha, to enhance its effectiveness.
Hepatitis C is a severe viral infection that affects the liver. It could cause liver harm, cirrhosis, and even liver most cancers if left untreated. In latest years, there was a big enhance in the number of individuals affected by this disease. According to the World Health Organization, round seventy one million people worldwide have continual hepatitis C, and approximately 399,000 people die annually as a outcome of associated complications.
Rebetol is on the market in capsule type and is to be taken orally. The dosage and period of treatment depend on varied elements, similar to the sort of hepatitis C, the extent of liver harm, and the individual's response to the treatment. It is crucial to comply with the prescribed regimen and full the complete course of treatment to attain the most effective results.
It is essential to notice that Rebetol just isn't efficient in treating different viral infections, such because the common cold or the flu. It is particularly designed to target and treat the hepatitis C virus and should only be used underneath the steerage of a healthcare professional.
Luckily, there are medicines out there to treat hepatitis C and prevent its detrimental consequences. One of essentially the most widely used drugs for this function is Rebetol. In this text, we are going to take a extra in-depth look at what Rebetol is, the method it works, and its function in treating hepatitis C.
One of the most significant advantages of Rebetol is its capacity to target multiple genotypes of the hepatitis C virus. There are six known genotypes of the virus, and Rebetol has proven efficacy towards all of them. This is essential because completely different regions of the world have completely different predominant genotypes, and Rebetol can provide a remedy possibility for a variety of patients.
In conclusion, Rebetol is a broadly used antiviral treatment for the therapy of chronic hepatitis C. It is effective in opposition to all genotypes of the virus and has shown promising results. However, it's not a cure and must be utilized in combination with other medications as prescribed by a physician. If you've been identified with hepatitis C, make sure to consult your healthcare provider about the potential use of Rebetol in your remedy plan.
Like all medications, Rebetol also carries the danger of unwanted effects. The most common ones reported include fatigue, headache, nausea, and anemia. In some circumstances, it might possibly also trigger more extreme adverse reactions such as coronary heart issues and psychological health issues. It is necessary to debate any potential side effects with a healthcare skilled earlier than beginning the treatment.
However, Rebetol is not a cure for hepatitis C. It can help to regulate and suppress the virus, however it doesn't eliminate it from the physique. Therefore, it's essential to continue common check-ups and monitoring of liver operate even after completing the remedy to stop a relapse.
Vaginal birth and de novo stress incontinence: relative contributions of urethral dysfunction and mobility treatment regimen order genuine rebetol. Prevention of urinary incontinence by behavioral modification program: a randomized, controlled trial among older women in the community. Transdermal Oxybutynin Study Group: comparative efficacy and safety of transdermal oxybutynin and oral tolterodine versus placebo in previously treated patients with urge and mixed urinary incontinence. Urinary incontinence prevalence: results from the National Health and Nutrition Examination Survey. Estrogen therapy in the management of urinary incontinence in postmenopausal women: a meta-analysis. Percutaneous tibial nerve stimulation effects on detrusor overactivityincontinence are not due to a placebo effect: a randomized, double-blind, placebo controlled trial. Breaking the cycle of pain in interstitial cystitis/painful bladder syndrome: toward standardization of early diagnosis and treatment: consensus panel recommendations. Effect of amitriptyline on symptoms in treatment of naïve patients with interstitial cystitis/ painful bladder syndrome. A randomized, controlled trial evaluating 2 techniques of postoperative bladder testing after transvaginal surgery. Microbiology of the urethral (frequency and dysuria) syndrome: a controlled study with a 5-year review. Discontinuation rates of anticholinergic medications used for the treatment of lower urinary tract symptoms. Comparative studies of the human external sphincter and periurethral levator ani muscles. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. Familial risk of urinary incontinence in women: a population based cross sectional study. Effectiveness of anticholinergic drugs compared with placebo in the treatment of overactive bladder: systematic review. The modified Pereyra procedure in recurrent stress urinary incontinence: a 15-year review. Surgically corrected urethral diverticula: long-term voiding dysfunction and reoperation rates. Randomised trial of laparoscopic Burch colposuspension versus tension-free vaginal tape: long-term follow up. Cognitive, behavioral, and physiological changes in Alzheimer disease patients as a function of incontinence and medications. The Q-tip test: Standardization of the technique and its interpretation in women with urinary incontinence. Artificial urinary sphincter for recurrent/severe stress incontinence in women: urogynecologic perspective. Long-term results of the tension-free vaginal tape operation in an unselected group of 129 stress incontinent women. National Institutes of Health state-ofthe-science conference statement: prevention of fecal and urinary incontinence in adults. Efficacy of sacral neuromodulation for symptomatic treatment of refractory urinary urge incontinence. Hormonal manipulation in women with chronic, cyclic irritable bladder symptoms and pelvic pain. Randomized controlled multisite trial of injected bulking agents for women with intrinsic sphincter deficiency: mid-urethral injection of Zuidex via the Implacer versus proximal urethral injection of Contigen cystoscopically. Guidelines for the evaluation and treatment of recurrent urinary incontinence following pelvic floor surgery. Management of urinary incontinence in Medicare managed care beneficiaries: results from the 2004 Medicare Health Outcomes Survey. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Prevalence of comorbid psychiatric illness and its impact on symptom perception, quality of life, and functional status in women with urinary incontinence. A randomized comparison of tensionfree vaginal tape and endopelvic fascia plication in women with genital prolapse and occult stress urinary incontinence. Duloxetine vs placebo in the treatment of stress urinary incontinence: a four-continent randomized clinical trial. How widespread are the symptoms of an overactive bladder and how are they managed Evolving trends in the successful management of interstitial cystitis/painful bladder syndrome. A 2-year observational study to determine the efficacy of a novel single incision sling procedure (Minitape) for female stress urinary incontinence. Randomized double-blind trial of terodiline in the treatment of urge incontinence in women. Updated systematic review and metaanalysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Prevalence of urinary incontinence and associated risk factors in nursing home residents: a systematic review. Long-term results of a fascia lata suburethral patch sling for severe stress urinary incontinence.
The place of D-dimer testing in an integrated approach of patients suspected of pulmonary embolism medicine 5 rights rebetol 200mg purchase online. A randomized comparison of secondary closure and secondary intention in patients with superficial wound dehiscence. American College of Chest Physicians: the perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Algorithm for treatment of postoperative incisional groin pain after cesarean delivery or hysterectomy. Femoral nerve palsy as a complication of vaginal hysterectomy: review of the world literature. Pelvic fluid collections by sonography and febrile morbidity after abdominal hysterectomy. A comparison between preincisional and postincisional lidocaine infiltration and postoperative pain. Outcomes of octogenarians and nonagenarians in elective major gynecologic surgery. Ximelagatran vs low-molecular-weight heparin and warfarin for the treatment of deep vein thrombosis. Ileus following gynecologic surgery: management with water-soluble hyperosmolar radiocontrast material. Assessment of wound infiltration with bupivacaine in women undergoing day-case gynecological laparoscopy. Evidence-based interventions for post discharge nausea and vomiting: a review of the literature. Clinical validity of negative helical computed tomography for clinical suspicion of pulmonary embolism. Rational use of D-dimer measurement to exclude acute venous thromoembolic disease. Granisetron, droperidol, and metoclopramide for the treatment of established postoperative nausea and vomiting in women undergoing gynecologic surgery. Effect of hyperglycemia and continuous intravenous insulin infusions on outcomes of cardiac surgical procedures: the Portland diabetic project. Necrotizing fasciitis in gynecologic and obstetric patients: a surgical emergency. Primary mass closure of midline incisions with a continuous polyglyconate monofilament absorbable suture. Postoperative pain after laparoscopic and vaginal hysterectomy for benign gynecologic disease: a randomized trial. Patient satisfaction and postoperative demands on hospital and community services after day surgery. Supraumbilical upper abdominal midline incision for pelvic surgery in the morbidly obese patient. Screening for pulmonary embolism with a D-dimer assay: Do we still need to assess clinical probability as well Assessment of outpatient treatment of deep-vein thrombosis with low-molecular-weight heparin. Urine culture at removal of indwelling catheter after elective gynecologic surgery: Is it necessary A comparison of subcutaneous lowmolecular-weight heparin with warfarin sodium for prophylaxis against deepvein thrombosis after hip or knee implantation. Subcutaneous low-molecular-weight heparin compared with continuous intravenous heparin in the treatment of proximal-vein thrombosis. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Low molecular weight versus standard heparin for prevention of venous thromboembolism after major abdominal surgery. Role of comuted tomography and magnetic resonance imaging for deep venous thrombosis and pulmonary embolism. Awake epidural anesthesia is associated with improved natural killer cell cytotoxicity in the perioperative period. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. Decision support increases guideline adherence for prescribing postoperative nausea and vomiting prophylaxis. Prospective trial of early feeding and bowel stimulation after radical hysterectomy. Effect of an intensive glucose management protocol on the mortality of critically ill patients. Efficacy of preemptive analgesia for wound pain after laparoscopic operations in infertile women: a randomised, double-blind and placebo control study. Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Comparison of efficacy and safety of low molecular weight heparins and unfractionated heparin in initial treatment of deep venous thrombosis: a meta-analysis. Use of different D-dimer levels to exclude venous thromboembolism depending on clinical pretest probability. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. Drainage following radical hysterectomy and pelvic lymphadenectomy: dogma or need Early feeding and the incidence of gastrointestinal symptoms after major gynecologic surgery.
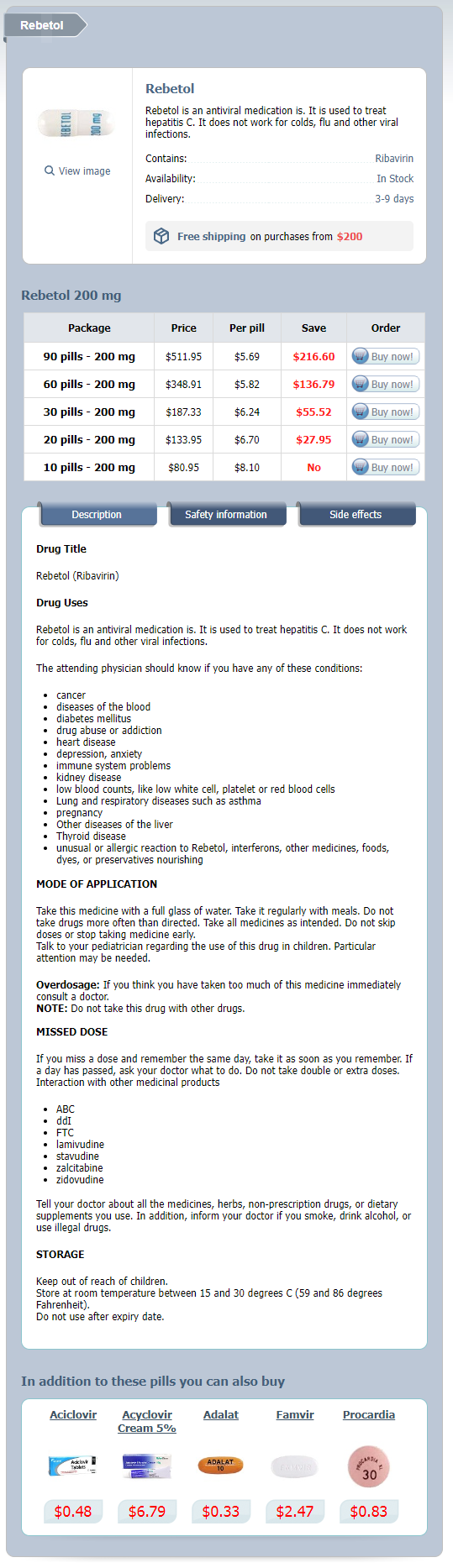
Rebetol Dosage and Price
Rebetol 200 mg
- 90 pills - $511.95
- 60 pills - $348.91
- 30 pills - $187.33
- 20 pills - $133.95
- 10 pills - $80.95
The theory suggests that this lag allowed the occult breast cancers to undergo apoptosis when later exposed to estrogen medications ending in pam cheap rebetol 200 mg, thus decreasing the risk of breast cancer (Jordan, 2015). The background risk for breast cancer in a woman between the ages of 50 and 60 is 2. Note that this applies to women who had also used hormones in the past, as noted earlier. This risk is expected to be even lower with different regimens including lower dose therapy, and potentially with different progestogens, such as natural progesterone, which has been shown in observational studies not to increase the risk. Furthermore, for estrogen alone, there is probably no increased risk at moderate to low doses for up to 20 years of exposure, as noted by Chen and colleagues. Screened cohort defined as those women starting in 1988 who reported either a screening mammogram or clinical breast examination in the previous 2 years. Accordingly, for longer-term therapy, if warranted (>5 years) lower doses of estrogen should be used, and progestogen exposure should be minimized. However, the data are inconsistent, and the purported risk is less than a twofold relative risk. The most recent meta-analysis suggested a modest risk of 30% to 40% (Collaborative Group, 2015). In this analysis it is unclear if adequate attention was paid to confounders, and there was no association with length of exposure regarding risk, which does not make sense physiologically. Further, estrogen and estrogen/progestogens both carried some risk, whereas use of oral contraceptives are known to decrease ovarian cancer risk. According to this meta-analysis, the risk was calculated to be approximately 1 extra case of ovarian cancer per 1000 women over 5 years, which suggests if this association is real, it is extremely rare. Women older than 50 should have a colorectal evaluation by some means (detection of occult blood, sigmoidoscopy, or a colonoscopy). No definitive mechanism for this protective effect has been found, although several theories have been advanced (changes in the composition of bile acids, anti-inflammatory effects, etc. As discussed previously, in a young healthy population of women close to menopause, estrogen-based therapy has been shown to significantly decrease coronary disease and mortality, with minimal to rare risks of adverse outcomes. Although some investigators have questioned the validity of this approach, risk assessment is not an unreasonable course in general, along the lines of stressing the need for prevention after menopause. Details of this approach may be found in the review cited, but in essence stresses the introduction of screening procedures for these disorders and then beginning prevention strategies such as prescribing diet and exercise regimens and the consideration of hormone therapy. Postmenopausal hormone therapy and cardiovascular disease by age and years since menopause. Hormone therapy for preventing cardiovascular disease in post-menopausal women (review). Finally, the data to date regarding protection are strongest for the use of estrogen; certain progestogens may eliminate or attenuate the benefit, and some progestogens increase the promotional risk of breast cancer. A more complete list may be found in the Consumer section of the North American Menopause Society website at For the clinician and patient, as noted earlier, the decision to start estrogen therapy need not involve a long-term commitment. For shortterm treatment of symptoms, estrogen should be used at the lowest dose that can control hot flushes or can be administered via the vaginal route for symptoms of dryness or dyspareunia. Therefore, lower doses are still recommended, which are sufficient for symptom control. Oral estrogen results in higher levels of estrone (E1) than estradiol (E2); this is true for oral micronized E2 as well as E1 products. Estrone sulfate is the major component, but the biologic activities of equilin, 17-dihydroequilin, and several other B-ring unsaturated estrogens, including 5 dehydroestrone, have been documented. Oral estrogens have a potent hepatic "first-pass" effect that results in the loss of approximately 30% of their activity with a single passage after oral administration. However, when these absolute numbers are compared with the benefit of the reduction in hot flushes in women receiving estrogen, the latter appears to be the predominant effect. For some women, the fear of breast cancer, particularly in those with Obstetrics & Gynecology Books Full 14 Menopause and Care of the Mature Woman 287 Box 14. Matrix patches are preferable to the older alcohol-based preparations because there is less skin reaction and estrogen delivery is more reliable. Whereas levels of E2 with oral therapy may vary widely among women and within the day (peaks and valleys), levels with transdermal therapy are more constant within each woman, yet values achieved may vary from woman to woman based on absorption and metabolic characteristics. Note also that many commercial assays for E2 are not reliable and do not accurately reflect estradiol status; this is particularly the case after oral estrogen therapy, because of the increase in estrogen conjugates, which interfere with many commercial assays. In women with vulvovaginal or urinary complaints, vaginal therapy is most appropriate. With creams, systemic absorption occurs but with levels that are one fourth of that achieved after similar doses administered orally. Other products (tablets and rings) are available that have been designed to limit systemic absorption. A Silastic ring is available that delivers E2 to the vagina for 3 months with only minimal systemic absorption. Estrogen may be administered continuously (daily) or for 21 to 26 days each month. If the woman has a uterus, a progestogen should be added to the regimen (see Table 14. For women who are totally intolerant of progestogens (regardless of the dose and route of administration) and take unopposed estrogen, even at lower doses, periodic endometrial sampling is necessary. The most inert progestogens, such as micronized progesterone, or vaginal delivery of progesterone should have the fewest attenuating effects.
© 2025 Adrive Pharma, All Rights Reserved..