General Information about Ramipril
It can also be necessary to watch your blood stress regularly while taking ramipril, as it might take a couple of weeks for the treatment to reach its full effect. It isn't uncommon for docs to additionally advocate lifestyle changes alongside medicine to manage hypertension, such as common train, a nutritious diet, and limiting alcohol and salt consumption.
High blood pressure, if left untreated, can result in severe well being penalties similar to coronary heart illness, stroke, and kidney failure. Therefore, it could be very important control it with the assistance of medications like ramipril.
Ramipril, sold under the model name Altace, is a medication used to treat hypertension (hypertension). It belongs to a category of medication generally identified as ACE inhibitors, and works by relaxing blood vessels and improving blood flow, which helps to decrease blood strain.
Ramipril is available in tablet form and is usually taken once a day, with or with out food. The dosage will depend upon the individual's blood pressure ranges and response to the medicine, and it might be adjusted by a physician over time.
Some common side effects that may happen while taking ramipril include dizziness, tiredness, cough, and headache. These unwanted side effects are usually gentle and should subside as the physique adjusts to the medication. However, in the occasion that they persist or turn out to be bothersome, you will need to consult a physician. Rare but more critical unwanted side effects could embrace difficulty respiration, swelling of the face, lips, tongue, or throat, and chest pain. If any of these occur, seek medical consideration immediately.
Ramipril can interact with different medicines, including over-the-counter medicine and herbal supplements. It is essential to tell your physician of all the medications you take to avoid any potential problems.
Altace ought to be taken regularly for it to be efficient in controlling blood stress. If a dose is missed, you will want to take it as quickly as remembered. However, whether it is virtually time for the following scheduled dose, do not take an extra dose to make up for the missed one.
Before beginning ramipril, it is necessary to inform your doctor of any pre-existing conditions or medications you could be taking. It is especially essential to debate any history of liver or kidney disease, diabetes, coronary heart disease, or any allergy symptoms. This will help the physician decide if ramipril is a protected and suitable medication for you.
Unlike other drugs for hypertension, ramipril not only helps to decrease blood strain, but it additionally has additional advantages. It has been proven to decrease the chance of heart assault, stroke, and demise in patients with a historical past of heart disease or those at high threat for it. This makes ramipril a useful and generally prescribed treatment for treating hypertension.
In conclusion, ramipril, bought as Altace, is a generally prescribed treatment for treating high blood pressure, nevertheless it also has extra benefits in reducing the risk of heart disease. It is important to comply with the beneficial dosage and seek the guidance of together with your doctor to make sure its effectiveness and to handle any potential unwanted facet effects. By working together with way of life adjustments, ramipril could be an efficient software in controlling blood strain and minimizing the risk of great health issues.
Progress in the design of a centrifugal cardiac assist pump with trans-cutaneous energy transmission by magnetic coupling hypertension or high blood pressure cheap 10 mg ramipril visa. Another way of pumping blood with a rotary but noncentrifugal pump for an artificial heart. Extracorporeal mechanical pulsatile pump and its significance for myocardial function recovery and circulatory support. Development of totally implantable electromechanical artificial heart systems: Baylor ventricular assist system. Baylor Gyro Pump: a completely seal-less centrifugal pump aiming for long-term circulatory support. Left ventricular assistance using a catheter-mounted coaxial flow pump (Hemopump) in a canine model of regional myocardial ischaemia. In vivo evaluation of an intraventricular electric axial flow pump for left ventricular assistance. Observations of coronary flow augmentation and balloon function during intraaortic balloon counterpulsation using transesophageal echocardiography. Left-to-right shunt reduction with intra-aortic balloon pump in postmyocardial infarction ventricular septal defect. Predictors of survival 1 hour after implantation of an intra-aortic balloon pump in cardiac surgery. Contemporary utilization and outcomes of intra-aortic balloon counterpulsation in acute myocardial infarction: the Benchmark registry. The current practice of intra-aortic balloon counterpulsation: results from the Benchmark Registry. Sheathless insertion of the percutaneous intraaortic balloon pump: an alternate method. Optimal timing of preoperative intraaortic balloon pump support in high-risk coronary patients. Estimation of timing errors for the intraaortic balloon pump use in pediatric patients. New sequential synchronized driving system of intraaortic balloon pumping and left ventricular assist device: influence on endocardial viability ratio and renal blood flow in their combination. A novel approach to pediatric intraaortic balloon pump timing using M-mode echocardiography. A novel technique for intraaortic balloon pump placement via the left axillary artery in patients awaiting cardiac transplantation. Transthoracic intraaortic counterpulsation: a simple method for balloon catheter positioning. Direct ascending aortic insertion of the "percutaneous" intraaortic balloon catheter in the open chest: advantages and precautions. Trends in intraaortic balloon counterpulsation complications and outcomes in cardiac surgery. Journal of the Medical Association of Thailand = Chotmaihet thangphaet 2002;85(Suppl. Vascular complications of the intraaortic balloon pump in patients undergoing open heart operations: 15-year experience. Vascular complications related to intraaortic balloon counterpulsation: an analysis of ten years experience. Frequency of long-term lower limb ischemia associated with intraaortic balloon pump use. Outcome and complications of prolonged intraaortic balloon counterpulsation in cardiac patients. Implications for the vascular surgeon with prolonged (3 to 89 days) intraaortic balloon pump counterpulsation. A prospective, randomized evaluation of prophylactic intraaortic balloon counterpulsation in high risk patients with acute myocardial infarction treated with primary angioplasty. Cardiogenic shock complicating acute myocardial infarction: the use of coronary angioplasty and the integration of the new support devices into patient management. Prolonged intraaortic balloon support for septal rupture after myocardial infarction. Results of surgery for irreversible moderate to severe mitral valve regurgitation secondary to myocardial infarction. Cardiovascular outcomes using intra-aortic balloon pump in high-risk acute myocardial infarction with or without cardiogenic shock: a meta-analysis. Intra-aortic balloon pump therapy for acute myocardial infarction: a meta-analysis. Analysis of the outcome for patients experiencing myocardial infarction and cardiopulmonary resuscitation refractory to conventional therapies necessitating extracorporeal life support rescue. The use of extracorporeal life support in adult patients with primary cardiac failure as a bridge to implantable left ventricular assist device. Roller pump induced tubing wear of polyvinylchloride and silicone rubber tubing: phase contrast and scanning electron microscopic studies. A compact, low hemolysis, non-thrombogenic system for non-thoracotomy prolonged left ventricular bypass. Roller and centrifugal pumps compared in vitro with regard to haemolysis, granulocyte and complement activation.
In the neonatal presentation of aortic coarctation blood pressure instruments order ramipril overnight, a normal circulation is maintained until ductal tissue contracts, at which point distal aortic flow is severely reduced, leading to a clinical presentation of heart failure or shock and characteristic loss of lower limb pulses. Following initial resuscitation, urinary output and resolution of metabolic acidosis are early indicators of successful reperfusion of the distal aorta. Beyond the early neonatal period, aortic coarctation presents as progressive onset of cardiac failure or as an incidental finding (murmur, upper limb hypertension, absent weak femoral pulses) later in childhood. Thoracic aortic collaterals develop and may be noted as rib notching on a plain chest x-ray. The tunnel form may be suitable for resection or require a more extensive Konno or Ross-Konnotype procedure. Balloon angioplasty with or without endovascular stent placement is frequently used to alleviate recurrent aortic coarctation and is increasingly being used with apparent success, to address native coarctation particularly in older patients but is not favored in symptomatic neonates. Specific postoperative problems include systemichypertension, which is thought to be due to multiple factors including altered baroceptor and adrenal catecholamine and renin-angiotensin axes. Some children have persistent hypertension following repair178 and require long-term antihypertensive therapy. Postcoarctectomysyndrome179 occurs in older patients and is thought to be the result of restoration of higher pressure pulsatile flow to the mesenteric arterial tree and presents as abdominal distention, abdominal pain, ascites, or occasionally, enteric infarction. The condition is best managed by avoiding enteral feeding for 24 hours following repair and aggressive treatment of systemic hypertension. The necessity of aortic clamping during surgical repair interrupts distal aortic flow and may result in spinal cord ischemia (rare in neonates, 0. Intensivists must seek positive confirmation of lower limb movement and adequate renal function in the early postoperative period. In neonates low cardiac output may persist due to preexisting ventricular dysfunction, although residual coarctation should be excluded. Structures near the aortic arch prone to surgical injury include the thoracic duct, recurrent laryngeal nerve, and phrenic nerve, leading to postoperative chylothorax, stridor, or hemidiaphragm paralysis. In this condition, the aortic arch is either atretic or interrupted, creating either complete disruption or luminal obstruction (without external interruption). It is classified according to the location of the interruption along the aortic arch, which may be distal to the left subclavian artery (type A), between the left common carotid and left subclavian arteries (type B), or between the brachiocephalic trunk and left common carotid arteries (type C). The more common form of interrupted aortic arch, type B, is associated with the 22q11 chromosomal deletion152,153 (see above). Interrupted aortic arch can be regarded as a severe form of aortic coarctation, with duct-dependent distal aortic perfusion, and requires similar initial management. There is a risk of transfusion-associated graft-versus-host disease and hypocalcemia in children with type B interrupted aortic arch associated with 22q11 deletion and Di George phenotype. Coronary artery abnormalities may also be present, and a right-sided aortic arch is seen in approximately 20% of cases. However, some centers adopt a two-stage approach with initial placement of a modified systemic-to-pulmonary arterial (Blalock-Taussig) shunt to secure pulmonary blood flow in cyanotic neonates with complete repair being undertaken after a few months. Preoperatively, there is complete mixing of systemic and pulmonary venous return in a duct-dependent circulation. Some blood may pass via coronary sinusoids, if present, or back through a regurgitant tricuspid valve. Fetal cardiac valvoulplasty may have a role in the management of this condition in the future. These include low cardiac output due to excessive runoff through the shunt, myocardial ischemia due to decompressed coronary fistulae, or low systemic diastolic pressure due to excessive shunt runoff. If the diagnosis is suspected in a neonate, an infusion of prostaglandin E1 or E2 should be established to maintain ductal patency, and following echocardiographic confirmation of the diagnosis, a balloon atrial septostomy is sometimes necessary to enlarge the foramen ovale and secure mixing at the atrial level, particularly if the foramen ovale is restrictive, leading to high pulmonary venous pressures. Saturations typically increase from very low levels (<50%) to 65%-85% following these interventions, and it is then usually possible to discontinue the prostaglandin infusion. The preferred surgical option in the current era is the arterial switch (Jatene) operation,195-198 although long-term results following Senning operations also appear to be acceptable. Left ventricular dysfunction is common in babies during the first 12 hours following the arterial switch operation. Preload should be augmented gradually, titrating volume infused against measured left atrial pressure. Atrial switch procedures are usually performed outside the neonatal age group and, compared to arterial switch patients, have a relatively uneventful postoperative course. Complex Single-Ventricle Circulations Some defects are such that they can never be corrected to provide two functioning ventricles. Children with this type of anatomy will always have two ventricles, even if one is hypoplastic, but physiologically they behave as if the heart consists of only a single ventricle. Complex single-ventricle hearts can be palliated with a series of interventions leading to creation of a Fontan circulation in which the systemic and pulmonary circulations are completely separated. Systemic and pulmonary blood flow is assured at the expense of mixing of pulmonary and systemic venous returns, with consequent cyanosis and volume loading of the single ventricle. Subsequently, if hemodynamic conditions are favorable, the Fontan circulation is established, usually in two-staged procedures. This has the benefit of reducing the volume load placed on the systemic ventricle by previously placed systemic-pulmonary shunt. In the Fontan circulation, there is no "subpulmonary" ventricle, all ventricular tissue having been incorporated in the single ventricle that receives pulmonary venous return and ejects into the systemic circulation. This establishes a form of series circulation and results in normal systemic oxygenation and equality of pulmonary and systemic blood flow. Long-term follow-up studies have demonstrated that systemic ventricular function remains abnormal after Fontan procedures. Balancing the pulmonary and systemic circulations in the immediate postoperative period can be challenging.
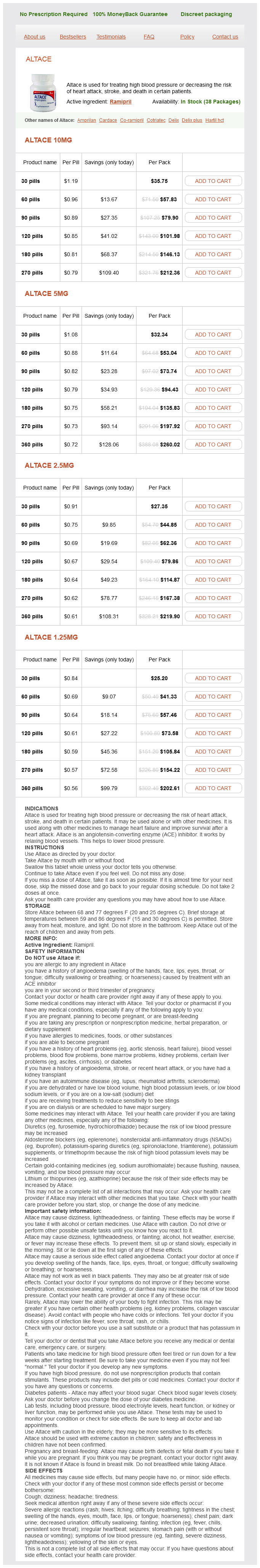
Ramipril Dosage and Price
Altace 10mg
- 30 pills - $35.75
- 60 pills - $57.83
- 90 pills - $79.90
- 120 pills - $101.98
- 180 pills - $146.13
- 270 pills - $212.36
Altace 5mg
- 30 pills - $32.34
- 60 pills - $53.04
- 90 pills - $73.74
- 120 pills - $94.43
- 180 pills - $135.83
- 270 pills - $197.92
- 360 pills - $260.02
Altace 2.5mg
- 30 pills - $27.35
- 60 pills - $44.85
- 90 pills - $62.36
- 120 pills - $79.86
- 180 pills - $114.87
- 270 pills - $167.38
- 360 pills - $219.90
Altace 1.25mg
- 30 pills - $25.20
- 60 pills - $41.33
- 90 pills - $57.46
- 120 pills - $73.58
- 180 pills - $105.84
- 270 pills - $154.22
- 360 pills - $202.61
Patients with borderline high levels of serum K+ can develop life-threatening hyperkalemia with the development of acidosis blood pressure medication ptsd buy ramipril mastercard. Such measures include the use of bicarbonate to correct acidemia, -agonist therapy, and glucose/insulin administration. The majority is in the bone, and in the absence of parathyroid hormone, there is reduced calcium reabsorption from bone and increased urinary secretion because of the decreased renal production of calcitriol. Forty percent of the calcium is protein bound, and the most common cause of a low total calcium in critically ill children is hypoalbuminemia. Hypocalcemia is seen in neonates with birth asphyxia, preterm infants, term newborns in the first week of life, and infants of diabetic mothers. This finding is invariable in newborn infants with DiGeorge syndrome, where it is seen in association with conotruncal congenital heart defects, typically truncus arteriosus and an interrupted aortic arch. The majority of these infants have microdeletions of the long arm of chromosome 22 (22q minus syndrome) and immunodeficiency. Hypocalcemia is a common finding in critically ill older children, with a reported incidence of 49% in one study. Hyperphosphatemia, seen in tumor lysis syndrome and renal failure, can also result in hypocalcemia. Hypercalcemia in critically ill children is usually the result of excessive calcium administration frequently in association with diuretic administration. Common causes of the latter include cellular breakdown or injury in tumor lysis syndrome, rhabdomyolysis, burns, and trauma. A large randomized controlled double-blind trial comparing isotonic fluid (Plasma-Lyte 148) with 0. This study provides further evidence in support of the use of isotonic rather than hypotonic solutions in pediatric practice. Acute hyponatremia related to intravenous fluid administration in hospitalized children: an observational study. Patients who developed hyponatremia had twice the amount of electrolyte-free water administered compared to controls. This study was designed to show that isotonic saline was a safe solution for pediatric use in terms of the development of hypernatremia. A randomized controlled trial of the use of hypotonic versus isotonic saline for fluid replacement in gastroenteritis. The use of isotonic saline resulted in a reduced incidence of hyponatremia without the development of hypernatremia. Hospital-acquired hyponatremia in postoperative pediatric patients: prospective observational study. Thirty-one percent of children had a plasma sodium concentration less than 135 mmol/L at 24 hours postop. A prospective randomized trial of isotonic versus hypotonic saline in a postsurgical pediatric population. The use of hypotonic saline was associated with an increased risk of developing hyponatremia. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. This study addressed the question of whether the risk of hyponatremia could be reduced by using hypotonic fluids in lower amounts rather than isotonic fluids at recommended maintenance levels. The incidence of hyponatremia was decreased by the use of isotonic saline but not by the combination of hypotonic saline and fluid restriction. Postnatal control of water and electrolyte homeostasis in pre-term and full-term infants. Arginine vasopressin and renin in acutely ill children: implication for fluid therapy. Hyponatraemic seizures and excessive intake of hypotonic fluids in young children. Incidence of hyponatraemia and hyponatraemic seizures in severe respiratory syncytial virus bronchiolitis. The syndrome of inappropriate secretion of antidiuretic hormone in children with bacterial meningitis. Hyponatremic natriuretic syndrome in tuberculous meningitis: the probable role of atrial natriuretic peptide. Isotonic is better than hypotonic saline for intravenous rehydration of children with gastroenteritis: a prospective randomised study. Hyponatremia in children with bronchiolitis admitted to the pediatric intensive care unit is associated with worse outcomes. Management of meningitis in children with oral fluid restriction or intravenous fluid at maintenance volumes: a randomised trial. Postoperative hyponatraemic encephalopathy following elective surgery in children. Severe hyponatremic encephalopathy after pediatric surgery: report of seven cases and recommendations for management and prevention. Pathogenesis of postoperative hyponatraemia following correction of scoliosis in children. Inappropriate secretion of antidiuretic hormone in postoperative scoliosis patients: the role of fluid management.
© 2025 Adrive Pharma, All Rights Reserved..