General Information about Proventil
One of the significant advantages of Proventil is its security profile. It is generally well-tolerated and has a decrease incidence of unwanted effects when compared to different medications used to deal with bronchospasm. However, as with every treatment, some gentle unwanted aspect effects might occur in some people, together with trembling, nervousness, headache, and elevated coronary heart fee. These unwanted side effects are usually momentary and may subside after a number of doses. However, if they persist or turn out to be worse, it is important to consult a healthcare professional.
In conclusion, Proventil is an efficient and safe treatment for the treatment and prevention of bronchospasm in people with reversible obstructive airway disease. Its fast-acting nature and minimal side effects make it a preferred alternative among patients and healthcare suppliers. However, it is essential to use this medication as prescribed and seek medical recommendation if any considerations arise. With proper use and monitoring, Proventil can provide aid and enhance the quality of life for people with bronchospasm.
Proventil may additionally be used as a preventative measure for people who expertise exercise-induced bronchospasm (EIB). This condition is common among athletes and individuals who engage in physical activities. By using Proventil before exercising, it can help forestall bronchospasm and improve general performance. It is crucial to follow the beneficial dosage and instructions when utilizing Proventil for EIB to avoid any potential unwanted effects.
One of the major advantages of Proventil is its rapid onset of action. It begins working within minutes after using it and offers aid from bronchospasm for as much as 4 to six hours. This makes it an excellent medicine for people who expertise sudden flare-ups of breathing difficulties.
Bronchospasm is a condition where the muscles across the airways tighten, inflicting the airways to become narrower and making it tough to breathe. This may be attributable to various elements similar to allergic reactions, bronchial asthma, and persistent obstructive pulmonary disease (COPD). Proventil offers relief by stress-free these muscular tissues, permitting the airways to open up and improve respiratory.
Proventil is a model name for the generic drug albuterol. It falls under the category of medicines known as short-acting beta-agonists (SABAs). It is out there within the type of an inhaler, which delivers the medicine directly to the lungs for faster reduction.
Proventil shouldn't be used as a long-term remedy for persistent conditions similar to asthma and COPD. It is primarily intended to offer quick aid during sudden episodes of bronchospasm. For long-term management of these situations, your doctor may recommend other drugs.
Individuals with a historical past of heart issues, hypertension, diabetes, and thyroid problems ought to consult their healthcare provider before using Proventil. It can be important to inform your doctor of any other medicines or supplements you may be presently taking to avoid potential drug interactions.
Proventil is a well-liked medication used to treat or forestall bronchospasm in individuals who've reversible obstructive airway illness. This medicine is a quick-relief inhaler that works by opening up the air passages within the lungs, making it simpler to breathe.
Brainstem auditory evoked potential studies in Gunn rats indicate functional abnormalities of the central auditory pathways at and rostral to the cochlear nuclei beginning at 17 days of age asthmatic bronchitis quizlet buy cheap proventil on-line. Sulfonamides displace bilirubin from albumin binding, thereby promoting the net transfer of bilirubin into neural tissues. Administration of sulfonamides results in reversible abnormalities of brainstem auditory evoked potentials in Gunn rats. A large number of Purkinje cells are affected in the cerebellum of Gunn rats at the age of 7 days; most of these cells degenerate and disappear between day 12 and day 30, resulting in cerebellar hypoplasia. However, synapse formation among these Purkinje cells or with other neural cells may remain abnormal. Photooxidation and Degradation In the presence of light and oxygen, bilirubin undergoes a selfsensitized reaction involving singlet oxygen, resulting in the formation of colorless fragments, chiefly maleimides and propentdyopent adducts. Bilirubin Toxicity the cerebral toxicity of bilirubin in neonatal jaundice has been known for at least 5 centuries. Degeneration of brain tissues associated with yellow pigmentation was reported in 1949. Bilirubin encephalopathy may present with a broad spectrum of neurologic features. In the severest cases, overt kernicterus presents between the third and sixth days of life. The normal Moro reflex is lost, the muscles become hypotonic, the cry is high-pitched, athetoid movements appear, and reflex opisthotonos occurs in response to a startling stimulus. Occasionally, in some children with Crigler-Najjar syndrome type 1, bilirubin encephalopathy may present late with cerebellar symptoms as the presenting feature. Cells of the auditory system that receive synaptic input from end-bulbs or calyces appear to be early targets. The sensitivity of auditory evoked potential testing can be increased by the recording of binaural difference waves obtained by subtraction of the sum of two monaural brainstem auditory evoked potentials from a binaural brainstem auditory evoked potential. Clinical manifestations precede histologic evidence of brain damage by approximately 72 hours. Nonspecific signs of encephalopathy in the neonate may result from other causes, such as cerebral hemorrhage,70 and therefore kernicterus cannot always be diagnosed without pathologic documentation. Conversely, focal bilirubin staining of the brain may occur in other forms of brain injury. Thus, in the absence of neuronal degeneration, bilirubin staining alone does not establish the diagnosis of classic kernicterus. The prognostic significance of a moderate degree of hyperbilirubinemia is not entirely clear. Serum bilirubin levels that are not high enough to cause kernicterus have been reported to result in an increased incidence of neurologic abnormalities or decreased intellectual performance later in life. Conventionally, immaturity of the blood-brain barrier in neonates has been implicated in the high incidence of kernicterus in this age group. However, it has been difficult to confirm a more rapid passage of labeled markers74 or lipophilic substances75 into the immature brain. Therefore there is no firm evidence to support the concept of an immature blood-brain barrier in the neonate. The efficiency of cerebral bilirubin clearance may be inversely related to the cerebral toxicity of bilirubin. Experimentally, the blood-brain barrier can be unilaterally and reversibly opened without causing brain damage by infusion of hypertonic urea76 or arabinose. When the blood-brain barrier is opened in newborn rats by this technique, intravenously administered albumin-bound bilirubin rapidly enters the brain. Following the reversal of the blood-brain barrier, bilirubin is rapidly cleared from the brain. The clearance of bilirubin from brain parallels its clearance from plasma, suggesting that bilirubin is cleared by diffusion or active transport back into the general circulation. According to these concepts the blood-brain barrier is not merely a passive anatomic structure but is an active tissue that can pump bilirubin and other metabolites and drugs out of the brain, thus reducing their intracellular concentrations. Substrate competition at the level of these pumps may be another way by which drug exposure can modulate bilirubin brain toxicity. Biochemical Basis of Bilirubin Toxicity In cell culture systems, bilirubin shows a very broad range of toxicity. It is not clear which of the toxic effects observed in monotype cell cultures are relevant in bilirubin encephalopathy, and results observed with cultured cells do not always mirror findings in vivo. Thus a variety of protective mechanisms fail to protect the Blood-Brain Barrier and Cerebral Bilirubin Clearance the equilibration of hydrophilic water-soluble substances and proteins between the blood and the brain is restricted by a functional blood-brain barrier. Clinical Consequences Risk of bilirubin toxicity increases when albumin levels are low. Excess extracellular glutamate causes excitotoxicity, further increasing intracellular Ca2+ levels, thereby activating enzymes that cause cell death. Activation of the intracellular inflammatory cascade causes apoptosis and necrosis of astrocytes and neurons. Oligodendrocytes Oligodendrocytes support brain neurons by providing myelination of axons. Physiologic mechanisms of protection against bilirubininduced injury and cellular mechanisms of bilirubin toxicity are summarized in Table 58-1. In the hepatic sinusoids the albumin-bilirubin complex dissociates and bilirubin is internalized by facilitated diffusion. Conjugated bilirubin exits from the endoplasmic reticulum and is eventually transported across the bile canalicular membrane into the bile by an energy-consuming process that is rate limiting in bilirubin Bilirubin Nephrotoxicity Renal medullary deposition of unconjugated bilirubin results in medullary necrosis and formation of bilirubin crystals on the renal papillae85 in Gunn rats and in hyperbilirubinemic infants.
Mutation identification will very likely become the diagnostic aid of choice when clinical and biochemical features arouse suspicion of Wilson disease symptoms asthma attack 3 year old proventil 100 mcg purchase mastercard. The most common mutation, H1069Q, is present as at least one of the two mutations in 35% to 75% of affected patients of European origin, particularly those from eastern Europe. One of the exceptions is the island of Sardinia, where most patients have a 15-bp deletion in the promoter region. Missense mutations tend to lie predominantly within functional domains but their functional effects are difficult to predict. When only one mutation is used to support the diagnosis, that one mutation must be definitely established as disease causing. Prediction of disruption of the molecule, conservation of the specific residue between species, and absence in at least 50 controls are among the features examined in attempts to identify which mutations are causing disease. Data from a number of laboratories indicate that there is not a high correlation between specifics of clinical disease (phenotype) and a specific mutation (genotype). Monozygotic twins with different clinical forms of Wilson disease have been reported. Because Wilson disease is a recessive condition, brothers and sisters of a patient have a 25% chance of also being affected and a 50% risk of being heterozygotes. However, all first-degree relatives should be screened for Wilson disease because the carrier rate may be higher than supposed. However, initiation of treatment before tissue damage occurs offers the best outlook for a normal span and quality of life. Because of the variability of biochemical tests, diagnosis in the presymptomatic stage can be difficult. When this approach is used, the flanking markers must be appropriate and informative on both sides of the gene to avoid possible error because of a recombination event. Many single nucleotide polymorphisms have been identified throughout the genome, and these can also be used for marker analysis. When first-degree relative diagnosis by haplotype is performed without mutation analysis, the initial patient must have an unequivocal diagnosis of Wilson disease. This assumption may no longer hold, but the mechanistically similar disorders recently described differ substantially from Wilson disease in their clinical features. In the absence of marker analysis or until the results of marker analysis are available, screening should include physical examination, liver function tests, serum copper and ceruloplasmin measurement, 24-hour urinary copper measurement, and a careful slit-lamp examination of the eyes. Children aged 6 years or younger who appear to be unaffected should be rechecked yearly in the next 5 to 10 years. Confirmation of the genotype is highly recommended before treatment is initiated because a heterozygote should not unnecessarily be consigned to lifelong treatment with the inherent risk of adverse side effects. Reassessment of heterozygotes for hepatic copper accumulation at approximately 50 years of age may have merit. Surveillance should include liver function tests, serum copper and ceruloplasmin measurements, measurement of basal 24-hour urinary copper excretion, and a liver sonogram. If total body copper overload is detected, treatment with zinc might be considered, although no clinical studies are currently available to determine whether treatment is ever warranted. Heterozygotes should be counseled to maintain good liver health by avoiding abdominal obesity and excessive use of alcohol. Diagnosis by Population Screening Mass screening of infants or very young children is an emerging diagnostic intervention related to Wilson disease. It potentially avoids the difficulties associated with confirming the diagnosis of Wilson disease in patients who have atypical clinical findings. Current experience suggests that molecular mass screening is not cost-effective for general populations because of the high allelic heterogeneity existing in Wilson disease; however, it is feasible and of benefit in isolated populations with a high degree of consanguinity. Genetic Differential Diagnosis A few genetic disorders even rarer than Wilson disease may be regarded as candidate mimics of Wilson disease. The serum ceruloplasmin level is very low, and basal 24-hour urinary copper excretion is elevated; hepatic parenchymal copper concentration may be increased, with evidence of chronic liver damage. The genetic basis of a hepatic copper toxicosis, described from southern India, which resembles both Indian childhood cirrhosis and Wilson disease has not been determined. From extensive clinical experience with long-term chelator treatment, it is evident that most patients live normal, healthy lives with effective treatment. There are two generally accepted orally administered chelating agents: D-penicillamine and trientine. The potent chelator tetrathiomolybdate is relatively new and remains an experimental treatment modality. Zinc interferes with copper uptake from the intestinal contents and stabilizes hepatic copper by inducing metallothioneins. The outcome is best for patients who begin treatment when their disease is diagnosed before the onset of symptoms (presymptomatic). The role of adjunctive treatments such as antioxidants has not been formally established, and the potential utility of gene transfer therapy is currently undetermined. Penicillamine is the sulfhydryl-containing amino acid cysteine with two methyl group substituents (,dimethylcysteine). It can be administered orally and is rapidly absorbed, with bioavailability on the order of 50%. Studies in the Long-Evans cinnamon rat model of Wilson disease indicate that penicillamine inhibits the accumulation of copper in hepatocellular lysosomes and, once accumulated, solubilizes copper for mobilization from these particles but not from cytoplasmic metallothionein. Urinary copper excretion in 24 hours generally reflects the total body copper load and can be used to monitor zinc treatment, even though zinc does not cause cupruresis; alternatively, an estimated serum nonceruloplasmin-bound copper level of less than 150 µg/L can be used. In addition to its chelating action, D-penicillamine inhibits collagen cross-linking and acts as an immunosuppressant. Some side effects are minor (loss of taste, gastrointestinal upset, and arthralgias), whereas others are severe (proteinuria, leukopenia, and thrombocytopenia).
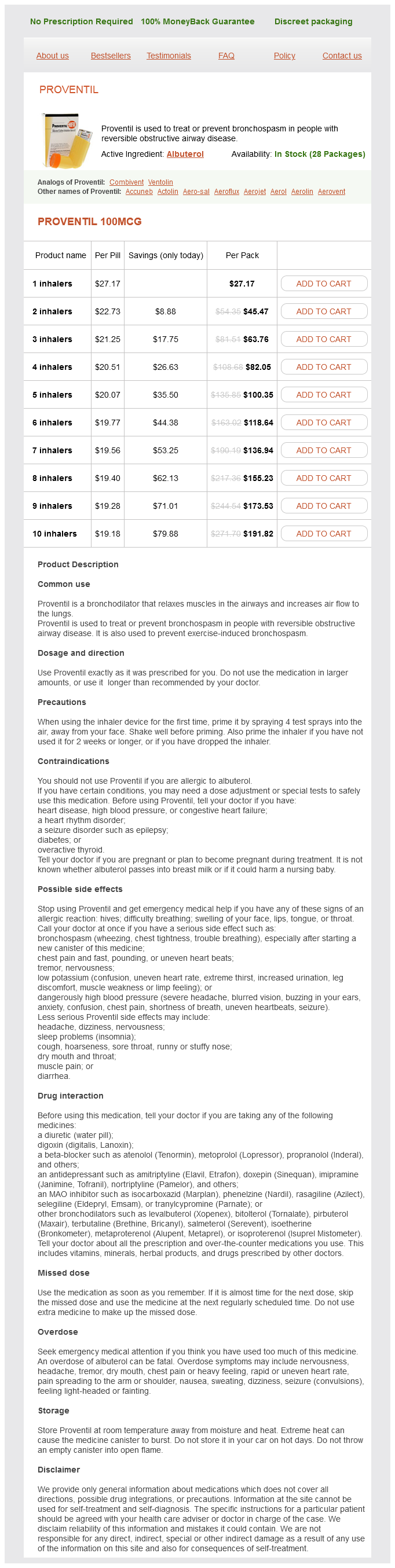
Proventil Dosage and Price
Proventil 100mcg
- 1 inhalers - $27.17
- 2 inhalers - $45.47
- 3 inhalers - $63.76
- 4 inhalers - $82.05
- 5 inhalers - $100.35
- 6 inhalers - $118.64
- 7 inhalers - $136.94
- 8 inhalers - $155.23
- 9 inhalers - $173.53
- 10 inhalers - $191.82
Many medications have proved disappointing despite preliminary promising data asthmatic bronchitis curable 100 mcg proventil buy with visa, and others are still under active investigation. Phlebotomy Dysmetabolic iron overload syndrome refers to hyperferritinemia and hepatic iron deposition commonly seen in fatty liver disease. Unfortunately, outside several animal trials and one human pilot trial, the results have been disappointing. These long-term studies are a minimum of 1 year in length, with many including 5-year end points to effectively determine if they produce an improvement in outcomes without significant side effects. Cytoprotective Agents Medications designed to prevent apoptosis and down-regulate the inflammatory cascade have also been investigated, with mixed results. Caffeinated drip coffee is likely beneficial in a dosage of two to three cups daily. Vitamin E in nondiabetic patients can be considered as can pioglitazone in diabetic patients without cardiovascular disease. Pilot trials using inhibitors of 3-hydroxy-3methylglutaryl-coenzyme A reductase, or statins, have demonstrated modest histologic benefit, with larger studies using serum aminotransferases as an imperfect surrogate. National Institutes of Health, National Heart, Lung, and Blood Institute: Risk factor clustering and the metabolic syndrome. Targher G, et al: Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease in type 2 diabetic patients. Kwok R, et al: Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Prashanth M, et al: Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. Machado M, et al: Hepatic histology in obese patients undergoing bariatric surgery. Kasapoqlu B, et al: Low vitamin D levels are associated with increased risk for fatty liver disease among non-obese adults. Rochon C, et al: Response of glucose disposal to hyperinsulinemia in human hypothyroidism and hyperthyroidism. Vilar-Gomez E, et al: Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Dudekula A, et al: Weight loss in nonalcoholic fatty liver disease patients in an ambulatory care setting is largely unsuccessful but correlates to the frequency of clinic visits. Kirk E, et al: Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Haufe S, et al: Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects. Fraser A, et al: A modified Mediterranean diet is associated with the greatest reduction in alanine aminotransferase levels in obese type 2 diabetes patients: results of a quasi-randomized controlled trial. Basaranoglu M, et al: Fructose as a key player in the development of fatty liver disease. Chung M, et al: Fructose, high-fructose corn syrup, sucrose, and non-alcoholic fatty liver disease or indexes of liver health: a systematic review and meta-analysis. Bravi F, et al: Coffee reduces risk for hepatocellular carcinoma: an updated meta-analysis. Fukushima Y, et al: Effects of coffee on inflammatory cytokine gene expression in mice fed high-fat diets. Vitaglione P, et al: Coffee reduces liver damage in a rat model of steatohepatitis: the underlying mechanisms and the role of polyphenols and melanoidins. Yamashita K, et al: Association of coffee consumption with serum adiponectin, leptin, inflammation and metabolic markers in Japanese workers: a cross-sectional study. Eckard C, et al: Prospective histopathologic evaluation of lifestyle modification in nonalcoholic fatty liver disease: a randomized trial. Hallsworth K, et al: Resistance exercise reduced liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Lassailly G, et al: Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Chalasani N, et al: the diagnosis and management of nonalcoholic fatty liver disease: practice guidelines by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and the American College of Gastroenterology. Valenti L, et al: Venesection for non-alcoholic fatty liver disease unresponsive to lifestyle counseling-a propensity score-adjusted observational study. Li Y, et al: Metformin in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Shyangdan D, Clar C, Ghouri N: Insulin sensitisers in the treatment of non-alcoholic fatty liver disease: a systematic review. Belfort R, et al: A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. Musso G, et al: A meta-analysis of randomized trials for the treatment of nonalcoholic fatty liver disease. Miyazaki M, et al: Increased hepatic expression of dipeptidyl peptidase-4 in non-alcoholic fatty liver disease and its association with insulin resistance and glucose metabolism. Xiang Z, et al: the role of ursodeoxycholic acid in non-alcoholic steatohepatitis: a systematic review. Du J, et al: Effects of pentoxyfylline on nonalcoholic fatty liver disease: a meta-analysis.
© 2025 Adrive Pharma, All Rights Reserved..