General Information about Penegra
It is necessary to notice that Penegra isn't appropriate for everybody. It should not be taken by individuals with a historical past of coronary heart disease, stroke, low blood pressure, liver or kidney illness, and those taking sure drugs corresponding to nitrates, alpha-blockers, or some HIV medications.
Penegra works by rising the blood flow to the penis, which helps in achieving and sustaining an erection. It inhibits the enzyme phosphodiesterase sort 5 (PDE5), which is liable for the breakdown of cGMP (cyclic guanosine monophosphate), a chemical messenger that helps in enjoyable the sleek muscular tissues of the penis. This leads to increased blood move, allowing the penis to turn out to be erect when sexually stimulated.
Like any other treatment, Penegra may cause some unwanted effects. The most commonly reported unwanted facet effects embody headache, facial flushing, nasal congestion, indigestion, and dizziness. These unwanted effects are normally delicate and subside with continued use. However, in uncommon cases, more severe unwanted facet effects corresponding to priapism (a prolonged and painful erection) and sudden loss of imaginative and prescient or listening to could occur. If any of those serious side effects occur, medical attention ought to be sought instantly.
One of the principle benefits of Penegra is its affordability. As it's a generic model of Viagra, it is significantly cheaper than the branded version, making it accessible to a bigger inhabitants. This does not imply that the standard or effectiveness of Penegra is inferior in any way. It is manufactured by Zydus Cadila, a reputable pharmaceutical firm that adheres to strict high quality control measures to ensure the safety and efficacy of its products.
Erectile dysfunction is a condition the place a person is unable to achieve or preserve an erection adequate for sexual activity. It is a common downside that affects tens of millions of men worldwide and may be brought on by numerous components corresponding to stress, anxiety, physical and psychological well being issues, and lifestyle decisions.
Penegra is a extensively known and trusted model within the field of erectile dysfunction medication. It is an oral remedy that accommodates Sildenafil Citrate, the same energetic ingredient present in its branded model, Viagra. Penegra is a cheap and environment friendly treatment for people affected by impotence, also called erectile dysfunction (ED).
The efficacy and safety of Penegra have been tested and confirmed in quite a few scientific trials. It has proven to be effective in males of all ages, including these with diabetes, hypertension, and other well being conditions. Penegra supplies a dependable and long-lasting resolution for men affected by ED, permitting them to get pleasure from a satisfying and fulfilling sex life.
In conclusion, Penegra is an effective and affordable remedy for erectile dysfunction. It has helped countless males regain their confidence and lead a extra satisfying intercourse life. However, like any medicine, it is essential to seek the guidance of a doctor earlier than taking it, discuss any medical conditions, and disclose any drugs being taken to avoid any potential interactions. With proper use and medical steerage, Penegra could be a game-changer for men fighting ED.
Penegra is available in tablet type, with the standard dosage being 50mg. However, the dosage may be adjusted based on the person's needs and response to the treatment. It is beneficial to take Penegra about an hour earlier than sexual exercise, and its results can last as lengthy as 4 hours. It just isn't an aphrodisiac and requires sexual stimulation to work.
Calcitonin was discovered in 1961 prostate hypertrophy order 100 mg penegra, demonstrating that the thyroid gland produced a second hormone. As a result, the ratio of [I-]thyroid to [I-]plasma is usually between 20 and 50 and can exceed 100 when the gland is stimulated. Iodide transport is inhibited by a number of ions, such as thiocyanate and perchlorate. Oxidation and Iodination Transport of iodine from the thyroid follicular cell to the colloid is facilitated by the apical transporter pendrin. Uptake of Iodide Iodine ingested in the diet reaches the circulation in the form of iodide ion (I-). The thyroid actively transports the ion via Because T4 and T3 are synthesized and stored within thyroglobulin, proteolysis is an important part of the secretory process. This process is initiated by endocytosis of colloid from the follicular lumen at the apical surface of the cell, with the participation of a thyroglobulin receptor, megalin. This "ingested" thyroglobulin appears as intracellular colloid droplets, which apparently fuse with lysosomes containing the requisite proteolytic enzymes. The normal daily production of T4 is estimated to range between 80 and 100 g; that of T3 is between 30 and 40 g. Although T3 is secreted by the thyroid, metabolism of T4 by 5, or outer ring, deiodination in the peripheral tissues accounts for about 80% of circulating T3 (Gereben et al. Under normal conditions, about 40% of T4 is converted to each of T3 and rT3, and about 20% is metabolized via other pathways, such as glucuronidation in the liver and excretion in the bile. It is upregulated in hyperthyroidism, downregulated in hypothyroidism, and inhibited by the antithyroid drug propylthiouracil. D2 localizes to the endoplasmic reticulum, which facilitates access of D2-generated T3 to the nucleus. This results in suppressed levels of D2 in hyperthyroidism and elevated levels in hypothyroidism, thus helping to maintain T3 homeostasis. D3 catalyzes inner ring or 5-deiodination, the main inactivating pathway of T3 metabolism; D1 performs this function to some extent. D3 can be induced locally by inflammation and hypoxia and is highly expressed in certain tumors. Both D2 and D3 are expressed during development in time- and spatially-restricted patterns. The three deiodinases contain the rare amino acid selenocysteine in their active sites. Incorporation of selenocysteine into the growing peptide chain is a complex process involving multiple proteins. Transport of Thyroid Hormones in the Blood Iodine in the circulation is normally present in several forms, with 95% as organic iodine and about 5% as iodide. Most (90%95%) organic iodine is T4; T3 represents a relatively minor fraction (~5%). The thyroid hormones are transported in the blood in strong but noncovalent association with several plasma proteins. It is a glycoprotein (mass of ~ 63,000 Da) that binds one molecule of T4 per molecule of protein with a very high affinity (Kd, is ~ 1010 M); T3 is bound less avidly. T4, but not T3, also is bound by transthyretin (thyroxine-binding prealbumin), a retinol-binding protein. Albumin also can bind T4 when the more avid carriers are saturated, but its physiological importance is unclear. Binding of thyroid hormones to plasma proteins protects the hormones from metabolism and excretion, resulting in their long half-lives in the circulation. The differential binding affinities for serum proteins also contribute to establishing the 10- to 100-fold differences in circulating hormone concentrations and half-lives of T4 and T3. Brain Pituitary Heart Brown fat Skeletal muscle Thyroid Essential to understanding the regulation of thyroid function is the "free hormone" concept: Only the unbound hormone has metabolic activity. Because of the high degree of binding of thyroid hormones to plasma proteins, changes in either the concentrations of these proteins or the affinities of the hormone-protein interactions have major effects on the total serum hormone levels. Certain drugs and a variety of pathological and physiological conditions can alter both the binding of thyroid hormones to plasma proteins and the amounts of these proteins (Table 431). In hyperthyroidism, the t1/2 is shortened to 34 days, whereas in hypothyroidism it may be 910 days. The opposite effect is observed when binding to protein is inhibited by certain drugs (see Table 431). The liver is the major site of nondeiodinative degradation of thyroid hormones; T4 and T3 are conjugated with glucuronic and sulfuric acids and excreted in the bile. Some thyroid hormone is liberated by hydrolysis of the conjugates in the intestine and reabsorbed. Factors Regulating Thyroid Hormone Secretion Thyrotropin is a glycoprotein hormone that consists of an subunit, common to pituitary glycoproteins such as gonadotropins, and a unique subunit. Low levels of I- are required for T4 synthesis, but high levels inhibit T4 synthesis and release. In some areas of the world, simple or nontoxic goiter is prevalent because of insufficient dietary iodine. The addition of iodate to table salt (NaCl) provides a convenient iodine supplement. The recommended daily allowances for iodine range from 90 to 120 g for children, 150 g for adults, 220 g for pregnancy, and 290 g for lactation (Public Health Committee of the American Thyroid Association et al. Vegetables, meat, and poultry contain minimal amounts of iodine, whereas dairy products and fish are relatively high in iodine.
The primary pathologic abnormality is increased bone resorption followed by exuberant bone formation prostate cancer veterans 100 mg penegra purchase with visa. However, the newly formed bone is disorganized and of poor quality, resulting in characteristic bowing, stress fractures, and arthritis of joints adjoining the involved bone. The altered bone structure can produce secondary problems, such as deafness, spinal cord compression, high-output cardiac failure, and pain. Malignant degeneration to osteogenic sarcoma is a rare but lethal complication of Paget disease. Vitamin D Deficiency Vitamin D deficiency results in inadequate absorption of Ca2+ and phosphate. In children, the result is failure to mineralize newly formed bone and cartilage matrix, causing the defect in growth known as rickets. Pathologically, lesions are typical of hyperparathyroidism (osteitis fibrosa), 896 vitamin D deficiency (osteomalacia), or a mixture of both. The underlying pathophysiology reflects increased serum phosphate and decreased calcium, leading to the loss of bone. Pharmacological Treatment of Disorders of Mineral Ion Homeostasis and Bone Metabolism Hypercalcemia Hypercalcemia can be life threatening. Such patients frequently are severely dehydrated because hypercalcemia compromises renal concentrating mechanisms. Thus, fluid resuscitation with large volumes of isotonic saline must be early and aggressive (68 L/d). Agents that augment Ca2+ excretion, such as loop diuretics (see Chapter 25), may help to counteract the effect of plasma volume expansion by saline but are contraindicated until volume is repleted. The response to steroid therapy is slow; from 1 to 2 weeks may be required before plasma Ca2+ concentration falls. Reduction in Ca2+ can be rapid, although "escape" from the hormone commonly occurs within several days. The recommended starting dose is 4 units/kg of body weight administered subcutaneously every 12 h; if there is no response within 12 days, the dose may be increased to a maximum of 8 units/kg every 12 h. If the response after 2 more days still is unsatisfactory, the dose may be increased to a maximum of 8 units/kg every 6 h. Intravenous bisphosphonates (pamidronate, zoledronate) have proven very effective in the management of hypercalcemia (see further material for discussion of bisphosphonates). With pamidronate, resolution of hypercalcemia occurs over several days, and the effect usually persists for several weeks. Zoledronate has largely superseded pamidronate because of its more rapid normalization of serum Ca2+ and longer duration of action. Reduction in plasma Ca2+ concentrations occurs within 2448 h when a relatively low dose of this agent is given (1525 g/kg of body weight) to minimize the high systemic toxicity of the drug; indeed, its toxicity generally precludes its use. Once the hypercalcemic crisis has resolved, or in patients with milder calcium elevations, long-term therapy is initiated. Parathyroidectomy remains the only definitive treatment of primary hyperparathyroidism. Therapy of hypercalcemia of malignancy ideally is directed at the underlying cancer. When this is not possible, parenteral bisphosphonates often will maintain Ca2+ levels within an acceptable range. Patients with moderateto-severe hypocalcemia are typically treated by intravenous infusion of calcium gluconate at a dose of 1015 mg of Ca2+/kg of body weight over 46 h. Because the usual 10-mL vial of a 10% solution contains only 93 mg Ca2+, many vials are needed. Treatment with intravenous Ca2+, administered as calcium gluconate (1030 mL of a 10% solution), also may be lifesaving in patients with extreme hyperkalemia (serum K+ > 7 mEq/L). The intramuscular route should not be employed because abscess formation at the injection site may result. For control of milder hypocalcemic symptoms, oral medication suffices, frequently in combination with vitamin D or one of its active metabolites. Calcium carbonate is relatively inexpensive and well tolerated, so it is prescribed most frequently. Bile is essential for adequate absorption of vitamin D and is also the primary route of vitamin D excretion. Patients who have intestinal bypass surgery or inflammation of the small intestine may fail to absorb vitamin D sufficiently to maintain normal levels; hepatic or biliary dysfunction also may seriously impair vitamin D absorption. Absorbed vitamin D circulates in the blood in association with vitamin Dbinding protein. The vitamin disappears from plasma with a t1/2 of 2030 h but is stored in fat depots for prolonged periods. Nutritional rickets results from inadequate expo- Hypocalcemia and Other Therapeutic Uses of Calcium Calcium is used in the treatment of calcium deficiency states and as a dietary supplement. Calcium chloride (CaCl2 2H2O) contains 27% Ca2+; it is valuable in the treatment of hypocalcemic tetany and laryngospasm. Injections of calcium chloride are accompanied by peripheral vasodilation and a cutaneous burning sensation. The rate of injection should be slow (not more than 1 mL/min) to prevent cardiac arrhythmias from a high concentration of Ca2+. Infants and children receiving adequate amounts of vitamin Dfortified food do not require additional vitamin D; however, breastfed infants or those fed unfortified formula should receive 400 units of vitamin D daily as a supplement (see Table 481) (Wagner et al.
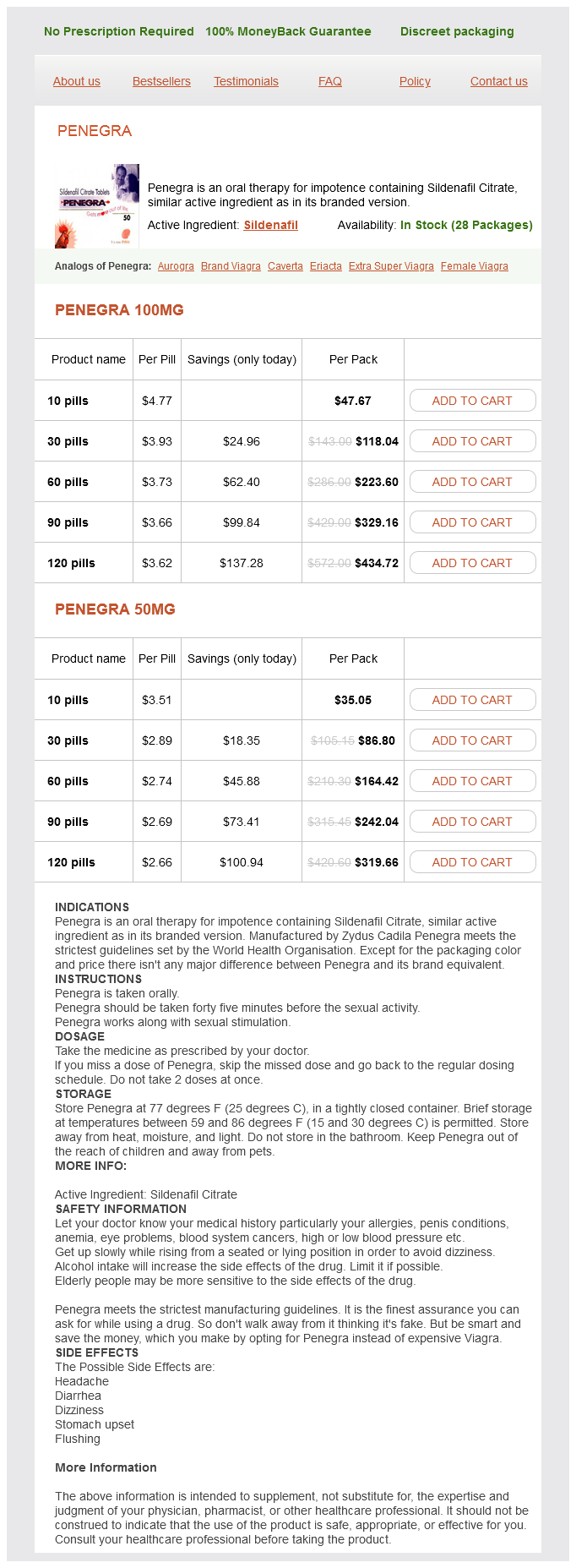
Penegra Dosage and Price
Penegra 100mg
- 10 pills - $47.67
- 30 pills - $118.04
- 60 pills - $223.60
- 90 pills - $329.16
- 120 pills - $434.72
Penegra 50mg
- 10 pills - $35.05
- 30 pills - $86.80
- 60 pills - $164.42
- 90 pills - $242.04
- 120 pills - $319.66
About 30%50% of all patients who receive chronic glucocorticoid therapy ultimately will develop osteoporotic fractures mens health yogurt 50 mg penegra order with visa. Glucocorticoids preferentially affect trabecular bone and the cortical rim of the vertebral bodies; the ribs and vertebrae are the most frequent sites of fracture. In addition, glucocorticoid inhibition of intestinal Ca2+ uptake may lead to secondary increases in parathyroid hormone, thereby increasing bone resorption. The initiation of glucocorticoid therapy at 5 mg/d or more of prednisone (or its equivalent) for 3 months or longer is an indication for bone densitometry to detect abnormalities in trabecular bone. Because bone loss associated with glucocorticoids predominantly occurs within the first 6 months of therapy, densitometric evaluation of the lumbar spine and hip, along with prophylactic measures, should be initiated. An important advance in the prevention of glucocorticoid-related osteoporosis is the successful use of bisphosphonates. Osteonecrosis (also known as avascular or aseptic necro- sis) is a relatively common complication of glucocorticoid therapy. The femoral head is affected most frequently, but this process also may affect the humeral head and distal femur. Joint pain and stiffness usually are the earliest symptoms, and this diagnosis should be considered in patients receiving glucocorticoids who abruptly develop hip, shoulder, or knee pain. Although the risk increases with the duration and dose of glucocorticoid therapy, osteonecrosis also can occur when high doses of glucocorticoids are given for short periods of time. Osteonecrosis generally progresses, and most affected patients ultimately require joint replacement. Growth retardation in chil- dren can result from administration of relatively small doses of glucocorticoids. Although the precise mechanism is unknown, there are reports that collagen synthesis and linear growth in these children can be restored by (off-label) treatment with growth hormone; further studies are needed to define the role of concurrent treatment with growth hormone in this setting. In experimental animals, antenatal exposure to glucocorticoids is clearly linked to cleft palate and altered neuronal development, ultimately resulting in complex behavioral abnormalities. The actions of glucocorticoids to promote cellular differentiation play important physiological roles in human development in late gestation and in the neonatal period. Babies born to women receiving large doses of corticosteroids during pregnancy should be monitored for signs of adrenal insufficiency and appropriate therapy initiated, if necessary. If some benefit is not observed quickly, then the dose should be doubled or tripled. After initial control in a potentially lethal disease, dose reduction should be carried out under conditions that permit frequent accurate observations of the patient. The lack of demonstrated deleterious effects of a single dose of glucocorticoids within the conventional therapeutic range justifies their administration to critically ill patients who may have adrenal insufficiency. If the underlying condition does result from deficiency of glucocorticoids, then a single intravenous injection of a soluble glucocorticoid may prevent immediate death and allow time for a definitive diagnosis. If the underlying disease is not adrenal insufficiency, the single dose will not harm the patient. Long courses of therapy at high doses should be reserved for life-threatening disease. Alternate-day therapy with the same glucocorticoids is employed for patients who obtain adequate therapeutic responses on this regimen. Given the number and severity of potential side effects, the decision to institute therapy with glucocorticoids always requires careful consideration of the relative risks and benefits in each patient. For any disease and in any patient, the optimal dose to achieve a given therapeutic effect must be determined by trial and error and periodic reevaluation as the activity of the underlying disease changes or as complications of therapy arise. A single dose of glucocorticoid, even a large one, is virtually without harmful effects, and a short course of therapy (up to 1 week), in the absence of specific contraindications, is unlikely to be harmful. As the duration of glucocorticoid therapy is increased beyond 1 week, there are time- and dose-related increases in the incidence of disabling and potentially lethal effects. Except in patients receiving replacement therapy, glucocorticoids are neither specific nor curative; rather, they are palliative by virtue of their anti-inflammatory and immunosuppressive actions. Finally, abrupt cessation of glucocorticoids after prolonged therapy is associated with the risk of adrenal insufficiency, which may be fatal. When glucocorticoids are to be given over long periods, the dose, determined empirically, must be the lowest that will achieve the desired effect. When the therapeutic goal is relief of painful or distressing symptoms not associated with an immediately life-threatening disease, complete relief is not sought, and the steroid dose is reduced gradually until worsening symptoms indicate that the minimal acceptable dose has been found. Where possible, the substitution of other medications, such as nonsteroidal anti-inflammatory drugs, may facilitate tapering the glucocorticoid Adrenal insufficiency can result from structural or functional lesions of the adrenal cortex (primary adrenal insufficiency or Addison disease) or from structural or functional lesions of the anterior pituitary or hypothalamus (secondary adrenal insufficiency). In developed countries, primary adrenal insufficiency most frequently is secondary to autoimmune adrenal disease, whereas tuberculous adrenalitis is the most frequent etiology in developing countries. Secondary adrenal insufficiency resulting from pituitary or hypothalamic dysfunction generally presents in a more insidious manner than does the primary disorder, probably because mineralocorticoid biosynthesis is preserved. It usually is associated with disorders of the adrenal rather than the pituitary or hypothalamus and sometimes follows abrupt withdrawal of glucocorticoids used at high doses or for prolonged periods. The immediate management of patients with acute adrenal insufficiency includes intravenous therapy with isotonic NaCl solution supplemented with 5% glucose and corticosteroids and appropriate therapy for precipitating causes such as infection, trauma, or hemorrhage. Because cardiac function often is reduced in the setting of adrenocortical insufficiency, the patient should be monitored for evidence of volume overload, such as rising central venous pressure or pulmonary edema. After an initial intravenous bolus of 100 mg, hydrocortisone should be given by continuous infusion at a rate of 50100 mg every 8 h, a dose that confers sufficient mineralocorticoid activity to meet all requirements. As the patient stabilizes, the hydrocortisone dose may be decreased to 25 mg every 68 h. Thereafter, patients are treated in the same fashion as those with chronic adrenal insufficiency. Failure to respond to cosyntropin in this setting is diagnostic of adrenal insufficiency. Patients with chronic adrenal insuf- ficiency present with many of the same manifestations seen in adrenal crisis but with lesser severity.
© 2025 Adrive Pharma, All Rights Reserved..