General Information about Pariet
In conclusion, Pariet is an efficient medicine for treating acid-related stomach issues. It works by lowering the amount of acid produced in the abdomen, offering aid and selling healing. It is well-tolerated and convenient because of its once-daily dosage. However, as with all medicine, it's essential to make use of it as directed and to tell your doctor of any other medicines or well being circumstances. With the right treatment plan, Pariet can greatly enhance the standard of life for those suffering from acid-related abdomen points.
Pariet is available in pill type and is usually taken as soon as a day. It is essential to take it on the identical time every day for the most effective outcomes. Your doctor may prescribe different medicines, along with Pariet, to assist handle your symptoms. It is crucial to follow your doctor's directions and to not stop taking the medicine with out consulting them first.
Like different PPIs, Pariet works by concentrating on an enzyme within the stomach generally known as the proton pump, which is responsible for producing stomach acid. It does this by binding to the proton pump, preventing it from releasing acid into the abdomen. As a result, the quantity of acid in the stomach decreases, offering reduction and selling therapeutic.
But why is reducing stomach acid manufacturing important? Well, our stomachs produce acid to assist within the digestion of food. However, too much acid can cause discomfort, pain, and harm to the lining of the stomach and esophagus, leading to conditions like ulcers and GERD. These conditions can be debilitating and significantly have an effect on a person's high quality of life. This is the place Pariet comes in, providing aid and therapeutic for those experiencing acid-related stomach issues.
One concern that has been raised about Pariet, and different PPIs, is the potential threat of vitamin and mineral deficiencies. Since stomach acid helps with the absorption of certain vitamins and minerals, lowering its manufacturing might affect their absorption. However, this danger could be minimized by sustaining a healthy diet and taking vitamin and mineral supplements as needed.
Pariet, additionally recognized by its generic name rabeprazole, is a medicine used to treat acid-related abdomen issues corresponding to gastric ulcers, gastroesophageal reflux illness (GERD) and Zollinger-Ellison syndrome. It is a half of a group of medicines generally recognized as proton pump inhibitors (PPIs) that work by lowering the quantity of acid produced within the abdomen.
One of the principle advantages of Pariet is its long-lasting effects. Compared to other PPIs, Pariet has an extended period of action, making it handy for sufferers who prefer taking their treatment as quickly as a day. It is also well-tolerated by most individuals, and unwanted aspect effects are generally mild and uncommon. Some of the identified unwanted effects of Pariet embody headache, nausea, and diarrhea. If these signs persist, it is necessary to speak to your doctor.
However, like another medication, there are some precautions that must be taken when using Pariet. It isn't really helpful for people with liver issues or allergy symptoms to PPIs. It is also important to inform your doctor of any other drugs you take, as some could react with Pariet and affect its effectiveness. Pregnant and breastfeeding ladies also needs to consult their docs before taking Pariet.
The evolution of organ transplantation was mainly related to the introduction of new immunosuppressive drugs such as cyclosporine gastritis diet mango order pariet 20 mg on line, but the development of effective preservation solutions also contributed to a significant extent. The current standard technique of liver preservation is static cold preservation using hypothermia and special preservation solutions. However, the concept of machine perfusion has challenged the standard technique during the past years, and there is growing evidence that continuous machine perfusion might be superior to the simpler cold storage technique. Prepreservation Injury Underlying Liver Disease the prepreservation injury can be related to preexisting liver disease, injury associated with brain death or events leading to brain death, and injury during organ harvest. The most common type of preexisting liver injury is related to steatosis,2,3 which is often related to obesity or alcohol and drug consumption. Steatosis aggravates the cold preservation injury in hepatocytes4 and sinusoidal lining cells5 and increases the magnitude of the reperfusion injury,6-8 which is associated with a higher risk for primary graft failure or severe primary dysfunction. Experimental studies have shown that hepatic arterial flow and microcirculation are significantly impaired in steatotic livers. Screening of potential donors by history, physical examination, drug toxicity and liver function test results, imaging with ultrasound or computed tomography scan, and liver biopsy results rules out most cases of preexisting liver disease. Injury Associated with Cardiopulmonary Arrest or Hypotension Another important component of prepreservation injury is related to the potential injury that is associated with brain death or events leading to brain death. Trauma leading to brain death is often associated with hypotension or hypoxia, which can lead to warm ischemia of the liver. A significant proportion of donors have cardiopulmonary arrest secondary to trauma, drug intoxication, cardiovascular or cerebrovascular event, or any form of asphyxia that leads to brain death. In addition, the management of brain-dead patients is in some instances suboptimal. Injury During Organ Procurement Injury during organ harvesting may occur because of intraoperative hypotension. This type of injury is mainly attributed to hemodynamic instability of the donor during the procurement procedure rather than to technical misadventure. A donor liver biopsy study demonstrated that one third of donors accepted for transplantation have evidence of prepreservation injury in terms of platelet adhesion to sinusoidal lining cells in biopsies taken at the time of organ procurement. This injury is related to warm ischemia secondary to cardiopulmonary arrest before procurement. Warm ischemia starts at the time of extubation and is characterized by hypoperfusion and tissue hypoxemia. Some complex enzymatic energy-dependent reactions have a Q10 between 4 and 6 and are completely inhibited at low temperatures. Nonfunction of the pump causes an osmotic equilibrium of sodium and potassium between the intracellular and extracellular space, resulting in passive sodium influx into the cell. The influx of sodium ions is further enforced by intracellular negatively charged proteins (anions). The intracellular hyperosmolarity finally results in water uptake, which leads to cell swelling, formation of protruding pockets, and lysis. Pathophysiology of Ischemic Cascade Although cooling of organs reduces the metabolic demand, some metabolic reactions are not stopped at low temperatures. Ischemia also promotes the conversion of xanthine hydrogenase to xanthine oxidase, which further catalyzes the degradation of hypoxanthine in the presence of oxygen. There is documented evidence that the risk for graft nonfunction and failure is related to the time interval from donor extubation to cardiac arrest, the duration of postextubation hypotension and hypoxemia. Cold Preservation Injury Although cold preservation injury caused by deleterious effects of hypothermia and ischemia affects all types of liver cells (hepatocytes, biliary cells, sinusoidal lining cells), there is established evidence that sinusoidal lining cells are particularly vulnerable to cold preservation, which is considered to be the main mechanism of this injury. There is established evidence that increased length of cold ischemia translates into inferior outcome after liver transplantation. The hepatic core temperature reaches equilibrium near 0° C during static cold storage in the ice box. In addition, the large impermeable macromolecules S (raffinose) and A- (lactobionic acid) are the extracellular opponent to intracellular P-. During cold preservation this reaction is very slow because of the short supply of molecular oxygen. Intracellular acidosis is mainly attributed to anaerobic glycolysis because lactic acid is the end product of this metabolic pathway. In addition, the activation of lipoprotein lipases and lysosomal hydrolases by intracellular acidosis causes membrane damage leading to increased permeability. Under physiological conditions the extracellular calcium concentration (1 to 2 mM) is approximately 104-fold higher than the intracellular concentration (0. This gradient is maintained by membrane-bound Ca2+ translocase and Na+-Ca2+ exchange mechanisms, both of which are energy dependent. The enormous increase in cytosolic calcium activates Ca2+-dependent phospholipases and proteases, which have damaging effects on cellular structures and membranes. These changes result in impairment of cellular integrity and progress to cell death. This was shown first in animal models34,35 and then confirmed in human allografts. Changes in liver core temperature during preservation and rewarming in human and porcine liver allografts. The reperfusion injury has two phases: (1) the immediate tissue damage upon reperfusion and (2) the injury that is caused by sterile inflammation as immunological response to the immediate insult. This damage is associated with mitochondrial injury and cell death, as well as platelet and leukocyte adhesion, which can further lead to microcirculatory disturbances or intravascular thrombosis (no-reflow phenomenon). All the early pathophysiological events initiate a sterile inflammatory immune response that amplifies local tissue destruction and triggers the activation of cell death programs. Now we will consider the most important mechanisms of the injury that occurs during and after reperfusion of the allograft. Mitochondrial Injury and Cell Death Immediately after reperfusion, parenchymal cells injured by cold and warm ischemia are stressed by reoxygenation.
In Massive Transfusion Coagulopathy Because standard laboratory tests often take too long to obtain, and with severe hemorrhage, several blood volumes may be replaced by the time the results are available, laboratory testing plays an uncertain role in decision making in many settings where massive transfusion is necessary gastritis stool pariet 20 mg without a prescription. One large study of civilian massive transfusion patients demonstrated improved survival with increased use of platelets. Current studies are underway to determine what the optimal ratios should be in a variety of clinical settings. Role of Red Blood Cells and Anemia Anemia may also contribute to bleeding as reported in nonsurgical patients due to multiple mechanisms that 664 Part V · Blood and Hemostasis a perioperative setting, blood warmers and other warming devices should be used to prevent and treat hypothermia. Bleeding and coagulopathy associated with massive transfusions in 21 acutely traumatized soldiers that occurred after transfusion of 20 t o 25 u nits of stored whole blood was described. Transfusion of approximately 15 t o 20 u nits caused significant dilution of blood volumes, and critical decreases in platelet count to approximately 20,000 to 30,000/mm3, far below the recommended platelet target goals in actively bleeding patients. Contact activation associated with tissue injury and hemostatic activation also activates kallikrein that initiates plasmin generation but also is involved in other proinflammatory steps including neutrophil chemotaxis and chemokinesis. During delivery, a systemic hemostatic state develops with consumption of platelets and coagulation factors (including fibrinogen) to allow clotting to occur; hemostasis then normalizes within 4 to 6 weeks postpartum. Older transfusion algorithms only recommend initiating treatment when fibrinogen levels are less than 100 mg/ dL and it may be difficult to reverse the effects of such low levels of this vital component of hemostatic function. European guidelines have focused on the role of normal fibrinogen levels in the bleeding patient, and recent studies also support the potential blood-sparing effects of fibrinogen concentrates. Standard plasma-based coagulation tests also do not provide information about platelet function or interactions with coagulation factors and can be prolonged even with normal clotting factor levels due to protein C deficiency. As a result, other coagulation tests are being used more and more for managing massive transfusions. Some of the advantages of using these systems include the ability to rapidly have information for the diagnosis and management of coagulopathy and also provide methods for algorithm- and goaldirected management. Thromboelastometry provides information about clot formation and fibrin polymerization and its use has been reported for evaluating abnormal trauma-induced coagulopathy. The role of these advanced tests Hypofibrinogenemia Fibrinogen is a critical component in clot formation and an acute-phase reactant protein. Fibrinogen circulates in the highest concentration of all of the coagulation factors, and normal values for plasma levels are approximately 200 to 400 mg/dL but increase in pregnancy and as a nonspecific anabolic postoperative response following tissue injury. Although be- Chapter 31 · Physiology and Management of Massive Transfusion 665 during massive transfusion continues to evolve as therapeutic strategies for transfusion and treatment algorithms are developed. In European countries where cryoprecipitate may not be available, these assays are used as therapeutic guides f or both fibrinogen concentrate and prothrombin complex concentrate administration. S pecific considerations for the management have been discussed and are also included in the following perspectives regarding individual component therapy. Plasma/Fresh Frozen Plasma Overall, developing massive transfusion protocols has been an important therapeutic tool for effectively managing life-threatening hemorrhage after trauma. There are major differences in the management of severe hemorrhage between the United States and Europe. Fibrinogen and other factor concentrates have been used for many years in Europe, as cryoprecipitate is not available in all countries. If patients have received antiplatelet agents recently, then even the existing platelets and platelet counts may not be helpful. Therefore, if pa- tients have received antiplatelet agents or are bleeding after separation from cardiopulmonary bypass, then platelet dysfunction should be suspected and platelet concentrates considered. However, there are signifi ant potential adverse events associated with platelet administration. Inhibiting fibrinolysis during acute bleeding has many benefic al effects including preserving initial clot formation at a bleeding site that may otherwise be broken down, similar to the clot destruction seen in hemophilia. Tranexamic acid is also approved in the United States for excessive menstrual bleeding at a dose of 1. Despite the efficacy and safety of tranexamic acid, clinicians often substitute epsilon-aminocaproic acid, another lysine analog, although this agent has not been studied as well as tranexamic acid and is not available in some European countries. The off- abel use of many of these agents to increase clot formation following major surgery and or traumatic injury is a reasonable but empiric approach for treating life-threatening bleeding and often used as a "last-ditch effort" in patients with ongoing bleeding and at risk for death or other adverse events. When clinicians are presented with a patient who continues to bleed despite standard therapeutic interventions, they have two choices. Clinicians are justified in choosing a procoagulant plan of action for several reasons. Second, persisting with standard interventions will likely not achieve this goal and will unnecessarily expose patients to the risks of excessive blood product administration. Th rd, the efficacy and safety data from most randomized trials are not applicable to these situations because patients with refractory bleeding were not studied. Fourth, even if the safety data from randomized trials do apply, which all suggest that procoagulants by virtue of their effects increase the risk of thromboembolic complications, this risk is relative to that of allowing bleeding and exsanguination to occur. Fifth, observational data from Europe and some randomized trial data in bleeding patients suggests that use of procoagulant therapy and concentrates is effective for refractory blood loss using factor concentrate driven algorithms. Finally, given the ethical implications and impracticality of such trials, it is unlikely that additional applicable data from placebo-controlled randomized trials to evaluate life-threatening hemorrhage will ever be performed. If initial therapy fails to stop bleeding and uterine atony persists, second- and third-line interventions, including mechanical or surgical maneuvers, that is, intrauterine balloon tamponade or hemostatic brace sutures with hysterectomy are the final surgical option for uncontrollable bleeding. From information learned from combat and battlefield casualties, a m ultimodal and multispecialty approach has evolved that includes perspectives from surgeons, anesthesiologists, emergency medicine physicians, and transfusion medicine specialists for the optimal resuscitative approach to hemorrhagic shock. When evaluating the causes of coagulopathy in this setting, preexisting pharmacotherapy including prior use of anticoagulants must be considered. The role of hypothermia, dilutional coagulopathy, platelet dysfunction and fibrinolysis should 668 Part V · Blood and Hemostasis 6. Managing new oral anticoagulants in the perioperative and intensive care unit setting. Recombinant activated factor vii: the controversial conundrum regarding its off- abel use.
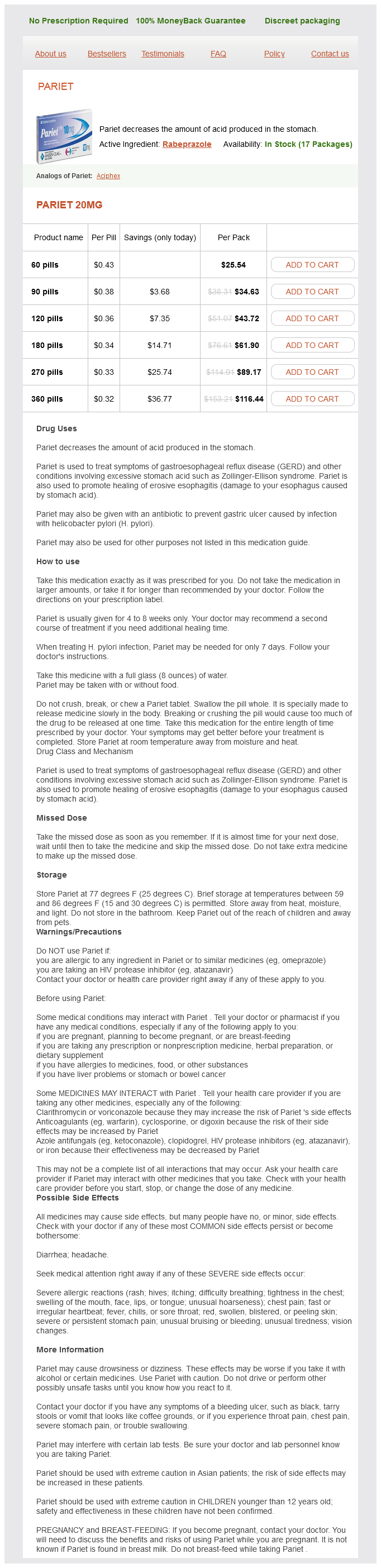
Pariet Dosage and Price
Pariet 20mg
- 60 pills - $25.54
- 90 pills - $34.63
- 120 pills - $43.72
- 180 pills - $61.90
- 270 pills - $89.17
- 360 pills - $116.44
In this process, calcium is removed from troponin C binding sites, triggering the dissociation of actin and myosin, thus facilitating isometric relaxation gastritis diet plan foods cheap 20 mg pariet with mastercard. Active diastolic relaxation uses approximately 15% o f the energy consumed during the cardiac cycle. This process is significantly impaired in the elderly and exacerbates the adverse effects of ventricular hypertrophy on diastolic filling. As such, the elderly heart is markedly dependent on the atrial "kick" for adequate ventricular preload. It is estimated that atrial contraction contributes approximately 30% of ventricular filling in the elderly versus 10% in younger individuals. Because of the importance of atrial contraction, Aging and the Cardiovascular System Increasing age is associated with increasing cardiac morbidity. Aging is associated with an increasing prevalence of cardiovascular disease and decreasing cardiovascular functional reserve. However, it is important to separate the cardiovascular effects of aging from those of common diseases with increased prevalence in the elderly, such as atherosclerosis, hypertension, and diabetes mellitus. The decline in cardiac function that occurs with aging in the healthy individual appears to be related, in part, to decreasing functional demand. Indeed, when exercise and low-calorie diet are maintained into the later decades, the decline in cardiovascular function is markedly attenuated. Important functional changes include arterial hypertrophy resulting in increased afterload, ventricular hypertrophy resulting in elevated systolic blood pressure, loss of cells in the electrical conduction system predisposing to arrhythmia, and loss of sensitivity to catecholamines resulting in reduced maximal heart rate and heart rate variability. Tachycardia and shortened diastolic intervals are associated with marked decreases in ventricular preload in the elderly. Loss of the atrial kick is particularly poorly tolerated by elderly patients because of decreased capacitance of the left ventricle from the previously noted changes. Perioperative events that reduce venous return, such as hypovolemia, positive pressure ventilation, and increased venous capacitance, may be accompanied by signifi ant decreases in cardiac output. Conversely, excessive perioperative increases in blood volume or decreases in contractility can precipitate congestive cardiac failure. Diastolic dysfunction is now recognized as a major contributor to cardiovascular disease in the elderly population and is exacerbated by several coexisting diseases8,9 (Table 46-1). It is difficult to distinguish systolic dysfunction from diastolic dysfunction during routine clinical evaluation. Furthermore, routine preoperative echocardiographic indices of function such as left ventricular ejection fraction will fail to identify diastolic dysfunction. However, diastolic filling can be evaluated by comparing Doppler echocardiographic measurements of mitral valve inflow velocities during the early and late (atrial contraction) phases of diastole. Dyspnea in the elderly may indicate congestive cardiac failure and/ or pulmonary disease. Large Vessels Structural changes in the large vessels are an important element of the aging process and contribute significantly to the age-related changes in the heart described earlier. The sinoatrial node, atrioventricular node, and conduction bundles also become infiltrated with fibrous and fatty tissue. These changes are responsible for the increased incidence of first- and second-degree heart block, sick sinus syndrome, and atrial fibrillation in the elderly. The development of atrial fibrillation is also facilitated by left atrial enlargement, which typically accompanies aging in otherwise healthy individuals. Otherwise, healthy elderly men also experience an age-related increase in the prevalence, frequency, and complexity of ventricular ectopy. Their intima and media are thickened, causing these vessels to be less distensible. The normal cushioning function of the large vessels is impaired; causing accelerated and enhanced pulse wave propagation. In young adults, the reflected pulse wave generally has lower amplitude and its return from the peripheral circulation is delayed such that diastolic rather than systolic pressure is augmented. Thus, in the elderly, both systolic pressure and pulse pressure are increased and left ventricular afterload is elevated. All of the aforementioned age-related vascular structural changes are accelerated in the presence of hypertension or atherosclerosis. Autonomic and Integrated Cardiovascular Responses Aging is associated with increased norepinephrine entry into the circulation and deficient catecholamine reuptake at nerve endings. Therefore, elevated circulating concentrations of norepinephrine are usual, generating chronically increased adrenergic receptor occupancy. However, the cardiovascular response to increased adrenergic stimulation is attenuated by downregulation of postreceptor signaling and reduced contractile response of the myocardium. The response to exogenously administered b agonists, such as isoproterenol, is similarly attenuated. Receptor downregulation is responsible for the age-related decline in maximum heart rate during exercise. Indeed, receptor downregulation in the elderly makes their cardiovascular function similar to that of a younger individual who has received b-adrenergic antagonists. Impaired baroreceptor reflexes and attenuated peripheral vasoconstriction are partially responsible. Hypovolemia and salt depletion also contribute and are the result of iatrogenic diuretic administration or increased atrial natriuretic peptide release. Orthostatic hypotension is more common in patients who are hypertensive at baseline.
© 2025 Adrive Pharma, All Rights Reserved..