General Information about Norvasc
Hypertension, or high blood pressure, is a common health issue that impacts tens of millions of individuals worldwide. It is sometimes called a “silent killer” as a result of it has no noticeable symptoms, however can cause severe damage to the center and other organs if left untreated. Norvasc is prescribed to assist decrease blood strain and reduce the chance of coronary heart assault and stroke in patients with hypertension.
In conclusion, Norvasc is a commonly prescribed medication for the therapy of hypertension, angina, and other heart-related circumstances. It helps to decrease blood pressure and improve blood circulate, thereby decreasing the risk of heart assault and stroke. While it could cause some gentle unwanted side effects, they are normally short-term and could be managed. It is essential to observe the doctor’s directions and schedule regular check-ups to monitor the effectiveness of the medication. With correct use and precautions, Norvasc might help enhance heart health and high quality of life for individuals who need it.
Norvasc is available in the form of oral tablets in varied strengths, starting from 2.5mg to 10mg. The dosage may range depending on the patient’s age, medical history, and situation being treated. It is often advised to take Norvasc as soon as a day, across the similar time each day, with or with out meals. It must be taken as directed by the doctor and should not be stopped all of a sudden without medical recommendation, as it could possibly trigger a sudden enhance in blood strain.
Norvasc, also known by its generic name amlodipine, is a commonly prescribed medicine used to treat hypertension, chest ache, and other heart-related circumstances. It belongs to a category of medication called calcium channel blockers, which work by relaxing and widening the blood vessels, permitting for easier blood circulate and reducing blood stress.
In uncommon instances, Norvasc could trigger serious unwanted effects corresponding to a rapid or irregular heartbeat, severe dizziness or fainting, and swelling of the throat, tongue, or face. These signs may be signs of an allergic response or a more severe facet effect, and immediate medical consideration should be sought.
Aside from its use in treating high blood pressure, Norvasc can be commonly prescribed for patients with angina, a situation characterized by chest ache or discomfort brought on by decreased blood move to the center. By relaxing and widening the blood vessels, Norvasc helps to enhance blood flow and oxygen provide to the guts, thereby decreasing the frequency and severity of angina episodes.
Norvasc should not be taken by sufferers with a recognized allergy to amlodipine or some other ingredients within the medicine. It is also important to tell the doctor about another medicines or supplements being taken, as they may work together with Norvasc and trigger potential issues.
While Norvasc is generally well-tolerated, like any other treatment, it could cause side effects in some patients. Common unwanted effects could embody headache, dizziness, drowsiness, nausea, and swelling of the legs and ankles. These unwanted effects are normally gentle and subside as the body adjusts to the treatment. However, if these side effects persist or worsen, it is important to consult a doctor.
Overall degree of heat loss within the target tissue depends on both the type of tissue being ablated blood pressure record chart uk 2.5 mg norvasc with visa, and the degree of vascular flow within the tissue itself. Reduction of blood flow to the lesion via angiographic balloon occlusion or particle embolotherapy of a feeding artery may therefore potentiate the effects of thermal ablation therapy. Use of these additional therapies prior to thermal ablation increases the sensitivity of tumor cells to heat and leads to a greater number of cell deaths. The percutaneous approach is the least invasive and is performed most commonly in patients with underlying cirrhosis and surgically unresectable disease. This consultation routinely includes a discussion on the risks and benefits of the procedure, as well as potential alternative treatment options. A complete review of all available imaging studies is performed, and an appropriate approach to the target lesion is planned. All patients undergo an overnight fast prior to a planned ablation procedure, to minimize risk of aspiration on account of sedation used during the procedure itself. Patients may take any necessary cardiac or antihypertensive medications on the morning of the scheduled procedure with a small quantity of water. Insulin-dependent diabetic patients should administer half of their usual morning insulin dose to avoid hyperglycemia. Each patient undergoes an abridged physical examination and a repeat discussion on issues relating to informed consent immediately prior to a scheduled procedure. An intravenous line is then placed for administration of sedative medications and fluids in the perioperative period. At our institution, we do not routinely administer prophylactic antibiotics prior to ablation therapy in the liver, but will do so in the setting of underlying biliary obstruction, an indwelling biliary stent, or prior surgery resulting in an enterobiliary anastomosis. The area is then prepped and draped in sterile fashion and local buffered lidocaine anesthesia is administered both intradermally and to the deeper soft tissues adjacent to the target lesion with a 25-gauge skin needle and 22-gauge spinal needle, respectively. Multiple additional conducting electrodes may be placed in this fashion to assure adequate volume of coagulation and complete treatment of the target lesion. For lesions larger than 2 cm in diameter, larger electrodes or several overlapping ablation zones may be needed to insure adequate thermocoagulation of the target lesion. Appropriate levels of sedation and analgesia vary on a case-by-case basis according to lesion size and location. Following the ablation procedure, the patient is monitored by nursing staff in a postprocedure recovery room for one to two hours prior to being discharged from the department. Patients who receive general anesthesia or conscious sedation require longer monitoring until the effects of sedative medications have completely resolved. Patients undergoing sedation are not permitted to drive a motor vehicle in the postprocedure period and are discharged only under the care of a friend or relative that may provide transportation home. Patients are usually allowed a trial of solid and liquid intake under supervision, prior to leaving the department. If appropriate, patients are allowed to resume their normal diet approximately two hours following the procedure. Each of these manufacturers has focused electrode design on one of three alternative strategies for energy application. Use of multitined devices result in heat deposition over larger tissue volumes, but require longer treatment times. When deployed, the tines of the Radiotherapeutics, Boston Scientific Device (LeVeen electrode) curve back toward the needle, and this device is therefore initially deployed at the more inferior margin of the target lesion. Currently used methodologies are still somewhat experimental, and as of this writing, there is no clearly discernable difference in effectiveness or complication rates of any one device over the others. Perihepatic fluid represents artificial ascites induced by infusion of sterile D5W in to the peritoneal cavity for thermal protection of the adjacent diaphragm. Axial T1 in- and out-of-phase images showing T1 hyperintense regions of coagulative necrosis within the treatment zone. The treatment zone is approximately the same size as the treated lesion, with very little thermal damage to surrounding normal liver parenchyma due to fibrous encapsulation. The overall rate of major complications associated with this procedure is reported to range between 2. Minor complications include subcapsular hematoma, reactive pleural effusion, and partial liver infarction. Progression to complete liver failure was more common in patients with Child-Pugh class B or C cirrhosis, and the presence of underlying biliary obstruction appears to increase the risk for posttreatment sepsis. Symptoms may persist for up to two weeks following treatment, and total duration depends on the volume of tumor necrosis within the liver. Careful positioning of grounding pads may help to direct the flow of current away from the cardiac device and minimize the chance of interaction. At these oscillation frequencies, the electrical charge of a microwave changes polarity nearly two billion times per second, which in turn causes rotation of polar molecules. The higher the applied microwave energy, the greater the rotational forces on water molecules within tissue. This technique does not require the use of grounding pads, which decreases the time required for patient preparation and eliminates the risk of inadvertent patient injury from grounding pad-related skin burns. Depending on whether the percutaneous or surgical approach is performed, a single or multiple thin (14. Application of electrical energy from the generator results in emission of electromagnetic microwaves from the exposed, noninsulated portion of the antenna. Since application of microwave energy within tissue does not require the use of a grounding pad, the procedure is not associated with risk of grounding pad burns.
If the mother gives history of feeding problem or the infant is low weight for age and has no indication for referral the mother is observed for breastfeeding blood pressure chart with age order norvasc 2.5 mg. Breastfeeding is observed to see the signs of attachment and whether the infant is suckling effectively. Mothers of infants with problem in All infants and children with a severe classification (pink) are referred to a hospital as soon as assessment is completed and necessary pre-referral treatment is administered. Successful referral of severely ill infants to the hospital depends on effective counseling of the caretaker. The first step is to give urgent prereferral treatment (written in bold font in identify treatment section of chart). Treatment in Outpatient Clinic and at Home Young infants who have local infection, feeding problem or low weight, or diarrhea with some dehydration should have treatment initiated in clinic which is to be continued at home (Table 30. For example, a child may present with cough and chest indrawing which indicate severe pneumonia. However, some children may present with serious, nonspecific signs called General Danger Signs that do not point to a particular diagnosis. For example, a child who is lethargic or unconscious may have meningitis, severe pneumonia, cerebral malaria or any other severe disease. Great care should be taken to ensure that these general danger signs are not overlooked because they suggest that a child is severely ill and needs urgent attention. The following general danger signs should be routinely checked in all children: (i) history of convulsions during the present illness, (ii) unconsciousness or lethargy, (iii) inability to drink or breastfeed when mother tries to breastfeed or to give the child something to drink, and (iv) child vomits everything. If a child has one or more of these signs, he must be consi dered seriously ill and will almost always need referral. In order to start treatment for severe illnesses without delay, the child should be quickly assessed for the main symptoms and malnutrition and referred urgently to a hospital. Feeding problem or low weight - Skin pustules or umbilical infection: Teach to apply gentian Teach correct positioning and attachment for breastfeeding Teach the mother to manage breast and nipple problems Treat thrush: Tell the mother to paint the mouth of the young infant with gentian violet 0. Cough or difficult breathing A child with cough or diffi cult breathing may have pneumonia or severe respiratory infection. Very sick children with cough or difficult breathing need to be identified as they require antibiotic therapy. Fortunately, one can identify almost all cases of pneumonia by checking for these two clinical signs: fast breathing and chest indrawing. A child presenting with cough or difficult breathing should first be assessed for general danger signs. Based on a combination of the above clinical signs, children presenting with cough or difficult Chart 30. A child with general danger sign or chest indrawing or stri der is classified as severe pneumonia or very severe disease and merits urgent referral to the hospital. A sick child with cough who has fast breathing is classified as pneumonia and his treatment initiated in clinic with oral antimicrobials. A child with cough with none of these signs is classified as cough and cold and given home remedies to soothe throat and counseled for home care. However, a child with chronic cough (more than 30 days) needs to be further assessed (and, if needed, referred) to exclude tuberculosis,asthma,whooping cough or any other problem). Most diarrheal episodes are caused by agents for which antimicrobials are not effective and therefore antibiotics should not be used routinely for treatment of diarrhea. Antidiarrheal drugs do not provide practical benefits for children with acute diarrhea, and some may have dan gerous side effects. In addition a child with diarrhea should be asked how long the child has had diarrhea and if there is blood in the stool. This will allow identification of children with persistent diarrhea and dysentery. All children with persistent diarrhea are classified based on presence or absence of dehydration. Children with per sistent diarrhea and dehydration are classified as severe persistent diarrhea and need to be referred to hospital after treatment of dehydration. Children with persistent diar rhea and no dehydration can be safely managed on out patient basis with appropriate feeding. When diagnostic capacity is limited, it is important first to identify those children who need urgent referral with appropriate prereferral treatment (antimalarial or antibacterial). All sick children should be assessed for fever if it is reported by mother or fever is present on examination. In endemic areas the risk of malaria transmission is defined by areas of high and low malaria risk in the country. A child presenting with fever is assessed and classified depending on risk of malaria. If fever has persisted daily for more than seven days the child needs to be referred to hospital for assessment and diagnostic tests. The other signs looked for in a child with fever include general danger signs (assessed earlier) and signs ofmeningitis,e. If the child has measles currently or within the last three months, he should be assessed for possible complications. In areas with low malaria risk children with fever with no other obvious cause are classified as malaria and should be evaluated with blood smear and treated with oral anti malarial drugs (chloroquine). Since the malaria risk may change with time malaria is treated as per national guidelines.
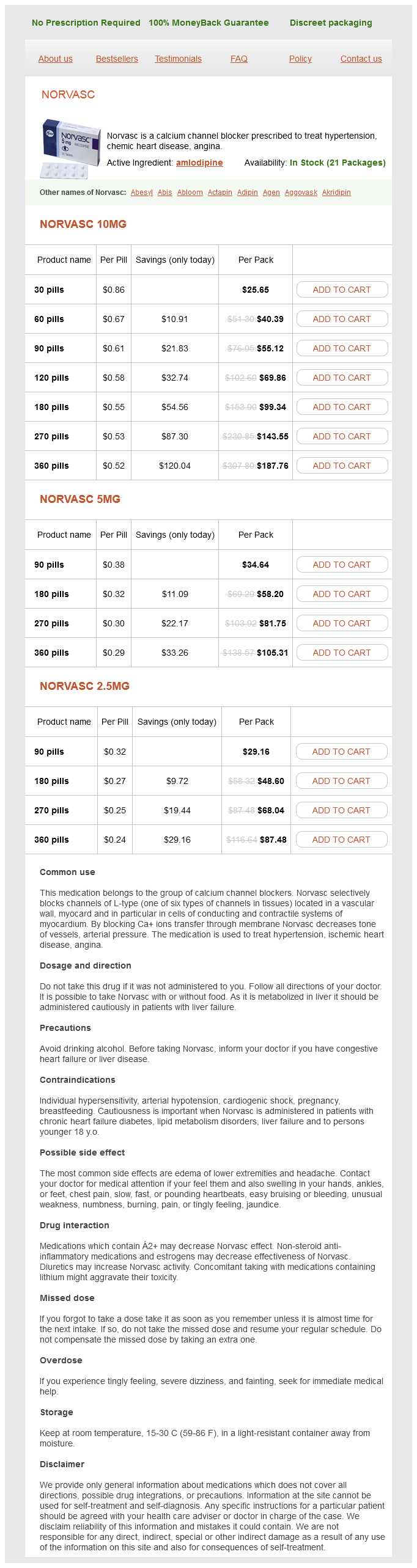
Norvasc Dosage and Price
Norvasc 10mg
- 30 pills - $25.65
- 60 pills - $40.39
- 90 pills - $55.12
- 120 pills - $69.86
- 180 pills - $99.34
- 270 pills - $143.55
- 360 pills - $187.76
Norvasc 5mg
- 90 pills - $34.64
- 180 pills - $58.20
- 270 pills - $81.75
- 360 pills - $105.31
Norvasc 2.5mg
- 90 pills - $29.16
- 180 pills - $48.60
- 270 pills - $68.04
- 360 pills - $87.48
A prospective trial of recombinant human interferon alpha 2B in previously untreated patients with hepatocellular carcinoma hypertension uncontrolled icd 9 code purchase norvasc with a visa. Distribution and therapeutic effect of intraarterially transferred tumor-infiltrating lymphocytes in hepatic malignancies. Recombinant interferon-alpha in inoperable hepatocellular carcinoma: a randomized controlled trial. Combined transarterial targeting locoregional immunotherapy-chemotherapy for patients with unresectable hepatocellular carcinoma: a new alternative for an old problem. Adriamycin, interleukin-2, and lymphokine-activated killer cells versus adriamycin alone. No synergistic activity of epirubicin and interferon-alpha 2b in the treatment of hepatocellular carcinoma. Combined cisplatinum and alpha interferon therapy of advanced hepatocellular carcinoma. Postoperative immunotherapy for patients with hepatocarcinoma using tumor-infiltrating lymphocytes. Alpha1-thymosin and transcatheter arterial chemoembolization in hepatocellular carcinoma patients: a preliminary experience. Systemic combined chemotherapy with low dose of 5-fluorouracil, cisplatin, and interferon-alpha for advanced hepatocellular carcinoma: a pilot study. Interferon therapy after tumor ablation improves prognosis in patients with hepatocellular carcinoma associated with hepatitis C virus. Autologous cytokine-induced killer cell therapy in clinical trial phase I is safe in patients with primary hepatocellular carcinoma. Phase I trial of intratumoral injection of an adenovirus encoding interleukin-12 for advanced digestive tumors. Intratumoral injection of dendritic cells engineered to secrete interleukin-12 by recombinant adenovirus in patients with metastatic gastrointestinal carcinomas. Combined therapy of transcatheter hepatic arterial embolization with intratumoral dendritic cell infusion for hepatocellular carcinoma: clinical safety. Minimally invasive treatment combined with cytokine-induced killer cells therapy lower the short-term recurrence 165. Interferon beta prevents recurrence of hepatocellular carcinoma after complete resection or ablation of the primary tumor-A prospective randomized study of hepatitis C virus-related liver cancer. Effects of long-term postoperative interferon-alpha therapy on intrahepatic recurrence after resection of hepatitis C virus-related hepatocellular carcinoma. Prospective pilot study of recombinant granulocyte-macrophage colony-stimulating factor and interferon-gamma in patients with inoperable hepatocellular carcinoma. Treatment of non-resectable hepatocellular carcinoma with autologous tumor-pulsed dendritic cells. Combined intraarterial 5-fluorouracil and subcutaneous interferon-alpha therapy for advanced hepatocellular carcinoma with tumor thrombi in the major portal branches. A randomized, controlled trial of postoperative adjuvant cytokineinduced killer cells immunotherapy after radical resection of hepatocellular carcinoma. Immunotherapy with cytokine induced killer cells in solid and hematopoietic tumours: a pilot clinical trial. Efficacy of transcatheter arterial chemoembolization combined with cytokine-induced killer cell therapy on hepatocellular carcinoma: a comparative study. These alternatives are often promoted for use instead of mainstream cancer care as viable cancer treatments, but they are typically fraudulent, deliver misleading pseudoscientific information with a heavy commercial bias,1 endorse unproven, potentially harmful therapies,2 and discourage conventional therapies such as surgery, chemotherapy, and radiotherapy, which are referred to as "cutting, poisoning, and burning. Multiple fitness programs are available for patients at all levels of clinical status and include gentle or chair aerobics, qigong, tai chi, strength and balance training, and more. These are safe, evidence-based approaches that optimally should be provided by licensed practitioners who are also trained to work with patients with cancer. Patients may also seek out these therapies because of a poor prognosis even if receiving standard of care, a fear of adverse effects from conventional treatment, a lack of a sense of control in the complicated health care system, a cultural and social affinity to therapies of natural origin, and the belief that unfamiliar therapies may yet hold surprising benefit. In addition, there is the risk of potential side effects or interference with concurrent conventional treatment. Complications related to hepatobiliary surgery can include bleeding, infection, and liver function impairment,29 and the use of natural products such as herbs and dietary supplements may contribute to such complications. In the context of a hepatobiliary and surgical oncology practice, this has led some institutions to routinely provide preoperative instructions to stop using all herbs and supplements one week before any surgery. Reasons for not broaching the discussion of complementary therapies during clinical encounters are bidirectional and manifold. Patients may not think it is important, may fear being ridiculed, or may feel that healthcare professionals do not know enough about the myriad therapies available to render a trustworthy opinion. Healthcare professionals may also choose to avoid the topic, which tends to initiate a time-consuming discussion, the proverbial "opening a can of worms. Furthermore, a healthcare professional may not believe that any particular complementary therapy is of any value to the patient. These issues underscore the important role that healthcare professionals play in soliciting information from patients about their use of adjunctive therapies and in maintaining an open and receptive demeanor when patients disclose their use. Not asking could put patients at risk from adverse interactions or prevent them from undergoing effective therapies due to erroneous advice they receive from unconventional sources. Although many therapies are unproven or have been disproved, some therapies have demonstrated safety and potential benefits to patients. In this case, a patient should be referred to a qualified healthcare professional trained and skilled in discussing the use of complementary therapies as an integrated part of their overall care. Today, most major cancer centers and many community hospitals have established integrative medicine programs to study and combine helpful complementary therapies with mainstream oncology care. The health professionals in these programs are valuable resources for busy oncologists who lack the time or knowledge for in-depth discussions with patients about complementary therapies.
© 2025 Adrive Pharma, All Rights Reserved..