General Information about Molvir
Furthermore, in vitro studies have proven that Molnupiravir is efficient towards multiple variants of SARS-CoV-2, together with the extremely transmissible Delta variant. This gives hope that Molnupiravir might be a priceless device within the battle towards COVID-19, even as the virus continues to mutate and new variants emerge.
What do early research show?
Molnupiravir is an experimental antiviral drug that works by introducing errors into the genetic materials of viruses, in the end leading to their death. It was initially developed for the remedy of influenza, but its broad-spectrum exercise against multiple forms of viruses, including coronaviruses, makes it a promising candidate for the therapy of COVID-19.
Conclusion
Molnupiravir, also referred to as EIDD-2801, is an oral antiviral treatment that has been gaining attention in latest months as a potential remedy for COVID-19. Developed by Ridgeback Biotherapeutics in collaboration with Merck & Co., Molnupiravir is at present in part 3 clinical trials and has proven promising leads to early studies.
Molnupiravir is currently in part 3 scientific trials, that are being conducted in multiple countries, together with the US, UK, and Brazil. The trials aim to enroll roughly 1,850 non-hospitalized sufferers with early signs of COVID-19. The outcomes of those trials are expected to be available within the coming months, and if the drug is shown to be safe and effective, Merck plans to submit an Emergency Use Authorization (EUA) utility to the US Food and Drug Administration (FDA).
If the EUA is granted, Molnupiravir might probably be obtainable for use in the treatment of COVID-19 as early as the tip of this 12 months. Merck has additionally entered into agreements with several nations, including the US, UK, and Australia, for the supply of Molnupiravir, should it receive regulatory approval.
Current status and potential timeline
In conclusion, Molnupiravir is a promising oral antiviral treatment for COVID-19 that has shown promising results in early studies. If proven secure and efficient, it could be a valuable addition to the existing arsenal of therapies for COVID-19, notably within the early stages of the illness. However, further research and regulatory approvals are still needed before it can be extensively out there to the public. Until then, you will want to continue following public health measures such as sporting masks and getting vaccinated to help control the spread of the virus.
Molnupiravir is a prodrug, meaning that it's inactive till it enters the body and is converted into its energetic form. Once inside the body, it's transformed into its energetic form, EIDD-1931, which works by concentrating on an enzyme called RNA-dependent RNA polymerase (RdRp). RdRp is essential for viruses to duplicate their genetic materials, and by inhibiting its exercise, Molnupiravir can doubtlessly stop the virus from replicating and spreading.
Molnupiravir is necessary as a end result of it is an oral treatment, meaning it may be taken at home and doesn't require hospitalization or intravenous administration. This could be a game-changer within the management of COVID-19, as it might help reduce the burden on healthcare techniques and make treatment more accessible to a larger inhabitants.
Early research have shown promising results for Molnupiravir in the remedy of COVID-19. In a part 2a examine, patients who acquired Molnupiravir within 5 days of symptom onset had a considerably shorter time to viral clearance in comparability with those that received placebo. Another examine in ferrets, a species that is identified to be susceptible to SARS-CoV-2, confirmed that Molnupiravir decreased the amount of virus within the animals’ nose and lungs, and prevented transmission to naive animals.
Why is Molnupiravir necessary within the struggle towards COVID-19?
What is Molnupiravir?
How does it work?
Another way of classifying the motor pathways is based on their sites of termination in the spinal cord and the consequent differences in their roles in the control of movement and posture natural antiviral supplements discount molvir 200mg without a prescription. The lateral pathways can excite motor neurons directly, although interneurons are their main target. They influence reflex arcs that control fine movement of the distal ends of limbs, as well as those that activate supporting musculature in the proximal ends of limbs. The medial pathways end in the medial ventral horn on the medial group of interneurons. These interneurons connect bilaterally with motor neurons that control the axial musculature and thereby contribute to balance and posture. In this book, the terms lateral and medial are used to classify the descending motor pathways. However, even this terminology is not perfect, partly because although motor neuron cell bodies form localized columns, motor neuron dendritic trees are rather large and typically span most of the ventral horn. Thus any motor neuron can potentially receive input from so-called medial or lateral system pathways. Flexor motor neuron axon Extensor motor neuron axon the Lateral System Lateral Corticospinal and Corticobulbar Tracts the corticospinal and corticobulbar tracts originate from a wide region of the cerebral cortex. This region includes the primary motor, premotor, supplementary, and cingulate motor areas of the frontal lobe and the somatosensory cortex of the parietal lobe. The cells of origin of these tracts include both large and small pyramidal cells of layer V of the cortex, including the giant pyramidal cells of Betz. Although Betz cells are a defining feature of the primary motor cortex, they represent a small minority (<5%) of the cells that contribute to these tracts, in part because they are found only in the primary motor cortex, and even there they represent a minority of the cells contributing to the tracts. These tracts leave the cortex and enter the internal capsule, then traverse the midbrain in the cerebral peduncle, pass through the basilar pons, and emerge to form the pyramids on the ventral surface of the medulla. The corticobulbar axons leave the tract as it descends in the brainstem and terminate in the motor nuclei of the various cranial nerves. The corticospinal fibers continue caudally, and in the most caudal region of the medulla, about 90% of them cross to the opposite side. They then descend in the contralateral lateral funiculus as the lateral corticospinal tract. The lateral corticospinal axons terminate at all spinal cord levels, primarily on interneurons, but also on motor neurons. The remaining uncrossed axons continue caudally in the ventral funiculus on the same side as the ventral corticospinal tract, which belongs to the medial system. Many of these fibers ultimately decussate (cross) at the spinal cord level at which they terminate. Descending Motor Pathways Classification of Descending Motor Pathways Descending motor pathways were traditionally subdivided into pyramidal and extrapyramidal pathways. This terminology reflects a clinical dichotomy between pyramidal tract disease and extrapyramidal disease. The signs of this disease were originally attributed to the loss of function of the pyramidal tract (so named because the corticospinal tract passes through the medullary pyramid). However, in many cases of pyramidal tract disease, the functions of other pathways are also altered, and most signs of pyramidal tract disease (see the later section "Motor Deficits Caused by Lesions of Descending Motor Pathways") are apparently not caused solely by loss of the corticospinal tract but also reflect damage to additional motor pathways. Major pathways connecting the cortical and brainstem motor areas to the spinal cord are shown. Note that the ventral corticospinal pathway is part of the medial system but is showninAforsimplicity. This number still represents a relatively small proportion of the outflow from the cortex because there are approximately 20 million axons in the cerebral peduncles. Nevertheless, the corticospinal pathway is critical for the fine independent control of finger movement, inasmuch as isolated lesions of the corticospinal tract typically lead to a permanent loss of this ability, even though other movement abilities are often recovered with such lesions. Indeed, in primates, corticospinal synapses directly onto motor neurons are particularly prevalent for the motor neurons controlling finger muscles and are probably the basis of the ability to make independent, finely controlled finger movements. The corticobulbar tract, which projects to the cranial nerve motor nuclei, has subdivisions that are comparable with the lateral and ventral corticospinal tracts. For example, part of the corticobulbar tract ends contralaterally in the portion of the facial nucleus that supplies muscles of the lower part of the face and in the hypoglossal nucleus. This component of the corticobulbar tract is organized like the lateral corticospinal tract. Its function is to excite motor neurons to the proximal extensor muscles to support posture. The medullary reticulospinal tracts arise from neurons of the medial medulla, particularly those of the gigantocellularis reticular nucleus. The tracts descend bilaterally in the ventral lateral funiculus, and they end mainly on interneurons associated with cell groups of medial motor neurons. This tract descends ipsilaterally through the ventral funiculus of the spinal cord and ends on interneurons associated with the medial motor neuron groups. The lateral vestibulospinal tract excites motor neurons that supply extensor muscles of the proximal part of the limb that are important for postural control. In addition, this pathway inhibits flexor motor neurons because it also excites the reciprocal group Ia interneurons that receive group Ia input from extensor muscles, which in turn inhibit flexor motor neurons. The excitatory input to the lateral vestibular nucleus is from both the semicircular canals and the otolith organs, whereas the inhibitory input is from the Purkinje cells of the anterior vermis region of the cerebellar cortex. An important function of the lateral vestibulospinal tract is to assist in postural adjustments after angular and linear accelerations of the head. This tract descends in the ventral funiculus of the spinal cord to the cervical and midthoracic levels, and it ends on the medial group of interneurons. Sensory input to the medial vestibular nucleus from the labyrinth is chiefly from the semicircular canals. This pathway thus mediates adjustments in head position in response to angular acceleration of the head.
As previously discussed hiv infection rate singapore cheap molvir 200mg without prescription, the S-I cortex, like the somatosensory thalamus, has a somatotopic organization. In the S-I cortex the face is represented in the lateral part of the postcentral gyrus, above the lateral fissure. The hand and the rest of the upper extremity are represented in the dorsolateral part of the postcentral gyrus, and the lower extremity on the medial surface of the hemisphere. A map of the surface of the body and face of a human on the postcentral gyrus is called a sensory homunculus. The map is distorted because the volume of neural tissue devoted to a body region is proportional to the density of its innervation. Thus in humans, the perioral area, the thumb, and other digits take up a disproportionately large expanse of cortex relative to their size. The sensory homunculus is an expression of place coding of somatosensory information. A locus in the S-I cortex encodes the location of a somatosensory stimulus on the surface of the body or face. For example, the brain knows that a certain part of the body has been stimulated because certain neurons in the postcentral gyrus are activated. The S-I cortex has several morphological and functional subdivisions, and each subdivision has a somatotopic map. These subdivisions were originally described by Brodmann, and they were based on the arrangements of neurons in the various layers of the cortex, as seen in Nissl-stained preparations. The subdivisions are therefore known as Brodmann areas 3a, 3b, 1, and 2 (see Chapter 10). Cutaneous input dominates in areas 3b and 1, whereas muscle and joint input (proprioceptive) dominates in areas 3a and 2. Thus separate cortical zones are specialized for processing tactile and proprioceptive information. Within any particular area of the S-I cortex, all the neurons along a line perpendicular to the cortical surface have similar response properties and receptive fields. A comparable columnar organization has also been demonstrated for other primary sensory receiving areas, including the primary visual and auditory cortices (see Chapter 8). Nearby cortical columns in the S-I cortex may process information for different sensory modalities. Besides being responsible for the initial processing of somatosensory information, the S-I cortex also begins higher-order processing such as feature extraction. For example, certain neurons in area 1 respond preferentially to a stimulus that moves in one direction across the receptive field but not in the opposite direction. Effects of Lesions of the Somatosensory Cortex A lesion of the S-I cortex in humans produces sensory changes similar to those produced by a lesion of the somatosensory thalamus. However, usually only a part of the cortex is involved, and thus the sensory loss may be confined, for example, to the face or to the leg, depending on the location of the lesion with respect to the sensory homunculus. Pain and thermal sensation may be relatively unaffected, although loss of pain sensation may follow cortical lesions. Conversely, cortical lesions can result in a central pain state that resembles thalamic pain (see "Effects of Interruption of the Spinothalamic Tract and Lesions of the Thalamus on Somatosensory Sensation"). Nociceptors and Primary Afferents the axons that carry painful and thermal sensations are members of the relatively slowly conducting A and C classes. However, not all A and C axons carry pain and temperature information; some respond to light touch in a manner similar to what was described for low-threshold mechanoreceptors. Unlike the case for low-threshold mechanoreceptors in which morphologically distinct receptors correspond to response properties, the A and C axons conveying pain and temperature information appear to originate mostly as "free nerve endings. This ability to sense tissue-damaging stimuli (mechanical, thermal, or chemical) is mediated by what are called nociceptors. Indeed, there appear to be a significant number of C fibers that are silent or unresponsive to any stimuli until first sensitized. The first functional distinction that may be made in the pain system is between A and C axons. A axons conduct signals faster than C fibers do and are thought to underlie what is called first pain, whereas C fibers are responsible for second pain. Thus after a damaging stimulus, one first feels an initial sharp, pricking, highly localized sensation (first pain) followed by a duller, more diffuse, burning sensation (second pain). Experiments in which A or C fibers were selectively activated demonstrated that activity in A fibers produces sensations similar to first pain and that activity in C fibers produces second painlike sensations. Each fiber class in turn forms a heterogeneous group with regard to sensitivity to stimuli. Thus afferents are classified according to both size and their sensitivity to mechanical, thermal, and chemical stimuli. Fibers may have a low or high threshold to mechanical stimulation or be completely insensitive to it. Thermal sensitivity has been classified as responsiveness to warmth, noxious heat, cool, and noxious cold. Note that 43°C and 15°C are the approximate limits above and below which, respectively, thermal stimuli are sensed as painful. Chemical sensitivity to a variety of irritating compounds has been tested, including capsaicin (found in chili peppers), mustard oil, and acids. Afferent fibers may be sensitive to one or more types of stimuli and have been named accordingly. For example, C fibers sensitive only to high-intensity (damaging) mechanical stimuli are called C mechanosensitive fibers, whereas those sensitive to heat and mechanical stimuli are labeled C mechanoheat-sensitive fibers (also called polymodal fibers). Other identified fiber types include A and C cold-sensitive, A mechanosensitive, and mechanoheat-sensitive fibers. Thus there is quite a variety of afferent types; however, the most common afferent type is the C polymodal fiber, which accounts for nearly half of the cutaneous C fibers.
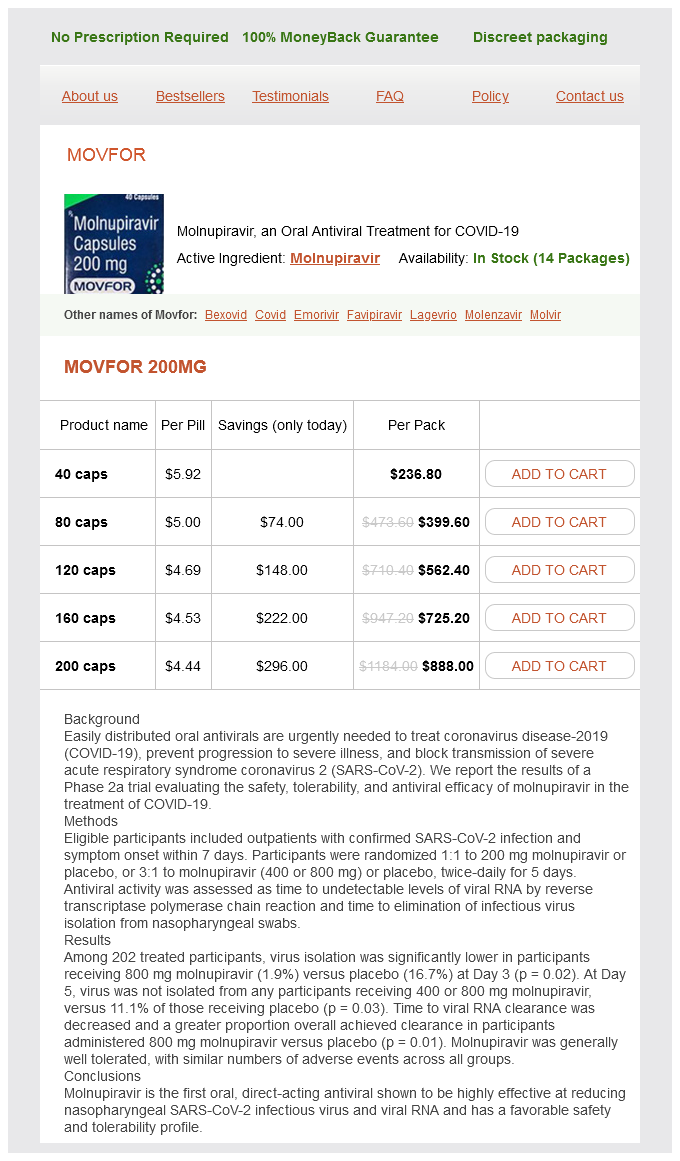
Molvir Dosage and Price
Movfor 200mg
- 40 caps - $236.80
- 80 caps - $399.60
- 120 caps - $562.40
- 160 caps - $725.20
- 200 caps - $888.00
A normal ventilation/perfusion ratio does not mean that ventilation and perfusion of that lung unit are normal; it simply means that the relationship between ventilation and perfusion is normal stages of hiv infection according to who purchase molvir 200 mg overnight delivery. If perfusion to this area remains unchanged, perfusion would exceed ventilation; that is, the ventilation/perfusion ratio would be less than 1 (V /Q < 1). However, the decrease in ventilation to this area produces hypoxic vasoconstriction in the pulmonary arterial bed supplying this lobe. This results in a decrease in perfusion to the affected area and a more "normal" ventilation/perfusion ratio. Nonetheless, neither the ventilation nor the perfusion to this area is normal (both are decreased), but the relationship between the two could approach the normal range. Regional Differences in Ventilation/Perfusion Ratios the ventilation/perfusion ratio varies in different areas of the lung. In an upright individual, although both ventilation and perfusion increase from the apex to the base of the lung, the increase in ventilation is less than the increase in blood flow. As a result, the normal V /Q ratio at the apex of the lung is much greater than 1 (ventilation exceeds perfusion), whereas the V /Q ratio at the base of the lung is much less than 1 (perfusion exceeds ventilation). The relationship between ventilation and perfusion from the apex to the base of the lung is depicted in. The mean value rises approximately 3 mm Hg per decade of life after 30 years of age. In each column, the number on top represents values at the apex of the lung, and the number on the bottom represents values at the base. This small difference in healthy individuals is not caused by "imperfect" gas exchange, but by the small number of veins that bypass the lung and empty directly into the arterial circulation. The thebesian vessels of the left ventricular myocardium drain directly into the left ventricle (rather than into the coronary sinus in the right atrium), and some bronchial and mediastinal veins drain into the pulmonary veins. Arterial Blood Hypoxemia, Hypoxia, and Hypercarbia Arterial hypoxemia is defined as a PaO2 lower than 80 mm Hg in an adult who is breathing room air at sea level. Hypoxia is defined as insufficient O2 to carry out normal metabolic functions; hypoxia often occurs when the PaO2 is less than 60 mm Hg. The six main pulmonary conditions associated with hypoxic hypoxia-anatomical shunt, physiological shunt, decreased FiO2, V /Q mismatching, diffusion abnormalities, and hypoventilation-are described in the following sections and in Table 23. A second category is anemic hypoxia, which is caused by a decrease in the amount of functioning hemoglobin as a result of too little hemoglobin, abnormal hemoglobin, or interference with the chemical combination of oxygen and hemoglobin. Histotoxic hypoxia, the fourth category of hypoxia, occurs when the cellular machinery that uses oxygen to produce energy is poisoned, as in cyanide poisoning. Individuals exposed to carbon monoxide experience headache, nausea, and dizziness, and if it is not recognized, such individuals may die. They often have a cherry-red appearance, and oxygen saturation as measured with an oximeter is high (approaching 100%). Thus it is imperative that the clinician recognize a potential case of carbon monoxide poisoning and order an oxygen saturation measurement with the use of a carbon monoxide oximeter. If a patient has carbon monoxide poisoning, there will be a marked difference between the measurement of oxygen saturation by oximetry and that measured with a carbon monoxide oximeter. The blood and alveolar gas partial pressures are normal values in a resting person at sea level. Ventilation/Perfusion Abnormalities and Shunts Anatomical Shunts A useful way to examine the relationship between ventilation and perfusion is with the twolung unit model. When ventilation is uniform, half the inspired gas goes to each alveolus, and when perfusion is uniform, half the cardiac output goes to each alveolus. In this normal unit, the ventilation/perfusion ratio in each of the alveoli is the same and is equal to 1. An anatomical shunt occurs when mixed venous blood bypasses the gas-exchange unit and goes directly into the arterial circulation. Alveolar ventilation, the distribution of alveolar gas, and the composition of alveolar gas are normal, but the distribution of cardiac output is changed. Some of the cardiac output goes through the pulmonary capillary bed that supplies the gas-exchange units, but the rest of it bypasses the gas-exchange units and goes directly into the arterial circulation. The blood that bypasses the gas-exchange unit is thus shunted, and because the blood is deoxygenated, this type of bypass is called a right-to-left shunt. Most anatomical shunts develop within the heart, and they develop when deoxygenated blood from the right atrium or ventricle crosses the septum and mixes with blood from the left atrium or ventricle. The effect of this right-to-left shunt is to mix deoxygenated blood with oxygenated blood, and it results in varying degrees of arterial hypoxemia. Alveolar ventilation is normal, but a portion of the cardiac output bypasses the lung and mixes with oxygenated blood. An important feature of an anatomical shunt is that if an affected individual is given 100% O2 to breathe, the response is blunted severely. The blood that bypasses the gas-exchanging units is never exposed to the enriched O2, and thus it continues to be deoxygenated. Thus the degree of persistent hypoxemia in response to 100% O2 varies with the volume of the shunted blood. Normally, the hemoglobin in the blood that perfuses the ventilated alveoli is almost fully saturated. The effect of a physiological shunt on oxygenation is similar to the effect of an anatomical shunt; that is, deoxygenated blood bypasses a gas-exchanging unit and admixes with arterial blood. Clinically, atelectasis (which is obstruction to ventilation of a gas-exchanging unit with subsequent loss of volume) is an example of a situation in which the lung region has a V /Q of 0.
© 2025 Adrive Pharma, All Rights Reserved..