General Information about Minocycline
Minocycline works by interfering with the expansion and reproduction of bacteria. It does this by binding to the ribosomal subunit of the micro organism, which is answerable for the production of proteins essential for the bacteria's survival. By blocking this process, Minocycline successfully kills the micro organism and stops the infection from spreading.
In conclusion, Minocycline is a strong antibiotic that is generally used to deal with a wide range of bacterial infections. Its broad spectrum of exercise and talent to penetrate different tissues in the physique make it a extremely efficient therapy possibility for various forms of infections. However, it's always important to comply with the prescribed dosage and to intently monitor any unwanted effects. By utilizing Minocycline appropriately, we are in a position to successfully deal with and manage certain bacterial infections and keep our total well being and well-being.
As with any medication, there are some potential side effects related to the use of Minocycline. These may embody nausea, diarrhea, dizziness, and allergic reactions. In rare circumstances, severe unwanted facet effects corresponding to liver harm, blood problems, and allergic reactions have been reported. Therefore, it is very important converse with a healthcare professional earlier than taking Minocycline and to intently monitor any possible opposed reactions.
One of the principle makes use of of Minocycline is for the treatment of respiratory infections, such as community-acquired pneumonia and bronchitis. It can also be commonly used to treat skin infections similar to acne and rosacea, as well as sure forms of sexually transmitted infections like chlamydia, gonorrhea, and syphilis. In addition, Minocycline can be efficient in treating intra-abdominal infections, urinary tract infections, and different critical bacterial infections.
Minocycline, also recognized by its brand names Minocin and Solodyn, is a robust antibiotic that's generally used to deal with a wide selection of bacterial infections. It belongs to a class of antibiotics generally identified as tetracyclines and is used to deal with a wide range of infections together with respiratory, skin, urinary tract, and sexually transmitted infections.
Minocycline is available in each oral and injectable forms, with the oral type being essentially the most commonly used. It can also be available in several strengths and dosages, relying on the kind and severity of the infection. Typically, it's taken a few times every day for a period of 7-14 days, relying on the an infection being handled.
In addition to its antimicrobial properties, Minocycline has also been found to have anti-inflammatory results. This makes it helpful in the treatment of inflammatory pores and skin conditions, similar to acne and rosacea. It works by decreasing the production of inflammatory substances, which helps to enhance the looks of the pores and skin and reduce the severity of symptoms.
One of the most important benefits of using Minocycline is its ability to penetrate into totally different tissues and fluids in the body. This makes it efficient in treating hard-to-reach infections, similar to these within the respiratory and genitourinary tracts. It is also known for its long-lasting results, which signifies that a single dose can remain lively within the physique for up to 24 hours.
What will you call a cystic mass deep to the sternocleidomastoid muscle bacteria 6th grade science buy discount minocycline on line, which approaches the carotid sheath and has a thin rim The cyst lies superficial to the anterior border of the sternocleidomastoid muscle beneath the cervical fascia. The cyst abuts the carotid sheath and is varyingly adherent to the internal jugular vein. The cyst passes characteristically medially between the internal and external carotid arteries and extends toward the lateral wall of the pharynx. This is a columnar-lined cyst located deep to the carotid vessels abutting the pharynx. The fascia around the carotid sheath is complex in that it may be incomplete in parts or absent in some people, and is uniformly intact only below the bifurcation. Its "incompetency" allows the carotid artery to veer into the retropharyngeal compartment. The carotid space courses down the entire length of the neck and begins at the skull base. These cysts probably arise because of incomplete closure of the cervical sinus of His (not Hers, misogynist). If they connect to the external skin or the pharyngeal mucosa, they are called branchial cleft sinus tracts. If they connect from pharynx to skin, they are considered fistulae (see Table 14-2). Bailey type I is located anterior to the surface of the sternocleidomastoid muscle, deep to the platysma. In a similar fashion, lymphangiomas may infiltrate the contents of the carotid space. Most (75%) occur in the posterior triangle of the neck, with the axilla the next most common site. The source of pericarotid cervical adenitis may be mucosal or odontogenic; tuberculous adenitis; or suppurative adenopathy associated with any pharyngitis can also occur here. Lemierre syndrome is an infection of the oropharynx with internal jugular vein thrombophlebitis and possible septic pulmonary emboli. Iatrogenic causes secondary to venous line placement or surgery may also account for some cases of thrombophlebitis. Typical scenario: a patient with leukemia with an internal jugular line left in just a tad too long. Pseudoaneurysms of the carotid artery may present as a neck mass, usually after traumatic dissection. Somber is the surgeon who rushes to perform a biopsy of this "lesion" before consulting the radiologist. Accelerated atherosclerosis may appear as thickening around the carotid bifurcation, and occasionally you may see intramural hemorrhage into an ulcerated carotid plaque. This axial contrast-enhanced computed tomographic image shows an occluded left internal jugular vein (arrow) and external jugular vein (arrowhead). There is enhancement of the vessel margins and stranding of the soft tissues surrounding these vessels. Carotidynia is a syndrome associated with tenderness, swelling, or increased pulsations over the carotid artery with pain in the ipsilateral neck. Although very few imaging studies have explored this entity, a recent report has noted enhancing soft tissue around the distal common carotid artery and bifurcation region that resolves with nonsteroidal antiinflammatory medication. Differential diagnosis includes giant cell arteritis, dissection, fibromuscular dysplasia,Takayasu arteritis, and wall hematoma. Situated posterior to the carotid artery, vagus nerve lesions tend to displace the carotid artery and parapharyngeal fat in an anterior direction. Occasionally, schwannomas may be cystic and demonstrate characteristic density and intensity features for cyst fluid. A, Axial proton density image shows a right carotid space mass (m) that has variable signal intensity. Note the peripheral rim of signal void and the posterolateral area of dark signal (asterisk). Only the surgeon will know for sure if you are unfortunate enough to recommend biopsy. Note also that the parapharyngeal fat (arrow) is displaced anteromedially by this carotid space lesion. B, Axial computed tomography shows that the majority of the mass is calcified in its rim. There is partial enhancement centrally, indicating that this pseudoaneurysm is only partially thrombosed. The carotid artery (C) is displaced anteromedially and the jugular vein (J) anteriorly by the mass. Note that this tumor is not enhancing as much as one would typically expect of a schwannoma. Glomus Tumor Like schwannomas that may derive from multiple origins, the paragangliomas of the carotid sheath may originate as glomus jugulare, glomus vagale, or carotid body tumors. Carotid body tumors (paragangliomas) usually arise at the carotid bulb and are the most common paraganglioma in the neck.
When a calcified cortex involving intraparenchymal mass is encountered antibiotic used to treat mrsa purchase minocycline 50 mg with mastercard, move from astrocytoma to oligodendrogliomas (these enhance in 40% of cases), and the rare intraparenchymal ependymoma. A mass in the posterior fossa in the adult is most likely a metastasis; one with increased vascularity, a mural nodule, and/or cyst formation is usually a hemangioblastoma or pilocytic astrocytoma. Pediatric Intraaxial Neoplasms As stated previously, the lesions in children tend to be different from those in adults. The differential diagnosis often reduces to a choice of ependymoma, medulloblastoma (primitive neuroectodermal tumor), and pilocytic astrocytoma. Astrocytomas are usually identified in the cerebellar hemispheres more peripherally and most often are cystic with an associated welldefined, enhancing nodule. Medulloblastomas, choroid plexus papillomas, and ependymomas may grow in the fourth ventricle in children. Ependymomas more commonly calcify, usually enlarge the fourth ventricle, and have a propensity for extending out the foramina of Magendie (medially) and Luschka (laterally). Fourth ventricular choroid plexus papillomas are more often seen in older patients; the lateral ventricles are favored in children. Usually, they are identified because of the distorted morphology; the density of these tumors (usually fibrillary astrocytomas) may mimic normal tissue. Worldwide, tuberculosis is a common brain stem lesion, distinguished by greater enhancement and associated leptomeningeal disease. Rhombencephalitis from Listeria monocytogenes may simulate an infiltrative brain stem mass and is a bugger of a bug to try to grow in culture. In the supratentorial space, gangliogliomas, lowgrade astrocytomas, and cortical neuroblastomas predominate in children. These lesions may be identical in appearance, and unless you see cystic areas suggesting Chapter 17 Approach and Pitfalls in Neuroimaging 613 gangliogliomas, arriving at a specific diagnosis is very difficult. In the adult, the major differential diagnosis of a lesion that has mass effect but is nonneoplastic is an infarct. As opposed to neoplastic lesions, infarcts follow a vascular distribution, may involve the gray matter preferentially, and generally are wedge shaped and wider at the cortical surface. Infarcts almost always present with an acute ictus and within a week or two lose mass effect and swelling, whereas neoplasms and untreated infections progress. The diagnosis of acute infarction is no longer the "stroke of genius" thanks to diffusion-weighted scanning. Difficulty arises when infarcts do not appear to be within an arterial distribution and do not obey the anterior, middle, and posterior cerebral artery territories. Depending on which vein/sinus is occluded, one may see deep gray (internal cerebral vein, straight sinus), temporal lobe (transverse sinus, middle cerebral veins, vein of Labbé), or parasagittal (superior sagittal sinus) lesions. Venous infarcts on the whole are hemorrhagic, and often a thrombosed sinus and/or cortical vein (most likely seen on that sagittal T1-weighted image) are seen in association. Herpes preferentially affects the gray matter and white matter of the temporal lobes and frontal lobes, and may be a unilateral or asymmetric bilateral process. Fever, bilaterality, confusion, and a rapidly progressive course over a few days distinguish herpes from tumors. Offer to perform the lumbar puncture to help, if the clinician looks at you cross-eyed. Once again, the differential diagnosis is generally made on clinical grounds, with the viral infections occurring in a younger population and white matter ischemia in an older population with vascular risk factors. Metabolic Disorders Metabolic disorders of the brain can cause signal intensity abnormalities in the basal ganglia and deep gray matter structures as well as within the white matter. As opposed to neoplastic, vascular, or infectious causes, the metabolic diseases generally are bilateral and symmetric processes. Leave these diagnoses to serology, spectroscopy, geneticists, and the fleas-they only deserve four sentences. Demyelinating Disorders When one or more lesions are present in the white matter in the brain of an adult, the differential diagnosis may be extensive. They may induce a large amount of vasogenic edema because of the infection, and they generally arise at the corticomedullary junction, with extension to the gray matter. These lesions are frequently multiple, and the differential diagnosis usually includes metastases. When septic emboli induce abscesses, the differentiation from neoplasm becomes much more difficult. It should be noted, however, that other polyphasic disorders such as Lyme disease, sarcoidosis, and vasculitides can appear in a similar manner. The typical differential diagnosis of monophasic white matter lesions includes acute disseminated encephalomyelitis or posttraumatic white matter shearing injuries. Shearing injuries of the white matter almost always have hemorrhage associated with them on susceptibilityweighted images. When hemorrhage is present in white matter lesions, search for a history of trauma. Typically, posttraumatic injuries, migrainous white matter lesions, progressive multifocal leukoencephalopathy, and dilated Virchow-Robin spaces do not enhance. As opposed to demyelinating disorders, the dysmyelinating, peroxisomal, and metabolic disorders are spotted zebras and tend to be bilateral, symmetric, and more diffuse (bizarre). When diffuse white matter disease is associated with macrocephaly,Alexander and Canavan diseases should be suggested. If the white matter abnormality has an occipital predominance and has an enhancing advancing border, adrenal leukodystrophy is the major diagnosis to consider.
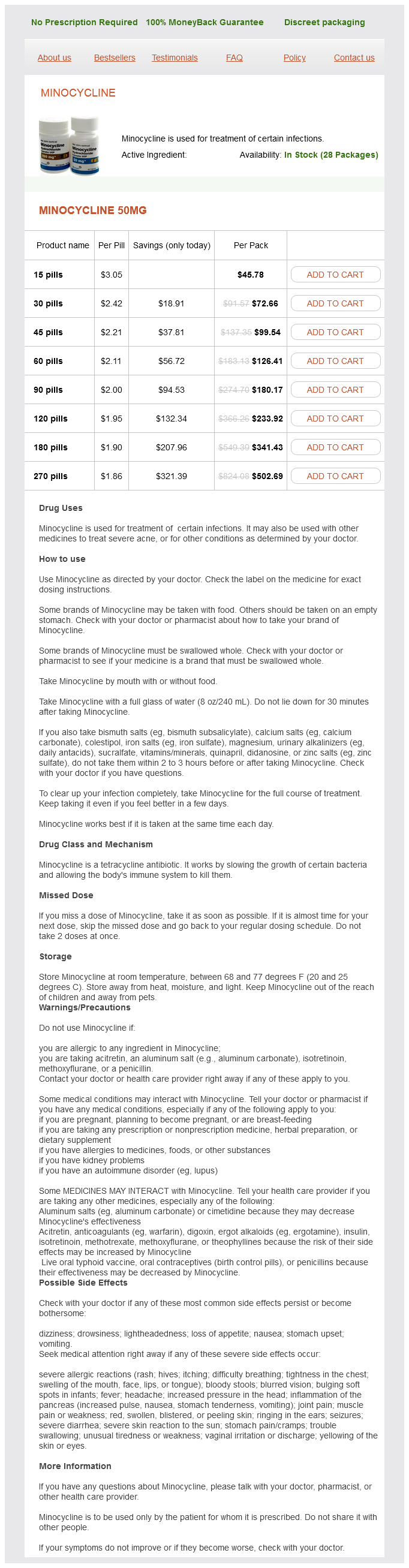
Minocycline Dosage and Price
Minocycline 50mg
- 15 pills - $45.78
- 30 pills - $72.66
- 45 pills - $99.54
- 60 pills - $126.41
- 90 pills - $180.17
- 120 pills - $233.92
- 180 pills - $341.43
- 270 pills - $502.69
A myelomeningocele is identical to a myelocele except for expansion of the ventral subarachnoid space resulting in posterior displacement of the neural placode and stretching of the nerve roots antimicrobial mouth rinses buy minocycline 50 mg mastercard. Myelomeningoceles are typically repaired soon after birth, often without any preoperational imaging, because it is quite clear with visual inspection only. Closed Spinal Dysraphism Skin covered or closed spinal dysraphisms include lipomyelocele and lipomyelomeningoceles (Box 8-10). The prognosis is far better compared with open spinal dysraphism because the neural tissue is covered by the subcutaneous fat and the skin. Then the mesenchymal tissue remains in touch with the neural tube, leading to excess production of fat. The size of the lipomas is variable and the extension can be exclusively intradural or intradural with subcutaneous continuation. Both the open and closed dysraphisms are usually associated with a low-lying, tethered conus medullaris below the L2-L3 disk. In several series involving more than 1000 cases, the normal termination of the conus is above the L2-3 disk level; and less than 2% of normal humans have conus below the L2-3 disk level. Therefore, conus at or below the level of L2-L3 disk space should prompt the search for tethering mass, bony spur or thick filum. The goal of therapy is to (1) enclose the defect into the intraspinal compartment so that infection is prevented, and (2) free up the distal end of the neural tube so that tethering does not occur as the patient grows. If tethering does occur, then downward herniation of intracranial contents through the foramen magnum is a possibility. One of the complications of the surgery is production of fibrous tissue, which may re-tether the dysraphic tissue. On postoperative examination, you may not see a difference in the location of the conus medullaris from the preoperative location. Nonetheless, symptomatic improvement usually occurs even with no change in the site of the bottom of the cord. Large multifocal T2 bright solid masses infiltrating the lower chin and right parotid gland represent infantile hemangiomas. After disjunction the ectoderm closes in the midline, dorsal to the closed neural tube. The perineural mesenchyma migrates into the space between the closed neural tube and ectoderm inducing the formation of meninges, bony spinal column, and paraspinous musculature. In closed spinal dysraphism, the malformed neural tube is covered by mesoderm and ectodermal elements such as subcutaneous fat and skin (see Box 8-8). Spinal bifida occulta refers to presence of defective/incomplete closure of the posterior osseous elements only. Complete/segmental nondisjunction of the cutaneous ectoderm from neural ectoderm results in formation of myeloceles and myelomeningoceles. The clinical and neurological symptoms are believed to arise from two major issues: the neural placode being less functional because of deranged neuroarchitecture, and long-lasting intrauterine exposure of the neural tissue to the amniotic fluid. The myelocele and the myelomeningocele are the most common forms of open dysraphism, with myelomeningoceles more frequently encountered than myeloceles. Dorsal Dermal Sinus these represent an intermediate malformation between open and closed spinal dysraphism but closer to the closed type. The sinus can attach at the dura without transgressing through it, resulting in dural tenting dorsally at the attachment site. Focal/incomplete disjunction of the skin ectoderm and neuroectoderm is believed to be the cause. These are most frequently seen in the lumbosacral and occipital regions (because these are the last portions of the neural tube to close). Only minor bony changes such as hypoplastic spinous process, single bifid spinous process, or laminar defect are noted if any. Secondary neurulation starts after completion of primary neurulation about day 48 of gestation. Fibrolipoma of the Filum Terminale Lipomas of the filum terminale are another form of spinal dysraphism that may cause tethering of the cord. Small amounts of fat (less than 2 mm in transverse diameter) in the filum are usually asymptomatic in kids and may be termed "fibrolipomas. Alternatively, the filum terminale may be markedly thickened and tethered without fatty infiltration (the adult tethered spinal cord syndrome). Sagittal T2-weighted imaging of the cervical spine demonstrates the presurgical (A) and postsurgical (B) cervical myelocele. The condition can be seen in association with urogenital anomalies such as pulmonary hypoplasia (secondary to renal insufficiency) and imperforate anus. Typically, the sacrum and coccyx are absent, and depending on the severity, higher-level vertebral bodies may be missing. Sacrococcygeal Teratoma Sacrococcygeal teratomas are the most common tumor in neonates and can be visualized on prenatal ultrasound. They are thought to arise from the rests of totipotential cells in the caudal cell mass. Previously the upper limit of normal filar thickness was considered to be 2 mm; however, with the advent of higher-resolution thinner slice imaging, now 1 mm in considered as the upper limit of normal. Associated findings with a taut filum terminale (adult tethered cord syndrome) are kyphoscoliosis, midline bony defects in the lumbosacral part of the spine, and fatty infiltration of the filum. Patients may develop conus ischemia, the dreaded sphincteric dysfunction, foot deformities, and abnormal gait. A, Sagittal T2-weighted imaging shows a tethered cord with a T2 and T1 bright (as seen in B) intradural lipoma extends from the subcutaneous fat through the bony spina bifida into the dorsal subarachnoid space (B). Usually it is seen on imaging as a mixed solid and cystic mass; however, purely cystic forms are seen as well.
© 2025 Adrive Pharma, All Rights Reserved..