General Information about Medex
One of the main makes use of of Medex. Coumadin is within the remedy of deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT is a situation by which a blood clot varieties in one of many deep veins in the body, often within the legs. If left untreated, this clot can break off and journey to the lungs, causing a PE which may be life-threatening. Medex. Coumadin helps to dissolve present clots and forestall new ones from forming, reducing the danger of a PE.
In addition to treating DVT and PE, Medex. Coumadin can additionally be used for the prevention of these conditions. People who have had a earlier blood clot are at the next danger for developing one other, and Medex. Coumadin is often prescribed to forestall this from happening. It can also be used to forestall stroke in people who have had a transient ischemic assault (TIA), also referred to as a mini-stroke, or an ischemic stroke caused by a blood clot.
Medex. Coumadin is on the market in pill type and is usually taken as quickly as a day at the identical time, with or without meals. The dose is based on particular person factors corresponding to age, weight, medical condition, and response to treatment. It is necessary to follow the prescribed dosage and not to stop or change the dose without consulting a well being care provider.
Medex. Coumadin, also called warfarin, is an anticoagulant medication that is commonly prescribed for the therapy and prevention of various blood clotting problems. This medicine works by slowing down the manufacturing of sure clotting factors within the blood, reducing the risk of blood clots from forming and causing critical well being complications.
One of the primary considerations with Medex. Coumadin is its potential to trigger bleeding. Since it reduces the blood's ability to clot, it might possibly enhance the risk of bleeding events. Patients taking this treatment should be cautious in participating in actions that will trigger harm and will inform their docs immediately in the occasion that they expertise signs of bleeding, corresponding to unusual bruising or bleeding from the nose or gums.
It can additionally be essential to intently monitor the extent of treatment in the blood to ensure it is within the therapeutic range. This is done through common blood exams and should involve making changes to the dose. Patients taking Medex. Coumadin should also inform their healthcare suppliers earlier than starting some other medication, as certain drugs can interact with it and affect its effectiveness.
Furthermore, Medex. Coumadin is used for secondary prevention of myocardial infarction (MI), commonly known as a heart attack. MI occurs when the move of blood to the guts is blocked, main to damage or dying of the center muscle. Medex. Coumadin is prescribed in combination with other medicines to prevent additional clots from forming and cut back the chance of one other heart attack.
In conclusion, Medex. Coumadin is an anticoagulant treatment that's used for the therapy and prevention of assorted blood clotting issues. It is an essential medicine for individuals at risk for DVT, PE, stroke, coronary heart assault, and different conditions related to blood clots. However, it's important to observe the prescribed dosage, closely monitor its blood levels, and report any concerning signs to ensure protected and effective remedy.
Another important use of Medex. Coumadin is in the prevention of thromboembolic episodes in sufferers with atrial fibrillation (AF). This is a condition during which the heart beats irregularly, increasing the chance of blood clots. Medex. Coumadin is used to stop these clots from touring to the brain and causing a stroke. It is also prescribed for sufferers with cardiac valve injury or those that have had a coronary heart valve alternative.
An additional mechanism for the genesis of brain injury with severe seizures relates to excitatory amino acids anti viral bronchitis purchase medex 5mg visa. The predilection of the limbic system of the newborn for seizure discharges discussed earlier is highly relevant in this regard. The evidence that indicates a major role of excitatory amino acids as mediators of neuronal death with prolonged seizures is summarized in Table 12. A particular vulnerability of the developing brain of the newborn may relate to the rich expression in the developing brain of glutamate receptors, which appear to play an important role in neuronal differentiation and plasticity. The morphological correlates of the functional disturbances involve neuronal developmental abnormalities rather than neuronal cell loss. In addition, dentate granule cell neurogenesis, which, unlike in other cortical areas, persists in the neonatal period, is impaired after recurrent seizures. Consistent with the deleterious effect of recurrent seizures, an observational study of neonatal electrophysiological monitoring of seizures in term infants with hypoxic-ischemic brain injury targeting anticonvulsants to reduce seizure burden was associated with a lower rate of postneonatal epilepsy. First, changes in immediate early genes and posttranslational modifications of existing proteins occur within minutes to hours, whereas transcriptional events and the onset of inflammatory signaling occur within hours to days. Cell death is minimal following seizures in the immature brain compared to the adult. Later changes include gliosis and axonal sprouting, which may contribute to overall network excitability and dysfunction. Although this question remains unanswered, there is mounting evidence that seizures are associated with less favorable neurobehavioral outcomes (see later). Second, many electrographic seizures are not accompanied by clinically observable alterations in neonatal motor or behavioral function; this finding suggests that the occurrence of neonatal seizures may have been underestimated in the past. An initial insult, such as traumatic brain injury and/or status epilepticus, is followed by a latent period lasting weeks to months or even years before the onset of spontaneous seizures. During this latent period, a cascade of molecular and cellular events occurs that alters the excitability of the neuronal network, ultimately resulting in spontaneous epileptiform activity. The alterations that occur during the latent period might provide a good opportunity for biomarker development and therapeutic intervention. Early changes, including the induction of immediate early genes and posttranslational modification of receptor and ion-channel related proteins, occur within seconds to minutes. Within hours to days, there can be neuronal death, inflammation, and altered transcriptional regulation of genes, such as those encoding growth factors. A later phase, lasting weeks to months, includes morphological alterations, such as mossy fiber sprouting, gliosis, and neurogenesis. It is normal for newborns to have some sharp waves, and many newborns with epileptiform discharges do not experience seizures. However, epileptiform discharges that occur in runs or are clustered in one brain region are associated with an increased risk of seizure occurrence. Clearly the 10-second rule is largely arbitrary, and electrographic events with a clinical correlate are generally considered electroclinical seizures even if they last less than 10 seconds. For those seizures with a clinical correlate, the most recent International League Against Epilepsy seizure classification report classifies neonatal seizures according to the same descriptors as seizures at later ages, rather than as a separate entity as had occurred in prior seizure classification systems. Despite great efforts to carefully describe the appearance of neonatal seizures, inter-rater agreement in neonatal seizure identification by clinical observation is suboptimal. Malone and colleagues presented clinical data and video clips of abnormal neonatal movements from 20 newborns to 137 observers, including 91 physicians from seven neonatal intensive care units. Further, interobserver agreement was poor for both physicians and other health care professionals. In addition, 78% of 177 nonictal events were incorrectly identified as seizures, indicating that an overdiagnosis of seizures occurred. A study of 61 seizures in 24 newborns classified seizures by their most prominent clinical features. Clonic and tonic seizures, which might be more readily identified, only occurred in 20% and 8%, respectively, while orolingual, ocular, and autonomic features, which might be more difficult to identify, were the main features in 55%. Four essential clinically evident seizure types can be recognized: subtle, clonic, tonic, and myoclonic (see Table 12. Subtle seizures do not have a clear position in the most recent International League Against Epilepsy seizure classification report,184 but they are very common in newborns and the term is used frequently throughout the literature. In the terminology used later, multifocal refers to clinical activity that involves more than one site, is asynchronous, and, usually, is migratory, whereas generalized refers to clinical activity that is diffusely bilateral, synchronous, and nonmigratory. An important initial distinction in classifying a seizure is whether it has a generalized or focal mechanism of onset. Focal seizures have a defined region of onset, and electrical activity initially spreads through neural networks in that region, although the re fre ks f ok s ks m. The clinical manifestations of certain neonatal oo ks seizure may spread within the hemisphere or to the contralateral hemisphere with time. Spread of the seizure within one hemisphere35 and secondary generalization to the contralateral hemisphere35,36 are less common in newborns than in older children, presumably because the network connections in the newborn brain are not as fully developed (discussed earlier). Taken together, the data indicate that at least some caution should be used in attributing an epileptic origin to subtle clinical phenomena, particularly when these phenomena are the only seizure manifestation. Although apnea has been demonstrated as a seizure manifestation in premature infants,23,187,196 most apneic episodes in the premature infants are not epileptic in origin. A clonic seizure is defined as a seizure characterized by "rhythmic movements of muscle groups in a focal distribution which consist of a rapid phase followed by a slow return movement. Focal clonic seizures involve the face, upper or lower extremities on one side of the body, or axial structures (neck or trunk) on one side of the body. Because focal clonic seizures occur with focal etiologies, it is likely that newborns with only focal clonic seizures have more favorable outcomes than those with other seizures types. Myoclonus is defined as a rapid, isolated ks ks oo oo eb o eb eb ok sf jerk which can affect one or multiple muscle groups, can be eb oo ks fre.
Muscle pathology was striking in six of the nine ks ks oo oo eb o eb eb ok sf patients studied in detail by Carroll and Brooke hiv symptoms eye infection discount medex 5mg with mastercard,237 and it eb oo ks fre Clinical Features. The infantile clinical syndrome, first described by Carroll and Brooke in 1979,237 is characterized by the onset of facial weakness in early infancy. Difficulty in closing the eyes is prominent, and the infant may sleep with the eyes open. However, motor milestones are usually not significantly delayed, and 8 of 11 patients in the largest series walked alone by 15 months of age. Although no specific therapies are available, more details concerning supportive management are available in specialized sources. Of five patients who had reached 15 years of age or more, four were no longer walking, and the remaining patient was walking with difficulty. A similarly progressive disease course has been documented by other investigators. Approximately 50% of subsequently reported cases have exhibited sensorineural hearing loss. However, on careful examination, as many as half of the apparently sporadic cases were found to have an affected parent. Frequently parents are carriers with somatic mosaicism of the mutation and thus may appear unaffected. The defect is particularly interesting and involves a reduction in the number of repeats of a 3. Most patients with 1 to 3 D4Z4 units are usually severely affected with seizures, cognitive delay, and hearing loss and are typically sporadic cases. This gene is embedded within each D4Z4 repeat and encodes a germline transcription factor. Management is similar to that for progressive ks fre ks f oo oo Previously reported in infants no younger than 3 months of age, polymyositis was described in two newborns in 1982. The parents should be counseled that, although the disorder in the affected parent is mild, a distinct possibility exists of a more severe form in the child. Note striking inflammatory response in muscle and significant variation in fiber size and many small basophilic fibers. The finding of perifascicular myopathy, generally considered a feature of such autoimmune myopathies as dermatomyositis, is particularly characteristic. The clinical features are not as prominent as those observed in more common myopathies. Considering the lack of pathological markers, the molecular basis for most of these myopathies may become easier to delineate with the use of extensive panel-based genetic testing. An enormous literature has developed in this area since the 1970s, and several books and reviews deal with the details and complexities of the. Moreover, considerable overlap exists among the disorders on both clinical and histological grounds. Nevertheless, certain specific congenital myopathies are well defined clinically, morphologically, and genetically, and several conclusions relevant to the neonatal patient can be drawn. In the following discussion, we emphasize the most common features of each disorder, particularly those disorders with prominent clinical manifestations in the neonatal period. The mitochondrial myopathies may be suspected by standard histological techniques, but electron microscopic studies are needed to define the distinctive mitochondrial abnormalities if present. Biochemical studies may identify a specific abnormality of a mitochondrial enzyme. The metabolic myopathies may show no distinctive morphological change; thus one could argue that these myopathies should be classified as histology not diagnostic. However, they are included here because the biopsy specimen may indicate glycogen or lipid deposition in muscle, which is usually the critical initial finding in the definition of the specific biochemical lesion. The biopsy demonstrates small type 1 fibers and centrally placed nuclei in the majority of fibers (hematoxylin and eosin). Note the widely spaced nuclei, which affects the number seen in transverse section Most fibers are less than 10 mm in diameter. The clinical syndrome consists of hypotonia and eb o eb eb eb oo ks fre ks ks oo oo ok sf weakness, apparent usually in the neonatal period. However, many infants are not recognized as exhibiting muscle disease until months later. Ptosis, extraocular muscle weakness, dysphagia, and respiratory difficulties have not been features. Slow progression of weakness may occur, but even without this progression, contractures, pes cavus or planus, and kyphoscoliosis may result. In a series of 11 patients followed to the age of 4 to 20 years, 2 were unable to walk alone and 2 had difficulty climbing stairs. Laboratory investigations, aside from muscle biopsy and genetic testing, are not particularly helpful. Muscle pathology is distinctive and diagnostic in the presence of the clinical findings. Single or multiple cores may be observed in a given fiber and are well demonstrated with the histochemical stains for oxidative enzymes. Indeed, electron microscopy shows an absence of mitochondria and sarcoplasmic reticulum in the core region. They have a particular predilection for type I fibers and, in some cases, type I fibers predominate or are the only fiber type observable. The pathogenesis relates to a genetic defect that is usually inherited in an autosomal dominant manner, although rarely autosomal recessive inheritance has been documented. The latter is a ligand-related release channel for internally stored calcium and thereby plays a crucial role in excitation-contraction coupling.
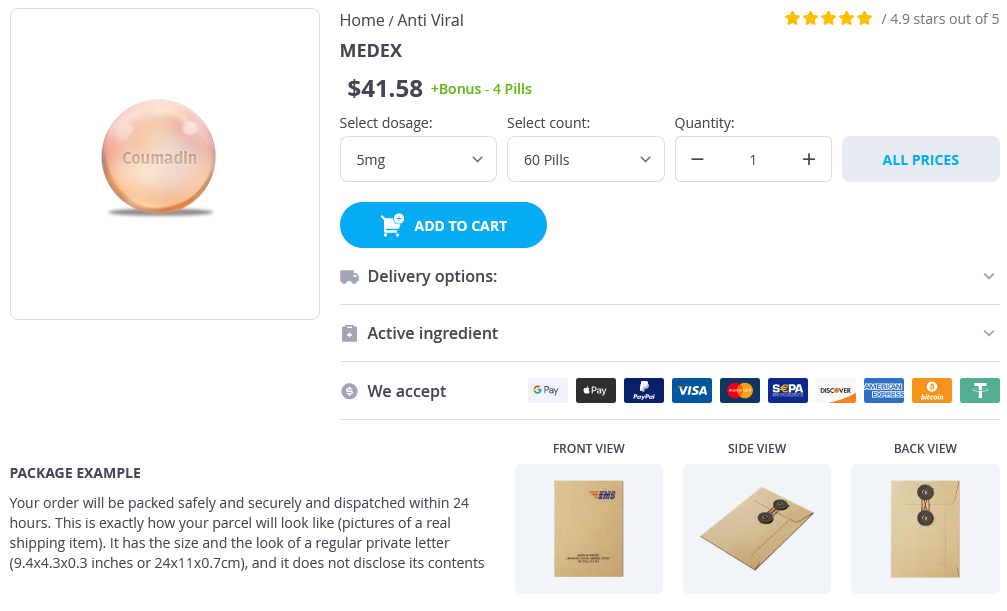
Medex Dosage and Price
Medex 5mg
- 60 pills - $46.20
- 90 pills - $58.49
- 120 pills - $70.78
- 180 pills - $95.36
- 270 pills - $132.22
- 360 pills - $169.09
Medex 1mg
- 90 pills - $39.87
- 180 pills - $63.79
- 270 pills - $87.71
- 360 pills - $111.64
Effective selective head cooling during posthypoxia hypothermia in newborn piglets hiv infection female to male buy 5mg medex fast delivery. Significant selective head cooling can be maintained long-term after global hypoxia ischemia in newborn piglets. Long-term neuroprotective effects of hypothermia on neonatal hypoxicischemic brain injury in rats, assessed by auditory brainstem response. Hypothermia for 24 hours after asphyxic cardiac arrest in piglets provides striatal neuroprotection that is sustained 10 days after rewarming. Head cooling with mild systemic hypothermia in anesthetized piglets is neuroprotective. Significant head cooling can be achieved while maintaining normothermia in the newborn piglet. Cerebral hypothermia is not neuroprotective when started after postischemic seizures in fetal sheep. N-methyl-isobutylamiloride ameliorates brain injury when commenced before hypoxia ischemia in neonatal mice. Neuroprotective effect of hypothermia in cortical cultures exposed to oxygenglucose deprivation or excitatory amino acids. Magnesium sulfate therapy during asphyxia in near-term fetal lambs does not compromise the fetus but does not reduce cerebral injury. The effect of long term caffeine treatment on hypoxic-ischemic brain damage in the neonate. Reduction in cerebral ischemic injury in the newborn rat by potentiation of endogenous adenosine. Enhancing adenosine A(1) receptor binding reduces hypoxic-ischemic brain injury in newborn rats. Neuroprotective effect of phenytoin against in utero hypoxic brain injury in fetal guinea pigs. The cannabinoid agonist Win55212 reduces brain damage in an in vivo model of hypoxic-ischemic encephalopathy in newborn rats. Glutamate uptake and glutamate content in primary cultgures of mouse astrocytes during anoxia, substrate of deprivation and simulated ischemia under normothermic and hypothermic conditions. Brain temperature alters hydroxyl radical production during cerebral ischemia reperfusion in rats. Delayed hypothermia prevents decreases in N-acetylaspartate and reduced glutathione in the cerebral cortex of the neonatal pig following transient hypoxia-ischaemia. Intraischaemic hypothermia reduces free radical production and protects against ischaemic insults in cultured hippocampal slices. Fructose-1,6-bisphosphate preserves intracellular glutathione and protects cortical neurons against oxidative stress. Neuroprotective effects of indomethacin and aminoguanidine in the newborn rats with hypoxic-ischemic cerebral injury. Nitric oxide synthase activity and inhibition after neonatal hypoxia ischemia in the mouse brain. Long-term neuroprotection with 2-iminobiotin, an inhibitor of neuronal and inducible nitric oxide synthase, after cerebral hypoxia-ischemia in neonatal rats. Combination of systemic hypothermia and N-acetylcysteine attenuates hypoxic-ischemic brain injury in neonatal rats. Ebselen, a seleno-organic antioxidant, is neuroprotective after embolic strokes in rabbits-synergism with low-dose tissue plasminogen activator. Prolonged hypothermia protects neonatal rat brain against hypoxic-ischemia by reducing both apoptosis and necrosis. Effects of hypothermia on hypoxia-induced apoptosis in cultured neurons from developing rat forebrain: comparison with preconditioning. Post-ischemic hypothermia blocks caspase-3 activation in the newborn rat brain after hypoxia-ischemia. Combination effect of systemic hypothermia and caspase inhibitor administration against hypoxic-ischemic brain damage in neonatal rats. Potential for protection and repair following injury to the developing brain: a role for erythropoietin The nonerythropoietic asialoerythropoietin protects against neonatal hypoxia-ischemia as potently as erythropoietin. Erythropoietin prevents long-term sensorimotor deficits and brain injury following neonatal hypoxia-ischemia in rats. Erythropoietin after focal cerebral ischemia activates the Janus kinase-signal transducer re fre ok s ks oo oo eb o eb eb eb oo ks ks fre fre. A comparison of high-dose recombinant erythropoietin treatment regimens in brain-injured neonatal rats. Pharmacokinetics of high-dose recombinant erythropoietin in plasma and brain of neonatal rats. Expression of erythropoietin and its receptor in the brain of late-gestation fetal sheep, and responses to asphyxia caused by umbilical cord occlusion. Hypoxia-ischemia affects erythropoietin and erythropoietin receptor expression pattern in the neonatal rat brain. Hypoxia-inducible factor 1 alpha and erythropoietin upregulation with deferoxamine salvage after neonatal stroke. Erythropoietin increases glutathione peroxidase enzyme activity and decreases lipid peroxidation levels in hypoxic-ischemic brain injury in neonatal rats. Regulation of hypoxiainducible factor 1 alpha and induction of vascular endothelial growth factor in a rat neonatal stroke model.
© 2025 Adrive Pharma, All Rights Reserved..