General Information about Macrobid
Macrobid, also known as nitrofurantoin, is an antimicrobial agent from the nitrofurans group that has been in use for over 60 years. It is particularly designed for the remedy of urinary tract infections (UTIs) and has been proven to be highly efficient on this regard. Moreover, it's also used for the prevention of infections after urologic surgical procedure or procedures such as cystoscopy and catheterization.
While Macrobid is usually well-tolerated, like several treatment, it could have some side effects. Commonly reported unwanted side effects embody nausea, vomiting, and headache. In rare instances, it could cause allergic reactions or more extreme side effects corresponding to lung or liver injury. It is essential to inform a healthcare provider of any allergic reactions or medical situations earlier than starting Macrobid therapy.
Urinary tract infections are one of the most common bacterial infections worldwide, affecting each women and men of all ages. The main cause of UTIs is bacteria, and the most typical culprit is Escherichia coli (E. coli). These infections can vary from gentle to severe, with signs like burning sensation throughout urination, frequent urination, and stomach pain. If left untreated, UTIs can result in serious complications similar to kidney injury and sepsis, especially in susceptible populations just like the aged and people with weakened immune techniques.
In conclusion, Macrobid is a crucial and extremely efficient antimicrobial agent in the therapy of UTIs. Its dual mechanism of motion and skill to concentrate in the urinary tract make it an acceptable choice for these affected by this frequent infection. Moreover, its use in preventing infections after urologic procedures has also confirmed to be helpful. It is essential to make use of this medicine judiciously to make sure its efficacy and prevent the event of antibiotic resistance.
In addition to treating UTIs, Macrobid is also used for the prevention of infections after urologic procedures corresponding to cystoscopy and catheterization. These procedures contain the insertion of medical gadgets into the urinary tract, which can introduce micro organism and increase the risk of an infection. By utilizing Macrobid as a preventive measure, the chance of infection can be significantly decreased.
Macrobid is available in both oral and intravenous varieties, with the oral type being the preferred option for treating UTIs. The really helpful dosage and duration of treatment might differ depending on the severity of the an infection and the patient's medical history. It is important to follow the prescribed remedy plan and complete the full course of medication as recommended by the healthcare provider to ensure the whole eradication of the infection.
This is where Macrobid comes into the image as a extremely effective remedy choice for UTIs. It works by disrupting the permeability of the bacterial cell membrane and inhibiting the production of proteins wanted for bacterial development and replication. This twin mechanism of action makes it extremely effective in treating UTIs brought on by a broad range of micro organism. In addition, Macrobid can be efficient towards some strains of antibiotic-resistant micro organism, making it an important software within the fight towards antimicrobial resistance.
One of the most important advantages of Macrobid is its ability to concentrate within the urinary tract and remain active for an prolonged period of time. This makes it perfect for the treatment of UTIs, as it can successfully get rid of the bacteria causing the infection. Furthermore, it also has a low danger of creating resistance, making it a dependable remedy option for recurrent UTIs.
Coat-The coat is composed of a keratin-like protein containing many intramolecular disulfide bonds gastritis diet plan uk generic 50mg macrobid free shipping. The impermeability of this layer confers on spores their relative resistance to antibacterial chemical agents. B anthracis and B cereus) possess an exosporium, but other species (eg, B atrophaeus) have spores that lack this structure. Germination the germination process occurs in three stages: activation, initiation, and outgrowth. Gram-positive cells retain the crystal violet iodine complex, remaining blue; gram-negative cells are completely decolorized by alcohol. As a last step, a counterstain (eg, the red dye safranin) is applied so that the decolorized gram-negative cells will take on a contrasting color; the gram-positive cells now appear purple (Table 2-1). The basis of the differential Gram reaction is the structure of the cell wall, as discussed earlier in this chapter. Among the agents that can overcome spore dormancy are heat, abrasion, acidity, and compounds containing free sulfhydryl groups. Initiation-After activation, a spore will initiate germination if the environmental conditions are favorable. Different species have evolved receptors that recognize different effectors as signaling a rich medium: Thus, initiation is triggered by l-alanine in one species and by adenosine in another. Binding of the effector activates an autolysin that rapidly degrades the cortex peptidoglycan. Water is taken up, calcium dipicolinate is released, and a variety of spore constituents are degraded by hydrolytic enzymes. The Acid-Fast Stain Acid-fast bacteria are those that retain carbolfuchsin (basic fuchsin dissolved in a phenolalcoholwater mixture) even when decolorized with hydrochloric acid in alcohol. A smear of cells on a slide is flooded with carbolfuchsin and heated on a steam bath. After this, the decolorization step with acidalcohol is carried out, and finally a contrasting (blue or green) counterstain is applied (see Chapter 47). Acid-fast bacteria (mycobacteria and some of the related actinomycetes) appear red; others take on the color of the counterstain. Outgrowth-Degradation of the cortex and outer layers results in the emergence of a new vegetative cell consisting of the spore protoplast with its surrounding wall. A period of active biosynthesis follows; this period, which terminates in cell division, is called outgrowth. Negative Staining this procedure involves staining the background with an acidic dye, leaving the cells contrastingly colorless. Basic stains consist of a colored cation with a colorless anion (eg, methylene blue+ chloride-); acidic stains are the reverse (eg, sodium+ eosinate-). Bacterial cells are rich in nucleic acid, bearing negative charges as phosphate groups. Acidic dyes do not stain bacterial cells and hence can be used to stain background material a contrasting color (see Negative Staining). Special staining techniques can be used, however, to differentiate flagella, capsules, cell walls, cell membranes, granules, nucleoids, and spores. The Flagella Stain Flagella are too fine (1230 nm in diameter) to be visible in the light microscope. However, their presence and arrangement can be demonstrated by treating the cells with an unstable colloidal suspension of tannic acid salts, causing a heavy precipitate to form on the cell walls and flagella. In this manner, the apparent diameter of the flagella is increased to such an extent that subsequent staining with basic fuchsin makes the flagella visible in the light microscope. In peritrichous bacteria, the flagella form into bundles during movement, and such bundles may be thick enough to be observed on living cells by dark-field or phase contrast microscopy. The Gram Stain An important taxonomic characteristic of bacteria is their response to Gram stain. The Gram-staining property appears to be a fundamental one because the Gram reaction is correlated with many other morphologic properties in phylogenetically related forms (see Chapter 3). An organism that is potentially gram positive may appear so only under a particular set of environmental conditions and in a young culture. The Gram-staining procedure (see Chapter 47 for details) begins with the application of a basic dye, crystal violet. A solution of iodine is then applied; all bacteria will be stained blue at this point in the procedure. One such "capsule stain" (Welch method) involves treatment with hot crystal violet solution followed by a rinsing with copper sulfate solution. The latter is used to remove excess stain because the conventional washing with water would dissolve the capsule. The copper salt also gives color to the background, with the result that the cell and background appear dark blue and the capsule a much paler blue. The chromosomes are then pushed apart by the inward growth of the septum, one copy going to each daughter cell. The spore wall is relatively impermeable, but dyes can be made to penetrate it by heating the preparation. The same impermeability then serves to prevent decolorization of the spore by a period of alcohol treatment sufficient to decolorize vegetative cells.
Response of vitamin B12 deficiency anemia to treatment is usually rapid gastritis management cheap macrobid amex, with reticulocytosis occurring within 25 days and hematocrit normalizing within weeks. Patients who have vitamin B12 deficiency with associated megaloblastic anemia might experience severe hypokalemia and fluid overload early in treatment due to increased erythropoiesis, cellular uptake of potassium, and increased blood volume. Once treated for a vitamin B12 deficiency due to pernicious anemia or other irreversible problems with absorption, patients need to continue some form of cobalamin therapy lifelong. Folic acid replacement can correct the hematoligic abnormalities of B12 deficiency, but not the neurologic abnormalities. Folic acid deficiency is almost always due to some form of decreased dietary intake. Occasionally, increased requirements from pregnancy, skin loss in diseases like eczema, or increased loss from dialysis and certain anticonvulsants such as phenytoin may occur. The hematologic presentation of folic acid deficiency is identical to B12 deficiency. Hemolytic anemias are caused by decreased red blood cell survival from increased destruction of the cells. The destruction may be either in the blood vessels (intravascular) or outside the vessels (extravascular), which generally means inside the spleen. Hemolytic anemias may either be chronic, as in sickle cell disease, paroxysmal nocturnal hemoglobinuria, and hereditary spherocytosis, or acute, such as in drug-induced hemolysis, autoimmune hemolysis, or glucose 6-phosphate dehydrogenase deficiency. The usual symptoms of anemia are present based on the severity of the disease, not necessarily the etiology. The major difference between hemolytic anemia and the micro- and macrocytic anemias is that hemolysis is more often the etiology when the onset is sudden. Fever, chills, chest pain, tachycardia, and backache may occur if the intravascular hemolysis is particularly rapid. The peripheral smear may aid in the specific diagnosis, and the haptoglobin may be low with intravascular hemolysis. Hemoglobin may be present in the urine when intravascular hemolysis is sudden and severe because free hemoglobin spills into the urine. There should not be bilirubin in the urine because indirect bilirubin is bound to albumin and should not filter through the glomerulus. Hemosiderin may be present in the urine if the hemolysis is severe and lasts for several days. Hydration is, in general, useful to help prevent toxicity to the kidney tubule from the free hemoglobin. A hereditary form of chronic hemolysis ranging from asymptomatic to severe, overwhelming crisis. Hemoglobin S is due to a substitution of a valine for glutamic acid as the sixth amino acid of the beta globin chain. The heterozygous form (trait) is present in 8% of the African-American population, and the homozygous form (disease) is present in 1 in 400 African-Americans. A sickle cell acute painful crisis can be precipitated by hypoxia, dehydration, acidosis, infection, and fever. Sickle cell crisis is most often not associated with an increase in hemolysis or drop in hematocrit. Sudden drops in hematocrit may also be caused by Parvovirus B19 infection or folate deficiency. This drop in hematocrit is from acute aplasia (decrease in cell production), not hemolysis. Chronic manifestations include renal concentrating defects (isosthenuria), hematuria, ulcerations of the skin of the legs, bilirubin gallstones, aseptic necrosis of the femoral head, osteomyelitis, retinopathy, recurrent infections from Pneumococcus or Haemophilus, growth retardation, and splenomegaly followed in adulthood by autosplenectomy. Occasionally some patients will have very severe and life-threatening manifestations of sickling. These include the acute chest syndrome consisting of severe chest pain, fever, leukocytosis, hypoxia, and infiltrates on the chest x-ray. Pregnant patients experience increased rates of spontaneous abortion and low birth weight. The only significant manifestation of trait is the renal concentrating defect presenting with isosthenuria. Those with trait will rarely develop the acute pain crisis under conditions of profound hypoxia and acidosis. The reticulocyte count should always be elevated in the 1020% range unless they have folate deficiency or Parvovirus B19 aplastic crisis. The sickle prep (or Sickledex) is a quick screening test used to diagnose evidence of sickle cell trait and cannot distinguish between trait and homozygous disease. The white blood cell count is often elevated in the 10,00020,000 range, although this can also indicate the presence of infection. Antibiotics are given with infection or even to patients with fever and leukocytosis even if a definite site of infection has not been documented. Ceftriaxone is the preferred agent because it covers Pneumococcus and Haemophilus influenza. Chronic management includes folic acid replacement and vaccinations against Pneumococcus and influenza. Bone marrow transplantation can be curative but should still be considered experimental at this time. Various forms of acquired hemolytic anemias resulting from the production of IgG, IgM, or activation of complement C3 against the red cell membrane. The lysis can be either extravascular or intravascular but is far more often extravascular.
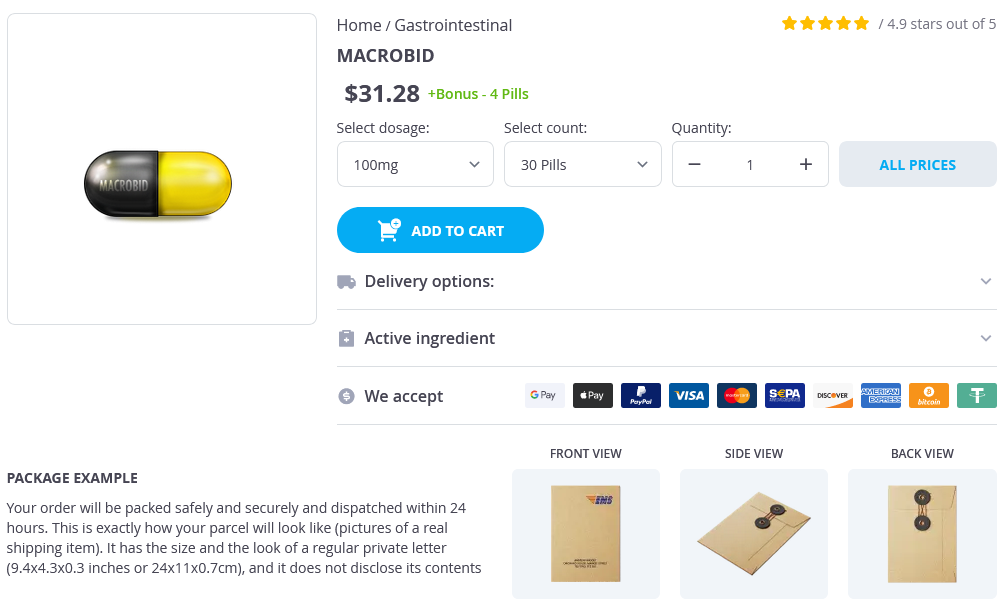
Macrobid Dosage and Price
Macrobid 100mg
- 30 pills - $34.76
- 60 pills - $58.49
- 90 pills - $80.29
- 120 pills - $80.19
- 180 pills - $125.19
- 360 pills - $214.49
Macrobid 50mg
- 120 pills - $118.99
- 180 pills - $157.99
- 360 pills - $305.99
The posterior meningeal branch arises from the vertebral artery above the level of C1 gastritis empty stomach generic macrobid 100mg online, and below the foramen magnum, and supplies the falx cerebelli and the medial portion of the dura of the occipital posterior fossa. Just before joining to form the basilar artery, each of the vertebral arteries give off a branch that will become the anterior spinal artery, which extend downward and medially to join in the midline with a corresponding branch from the other vertebral artery. The posterior spinal arteries can originate from the posterior inferior cerebellar arteries or from the intracranial portion of the vertebral arteries. Spinal Arteries the spinal cord circulation is derived from segmental branches off of the vertebral arteries, as well as multiple radicular arteries arising from segmental vessels. These segmental vessels include the descending cervical, deep cervical, intercostal, lumbar, and sacral arteries. The anterior spinal artery arises at the junction of the intradural segment of the vertebral arteries, caudal to the basilar artery. The anterior spinal artery descends in the midline without interruption from the foramen magnum to the filum terminale. The segmental feeders give rise to sulcal, or central branches, which supply the anterior 2/3 of the cord. The anterior 2/3 includes the anterior horns, spinothalamic tracts, and corticospinal tracts. The anterior spinal artery lies in the midline on a ventral aspect of the cord, in the groove of the anterior median fissure. The posterior spinal arteries arise from the posterior rami of the vertebral artery or from the posterior inferior cerebellar artery. The posterior spinal arteries are a paired longitudinal system of vessels on the dorsal cord medial to the dorsal roots. The posterior spinal artery supplies the posterior 1/3 of the cord, which includes supply to the posterior columns and a variable supply to the corticospinal tracts. Continuation of both the anterior and posterior spinal artery supply is derived from segmental anastomoses. These segmental vessels arise as dorsal rami from vertebral, subclavian, thoracic intercostal, and lumbar intercostal arteries. The dorsal rami enter the canal through the neural foramen and then penetrate the dura and divide into 2 main branches: the dural artery, which supplies the nerve root sleeve and the dura, and the radiculomedullary branch. The radiculomedullary branch then divides into a radicular artery, which penetrates the subarachnoid space to supply the anterior and posterior roots. There is also a variable medullary artery branch, which joins the anterior spinal artery and posterior spinal artery. The radicular arteries arise from the division of the radiculomedullary arteries along the anterior and posterior nerve roots. The anterior radicular artery extends along the anterior surface of the spinal cord, whereas the posterior radicular artery likewise extends along the posterior cord surface. The multiple fetal segmental vessels will regress with adulthood, leaving 2-14 (average 6) anterior radicular arteries persisting in the adult and 11-16 posterior radicular arteries in the adult. The major cervical radicular feeders to the spinal cord occur between the C5-C7 levels. There are 2-3 anterior cervical cord feeders that measure 400-600 microns in size. There are also 3-4 posterior cervical cord feeders, which are smaller in size, on the order of 150-400 microns. In the thoracic spine, there are 2-3 anterior thoracic cord feeding segmental vessels. Small ventral feeding 431 Vascular Anatomy Spine: Neoplasms, Cysts, and Other Masses vessels may also be present on the order of 200 microns. There is an inverse relationship between the number and caliber of ventral radicular vessels. There can occur "paucisegmental" anatomy with fewer vessels (< 5) with larger caliber or "pluri-segmental" anatomy with more vessels with smaller caliber. The dominant thoracic anterior radicular artery is also called the artery of Adamkiewicz. The artery of Adamkiewicz tends to have a left-sided origin (73%) and arises from T9-T12 (62%), with less common origins in the lumbar region (26%) and from T6-T8 (12%). A major segmental feeder may also occur in the upper thoracic spine, often the T5 level. The number of posterior thoracic cord feeding vessels varies from 9-12, with an average of 8. The lumbosacral and pelvic regions have from 0-1 major feeding vessels to the spinal cord. The anterior spinal artery ends at the conus with communicating branches (rami cruciantes) to the posterior spinal artery. The posterior division of the iliac artery gives rise to the inferior and superior lateral sacral branches, which give rise to the spinal arteries via the anterior sacral foramen. The anterior division of the iliac artery gives rise to the inferior gluteal artery, which supplies the sciatic nerve. The posterior division of the internal iliac artery gives rise to the iliolumbar artery, which supplies the femoral nerve at the iliac wing level. There is a very symmetrical pattern of venous drainage (compared with the highly asymmetrical arterial supply) with minimal anterior-to-posterior, right-to-left segmental variation. There are 2 sets of intrinsic radial draining veins, which drain into the anastomoses on the cord surface. The central group of veins provides for return of the anterior horns and surrounding white matter and drain into the central veins in the anterior median fissure. Peripheral dorsal and lateral cord drainage is via small valveless radial vein plexus, which extends to the coronal venous plexus on the cord surface and then drains to the epidural venous plexus of Batson. The epidural plexus consists of anterior and posterior internal vertebral plexus components and connects with the superior and inferior vena cava, azygos and hemiazygos systems, and the intracranial dural sinuses.
© 2025 Adrive Pharma, All Rights Reserved..