General Information about Lotrisone
Fungal infections can occur nearly wherever on the physique, from the scalp, ft, and nails, to the groin, hands, and even the within of the mouth. They may be caused by quite a lot of fungi, together with dermatophytes, yeasts, and molds. These infections can usually be troublesome to deal with, and if left untreated, can lead to severe problems. Thankfully, Lotrisone is right here to assist.
Lotrisone is a popular antifungal medication that has been widely used for treating pores and skin infections caused by varied kinds of fungi. The active components in Lotrisone, betamethasone and clotrimazole, work together to inhibit the expansion of fungi, offering relief from signs and serving to to clear up the infection. This powerful mixture makes Lotrisone extremely efficient in treating a variety of fungal pores and skin infections, and it is strongly recommended by doctors and pharmacists alike.
In addition to its effectiveness in treating fungal pores and skin infections, Lotrisone can be known for its ease of use. It may be applied on to the affected area, and solely needs to be used once or twice a day, depending on the severity of the an infection. Lotrisone additionally is available in convenient, transportable packaging, making it simple to take with you wherever you go.
In conclusion, Lotrisone is a safe, efficient, and convenient remedy for fungal skin infections. Its mixture of betamethasone and clotrimazole makes it a robust weapon in opposition to quite so much of fungi, providing quick relief from signs and selling therapeutic. However, it is important to notice that Lotrisone just isn't recommended to be used in children underneath the age of 17, or pregnant or lactating girls, until particularly instructed by a doctor. If you may be experiencing signs of a fungal pores and skin an infection, seek the guidance of your doctor or pharmacist to see if Lotrisone is the proper remedy for you.
Lotrisone has been proven to be extremely efficient in treating quite so much of fungal pores and skin infections, similar to athlete's foot, jock itch, ringworm, and yeast infections. It works by attacking the root reason for the infection, offering quick reduction from signs and preventing the an infection from spreading. This not solely helps to alleviate discomfort but in addition hastens the therapeutic process and reduces the chance of issues.
The two lively ingredients in Lotrisone, betamethasone and clotrimazole, work in different methods to treat fungal infections. Betamethasone is a type of corticosteroid that helps to minimize back inflammation and alleviate symptoms corresponding to redness, swelling, and itching. Clotrimazole, however, is an antifungal agent that works by inhibiting the expansion of fungi, preventing them from reproducing and spreading. Together, these two ingredients work to offer fast-acting reduction and remove the supply of the infection.
Another advantage of Lotrisone is that it's comparatively protected to use. Side results similar to itching, burning, or stinging at the web site of utility are uncommon, and severe allergic reactions are very uncommon. However, as with every treatment, it may be very important observe the instructions fastidiously and solely use Lotrisone as directed by a physician or pharmacist.
One of one of the best things about Lotrisone is that it is obtainable in different varieties, together with cream and lotion, making it suitable for quite so much of skin varieties and situations. Lotrisone cream is normally used to deal with infections that occur between the toes, while the lotion is extra suited for treating infections on larger skin surfaces. This versatility makes it a well-liked selection among both patients and healthcare professionals.
Although there is a genetic factor in the development of the disease xen fungus order 10 mg lotrisone, the insulin deficit results from destruction of the pancreatic beta cells in an autoimmune reaction, resulting in an absolute deficit of insulin in the body and therefore requiring replacement therapy. The amount of insulin required is equivalent to the metabolic needs of the body based on dietary intake and metabolic activity. Acute complications such as hypoglycemia or ketoacidosis are more likely to occur in this group. About 1 in every 400 to 500 children has Type 1 diabetes; Type 1 diabetes occurs in approximately 10% of all individuals diagnosed with diabetes. This abnormality may involve decreased pancreatic beta cell production of insulin, increased resistance by body cells to insulin, increased production of glucose by the liver, or a combination of these factors. This form of diabetes may be controlled by adjusting the need for insulin by: Regulating dietary intake Increase use of glucose, such as with exercise Reducing insulin resistance Stimulating the beta cells of the pancreas to produce more insulin Type 2 is a milder form of diabetes, often developing gradually in older adults, the majority of whom are overweight. However, there has been an increased incidence in adolescents and younger adults who are identified with metabolic syndrome, a complex of several pathophysiologic conditions marked by obesity, cardiovascular changes, and significant insulin resistance due increased adipose tissue (see Chapter 8). Individuals with metabolic syndrome often have developed vascular or other chronic complications before diagnosis. A major concern at this time is the rapid climb in incidence of Type 2 diabetes, with prevalence now estimated at about 9% (18 million) of the population greater than 20 years of age. With increasing obesity seen in the population, it is anticipated that the future incidence will increase significantly. Also, it is thought that there may be one undiagnosed case for every two to three diagnosed cases. Prevalence of Type 2 diabetes increases with age, with approximately half the cases found in persons greater than 55 years of age. There is a higher prevalence in African Americans, Hispanic Americans, and Native Americans. Gestational diabetes may develop during pregnancy and disappear after delivery of the child (see Chapter 9). Approximately 5% to 10% of women who have gestational diabetes develop Type 2 diabetes some years later. A number of other types of diabetes and glucose intolerance vary in cause and severity. Insulin deficit results in decreased transportation and use of glucose in many cells of the body. Excess glucose spills in to the urine (glucosuria) as the level of glucose in the filtrate exceeds the capacity of the renal tubular transport limits to reabsorb it. Glucose in the urine exerts osmotic pressure in the filtrate, resulting in a large volume of urine to be excreted (polyuria), with the loss of fluid and electrolytes. Fluid loss through the urine and high blood glucose levels draw water from the cells, resulting in dehydration (see Chapter 6). If the insulin deficit is severe or prolonged, the process continues to develop, resulting in additional consequences, ultimately, diabetic ketoacidosis. Lack of glucose in cells results in catabolism of fats and proteins, leading to excessive amounts of fatty acids and their metabolites, known as ketones or ketoacids, in the blood. Ketones consist of acetone and two organic acids- beta-hydroxybutyric acid and acetoacetic acid. Because the liver and other cells are limited in the amount of lipids, fatty acids, or ketones they can process completely within a given time, excessive amounts of ketones in the blood cause ketoacidosis. The ketoacids bind with bicarbonate buffer in the blood, leading to decreased serum bicarbonate and eventually to a decrease in the pH of body fluids. Signs and symptoms As Type 2 diabetes develops, weight gain or increased abdominal girth is common, whereas in Type 1 weight loss is common. Polyuria is indicated by urinary frequency, which is often noticed by the patient at night (nocturia) with the excretion of large volumes of urine. Typically, the three Ps- polyuria, polydipsia, and polyphagia-herald the onset of diabetes. If the insulin deficit continues, the patient progresses to the stage of diabetic ketoacidosis. Diagnostic tests Fasting blood glucose level, the glucose tolerance test, and the glycosylated hemoglobin test are used to screen people with clinical and subclinical diabetes. There is less emphasis now on the "prediabetic stage" because tissue and organ damage appear to commence at an early stage. At present, a fasting blood sugar equal to or greater than 126 mg/dL, taken on more than one occasion, confirms a diagnosis of diabetes. The test for glycosylated hemoglobin (HbA1c) is used to monitor long-term control (8 to 12 weeks) of blood glucose levels. The acceptable level for HbA1c has been lowered to 7%, and is likely to be lowered again to 6% (normal), so as to reduce the serious long-term effects of hyperglycemia. Patients with diabetes can monitor themselves at home by taking a sample of capillary blood from a finger and checking it with a portable monitoring machine (glucometer). When performed regularly, this self-monitoring test helps reduce the fluctuations in blood glucose levels and therefore the risk of complications. Urine tests for ketones are helpful for those who are predisposed to ketoacidosis. Treatment Maintenance of normal blood glucose levels is important to minimize the complications of diabetes mellitus, both acute and chronic.
When a large palatal flap has been reflected fungus gnats on bonsai lotrisone 10 mg order with visa, maintaining a palatal splint to support the soft tissues for several days prevents hematoma formation and may improve patient comfort. Mandibular premolars are generally approached from the labial surface of the mandible. Care must be taken to preserve the integrity of the mental nerve when the impacted tooth is nearby. When the impacted lower premolar is lingually positioned, it is sometimes useful to identify the tooth through a lingual exposure; a labial flap then may be raised and a small hole placed in the labial surface of the bone to allow the premolar to be pushed through to the lingual. It is widely employed in part because it may be the most useful indicator of the time required for surgery and, perhaps even more important, because it is the system required to classify and code impaction procedures to all commercial insurance carriers. Surprisingly, factors such as the angulation of impaction, the relationship of the tooth to the anterior border of the ramus, and the root morphology may have little influence on the time that surgery requires. Roots can be either conical and fused roots or separate and divergent, with the latter being more difficult to manage. A large follicular sac around the crown of the tooth provides more room for access to the tooth, making it less difficult to extract than one with essentially no space around the crown of the tooth. Another important determinant of difficulty of extraction is the age of the patient. When impacted teeth are removed before age 20 years, the surgery is almost always less difficult to perform. The roots are usually incompletely formed and, thus, less bone removal is required for tooth extraction. There is usually a broader pericoronal space formed by the follicle of the tooth, which provides additional access for tooth extraction without bone removal. Because the roots of the impacted teeth are incompletely formed, they are usually separated from the inferior alveolar nerve. In contradistinction, removal of impacted teeth in patients of older age groups is almost always more difficult. The roots are usually completely formed and are thus longer, which requires more bone removal, and closer to the inferior alveolar canal, which increases the risk of postsurgical anesthesia and paresthesia. The follicular sac almost always degenerates with age, which makes the pericoronal space thinner; as a result, more bone must be removed for access to the crown of the tooth. Finally, there is increasing density and decreasing elasticity in the bone, necessitating greater bone removal to deliver the tooth from its socket. In summary, the degree of difficulty of the surgery to remove an impacted tooth is determined primarily by two major factors: (1) the depth of impaction and type of overlying tissue and (2) the age of the patient. Full bony impactions are always more difficult to remove than are soft tissue impactions, and given two impactions of the same depth, the impaction in the older patient is always more difficult than the one in the younger patient. As a general rule, a more challenging and time-consuming surgical procedure results in a more troublesome and prolonged postoperative recovery. It is more difficult to perform surgery in the older individual, and it is harder for these patients to recover from the surgical procedure. The surgeon pays particular attention to the variety of factors known to make the impaction surgery more or less difficult. A variety of classification systems have been developed to aid in the determination of difficulty. The three most widely used are angulation of the impacted tooth, the relationship of the impacted tooth to the anterior border of the ramus and the second molar, and the depth of the impaction and the type of tissue overlying the impacted tooth. It is generally acknowledged that the mesioangular impaction, which accounts for approximately 45% of all impacted mandibular third molars, is the least difficult to remove. The vertical impaction (40% of all impactions) and the horizontal impaction (10%) are intermediate in difficulty, whereas the distoangular impaction (5%) is the most difficult. The relationship of the impacted tooth to the anterior border of the ramus is a reflection of the amount of room available for the tooth eruption as well as the planned extraction. If the length of the alveolar process anterior to the anterior border of the ramus is sufficient to allow tooth eruption, the tooth is generally less difficult to remove. Conversely, teeth that are essentially buried in the ramus of the mandible are more difficult to remove. The depth of the impaction under the hard and soft tissues is likewise an important consideration in determining the degree of difficulty. If the surgeon requires greater access to remove a deeply impacted tooth, the envelope flap may not be sufficient. The envelope incision is usually associated with fewer complications and tends to heal more rapidly and with less pain than the three-cornered flap. The buccal artery is sometimes encountered when creating the releasing incision; this may be bothersome during the early portion of the surgery. There is more variety in presentation of impacted third molars than in any other condition requiring a dental surgical procedure. Other textbooks describe in detail the techniques for removal of the different types of impactions. Bone must be removed in an atraumatic, aseptic, and nonheat-producing technique, with as little bone removed and damaged as possible. The tooth is then divided in to sections and delivered with elevators, using judicious amounts of force to prevent complications. Finally, the wound must be thoroughly débrided mechanically and by irrigation to provide the best possible healing environment in the postoperative period. A, the envelope incision is most commonly used to reflect the soft tissue of the mandible for removal of an impacted third molar. Posterior extension of the incision should diverge laterally to avoid injury to the lingual nerve.
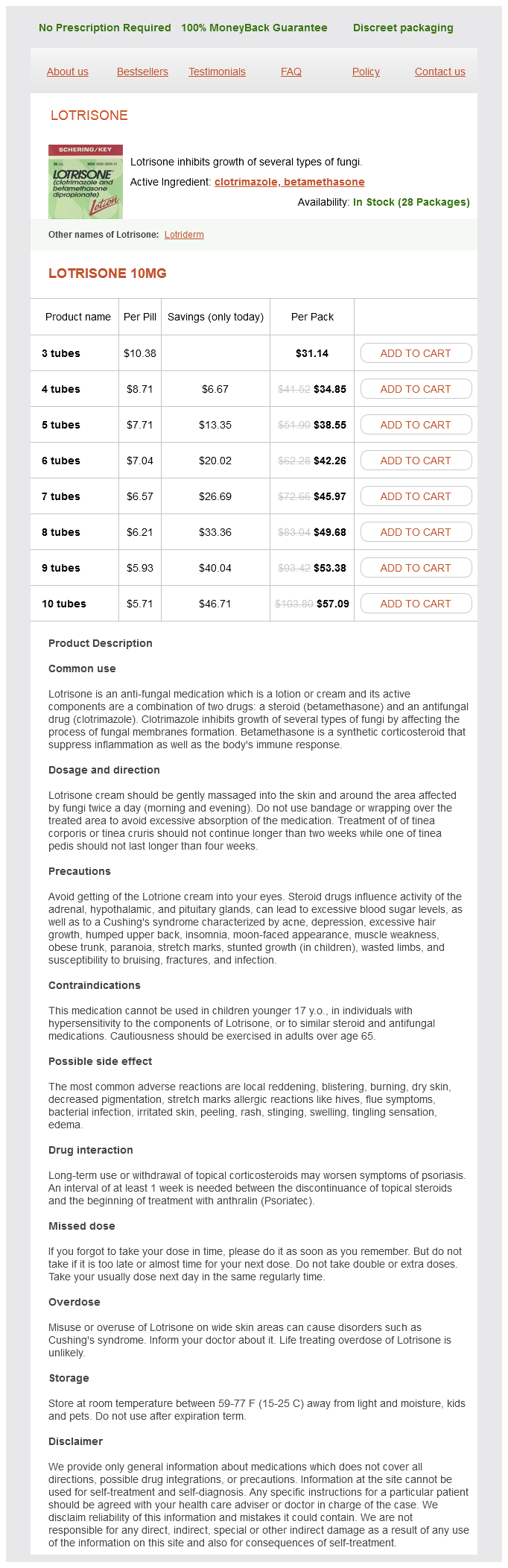
Lotrisone Dosage and Price
Lotrisone 10mg
- 3 tubes - $31.14
- 4 tubes - $34.85
- 5 tubes - $38.55
- 6 tubes - $42.26
- 7 tubes - $45.97
- 8 tubes - $49.68
- 9 tubes - $53.38
- 10 tubes - $57.09
This pain is caused by vigorous contractions of the ureter in an effort to force the stone out fungus gnats tomato plants 10 mg lotrisone order visa. The severe pain may be accompanied by nausea and vomiting, cool moist skin, and rapid pulse. B, Hydronephrosis with dilation of the renal pelvis and calyces and atrophy of renal tissue. Hydronephrosis is frequently asymptomatic unless mild flank pain occurs as the renal capsule is distended, or unless infection develops. If the cause is not removed, bilateral hydronephrosis could lead to chronic renal failure. Renal Cell Carcinoma Renal cell carcinoma (adenocarcinoma of the kidney) is a primary tumor arising from the tubule epithelium, more often in the renal cortex. Approximately 54,000 people in the United States were diagnosed with this cancer in 2008. This tumor tends to be silent; therefore, diagnosis is made in one third of cases after metastasis to lungs, liver, or bone has occurred. Removal of the kidney (nephrectomy) is the treatment because the tumor is usually unresponsive to radiation or chemotherapy. The tumor is invasive through the wall to adjacent structures, and it metastasizes through the blood to pelvic lymph nodes, liver, and bone. Staging categories range from an in situ tumor through the degree of bladder wall invasion to metastasis. Bladder cancer has a high incidence in individuals working with chemicals in laboratories or industry, particularly with dyes, rubber, and aluminum. Other predispos- ing factors are recurrent infection and heavy intake of analgesics. Treatment includes surgical resection of the tumor in 90% of cases, chemotherapy, and radiation. Photoradiation (a combination of drug and laser treatment) has been successful in some early cases. Renal vascular damage Nephrosclerosis Arteriole/arteries Interference with blood flow Atrophy of kidney Fibrosis 1. Such changes reduce the blood supply to the kidney, causing ischemia and atrophy, and also stimulate the secretion of renin, ultimately increasing the blood pressure. Continued ischemia can lead to gradual destruction of renal tissue and chronic renal failure. It is often difficult to determine whether the primary lesion has developed in the kidney or it is secondary to essential hypertension (see Chapter 18), diabetes mellitus (see diabetic nephropathy and. In any case, a vicious cycle can develop with the kidneys and hypertensive changes, and this must be broken to prevent renal failure or other complications of hypertension such as congestive heart failure. Some examples follow: Vesicoureteral reflux is due to a defective valve in the bladder was mentioned under infections. Sometimes it results from fibrosis in the kidney, rather than being a true developmental flaw. There are no indications in the child and young adult; the first manifestations usually appear around age 40 years, when chronic renal failure becomes symptomatic and dialysis is required. This condition is responsible for about 10% of the patients with end-stage chronic renal failure. In some cases, early diagnosis is possible when high blood pressure occurs and is difficult to control or when secondary polycythemia develops due to increased erythropoietin secretion. Multiple cysts develop in both kidneys and gradually expand over the years, first enlarging the kidneys, then compressing and destroying kidney tissue until chronic renal failure occurs. In some cases, cysts are found in other organs such as the liver or cerebral aneurysms are found. Polycystic disease in children is transmitted as a recessive gene and is manifest at birth. However, in this case, the child is either stillborn or dies during the first months. Tumors showing a favorable histology (less aggressive) have an average survival rate of 90%; those with a less favorable pathology (more aggressive) have survival rates ranging from 80% to 40%. Shock associated with burns or crush injuries or sepsis frequently causes renal failure. It is associated with defects in tumor-suppressor genes on chromosome 11 and may occur in conjunction with some other congenital disorders. The gradual loss of nephrons is asymptomatic until it is well advanced because the kidneys normally have considerable reserve function. Once advanced, the progress of chronic renal failure may be slowed but cannot be stopped because the scar tissue and loss of functional organization tend to cause further degenerative changes. The second stage (around 75% nephrons lost), or that of renal insufficiency, is indicated by a change in blood chemistry and manifestations. Tubule function is decreased, resulting in failure to concentrate the urine and control the secretion and exchange of acids and electrolytes. Osmotic diuresis occurs as the remaining functional nephrons filter an increased solute load. This stage is marked by excretion of large volumes of dilute urine (low fixed specific gravity). Fluid, electrolytes, and wastes are retained in the body, and all body systems are affected.
© 2025 Adrive Pharma, All Rights Reserved..