General Information about Loratadine
Claritin isn't really helpful for youngsters beneath 2 years of age, and pregnant or breastfeeding ladies should consult their physician before taking it. In some circumstances, loratadine will not be suitable for people with specific medical circumstances, corresponding to liver illness or kidney issues. It is important to always read the label and follow the instructions to be used.
In conclusion, loratadine, or Claritin, is a generally used antihistamine that gives aid for individuals affected by seasonal allergy symptoms and continual idiopathic urticaria. Its effectiveness and relatively low danger of unwanted facet effects make it a well-liked selection for those looking for relief from allergies and hives. However, it is essential to use it as directed and to consult a healthcare skilled in case you have any issues or questions.
Loratadine is available in several types, together with tablets, liquid, and chewable tablets. It is often taken as soon as a day, and the dosage for adults and children over the age of 6 is 10 mg. For children between the ages of two and 5, the dosage is 5 mg once a day. It is essential to observe the beneficial dosage and to not exceed the day by day limit, as this could result in antagonistic effects.
While loratadine is usually protected and well-tolerated, it might trigger some side effects in some people. These can include dry mouth, headache, drowsiness, and abdomen upset. It is important to note that loratadine might interact with sure medications, so it is essential to seek the assistance of a well being care provider or pharmacist earlier than taking it in case you are already taking different medicines.
One of the principle uses of loratadine is for the reduction of nasal and non-nasal symptoms of seasonal allergic rhinitis, also referred to as hay fever. This situation occurs when the physique's immune system overreacts to allergens, similar to pollen or pet dander. Symptoms can embody sneezing, congestion, runny nose, itching in the nostril and throat, and watery eyes. Claritin works by blocking the results of histamine, reducing these bothersome signs and providing reduction for the person affected by allergy symptoms.
Another use of Claritin is for the therapy of continual idiopathic urticaria, a pores and skin condition characterised by itchy, raised welts on the pores and skin that can appear abruptly and final for a quantity of hours or days. Chronic urticaria, also referred to as hives, is often caused by an allergic reaction to certain foods, medicines, or environmental elements. Loratadine helps to reduce the signs of chronic idiopathic urticaria by blocking the discharge of histamine within the physique.
Loratadine, commonly identified by its model name Claritin, is a popular over-the-counter treatment that is used to alleviate signs of seasonal allergy symptoms and chronic urticaria. It belongs to a category of medication called antihistamines, which work by blocking the motion of histamine, a chemical that is answerable for causing allergy signs such as sneezing, itching, and watery eyes.
This snail-shaped structure contains fluid and thousands of microscopic hair cells tuned to various frequencies allergy forecast madison wi purchase genuine loratadine on line, in addition to the organ of Corti (the receptor for hearing). Conductive hearing loss-A type of medically treatable hearing loss in which the inner ear is usually normal but there are specific problems in the middle or outer ears that prevent sound from getting to the inner ear in a normal way. Vertigo-A feeling of dizziness together with a sensation of movement and a feeling of rotating in space. Turkington Staphylococcal infections Definition Staphylococcal (staph) infections are communicable infections caused by a staphylococcal bacteria. Staphlococcal infections are the leading cause of primary infections originating in hospitals (nosocomial infections) in the United States. It is sometimes found in breast tissue, the mouth, and the genital, urinary, and upper respiratory tracts. Infection is most apt to occur in: Severe dizziness or vertigo may be a signal that there has been an incomplete seal between the fluids of the middle and inner ear. If this is the case, the patient needs immediate bed rest, an exam by the ear surgeon, and (rarely) an operation to reopen the eardrum to check the prosthesis. Results Most patients are slightly dizzy for the first day or two after surgery and may have a slight headache. Hearing improves once the swelling subsides, the slight bleeding behind the ear drum dries up, and the packing is absorbed or removed, usually within two weeks. About 90% of patients will have a completely successful surgery, with markedly improved hearing. About half the patients who had ringing in the ears (tinnitus) before surgery will have significant relief within six weeks after the procedure. A localized staph infection is confined to a ring of dead and dying white blood cells and bacteria. Most of these abscesses eventually burst and pus that leaks onto the skin can cause new infections. A small fraction of localized staph infections enter the bloodstream and spread through the body. In children, these systemic (affecting the whole body) or disseminated infections frequently affect the ends of the long bones of the arms or legs, causing a bone infection called osteomyelitis. When adults develop invasive staph infections, bacteria are most apt to cause abscesses of the brain, heart, kidneys, liver, lungs, or spleen. Staphylococcus aureus Named for the golden color of the bacteria grown under laboratory conditions, S. About 7090% of the population carry this strain of staph in the nostrils at some point in their life. Although present on the skin of only 520% of healthy people, as many as 40% carry the bacteria elsewhere, such as in the throat, vagina, or rectum. These people may carry the bacteria for varying periods of time (from hours to years) without developing symptoms or becoming ill. Boils and inflammation of the skin surrounding a hair shaft (folliculitis) are the most common. Inadequate blood flow to peripheral parts of the body (shock) and loss of consciousness occur within the first 48 hours. Between the third and seventh day of illness, skin peels from the palms of the hands, soles of the feet, and other parts of the body. Rare in adults and most common in newborns and other children under the age of five, scalded skin syndrome originates with a localized skin infection. A mild fever and/or an increase in the number of infection-fighting white blood cells may occur. A bright red rash spreads from the face to other parts of the body and eventually forms scales. Staph bacteria often enter the body through inflamed hair follicles or oil glands. Or they penetrate skin damaged by burns, cuts and scrapes, infection, insect bites, or wounds. Multiplying beneath the skin, bacteria infect and destroy tissue in the area where they entered the body. Staph infection of the blood (staphylococcal bacteremia) develops when bacteria from a local infection infiltrate the lymph glands and bloodstream. These infections, which can usually be traced to contaminated catheters or intravenous devices, usually cause persistent high fever. The primary cause of bacteremia in hospital patients, this strain of staph is most likely to infect cancer patients, whose immune systems have been compromised, and high-risk newborns receiving intravenous supplements. Prosthetic valve endocarditis is endocarditis as a complication of the implantation of an artificial valve in the heart. Although contamination usually occurs during surgery, symptoms of infection may not become evident until a year after the operation. Existing within and around the tube-like structure that carries urine from the bladder (urethra) of about 5% of healthy males and females, S. This strain of staph is responsible for 1020% of infections affecting healthy outpatients. Usually a sign that infection has spread, this condition may be accompanied by fever, chills, and red streaks radiating from the site of the original infection. Diagnosis Blood tests that show unusually high concentrations of white blood cells can suggest staph infection, but diagnosis is based on laboratory analysis of material removed from pus-filled sores, and on analysis of 4779 Staphylococcal infections normally uninfected body fluids, such as, blood and urine. Also, x rays can enable doctors to locate internal abscesses and estimate the severity of infection. Needle biopsy (removing tissue with a needle, then examining it under a microscope) may be used to assess bone involvement. Treatment Superficial staph infections can generally be cured by keeping the area clean, using soaps that leave a germ-killing film on the skin, and applying warm, moist compresses to the affected area for 2030 minutes three or four times a day.
If performed through an abdominal incision allergy treatment options cheap 10 mg loratadine, salpingo-oophorectomy is major surgery that requires three to six weeks for full recovery. There may be some discomfort around the incision for the first few days after surgery, but most women are walking around by the third day. Within a month or so, patients can gradually resume normal activities such as driving, exercising, and working. Immediately following the operation, the patient should avoid sharply flexing the thighs or the knees. Persistent back pain or bloody or scanty urine indicates that a ureter may have been injured during surgery. If both ovaries are removed in a premenopausal woman as part of the operation, the sudden loss of estrogen will trigger an abrupt premature menopause that may involve severe symptoms of hot flashes, vaginal dryness, painful intercourse, and loss of sex drive. Women who have had their ovaries removed are seven times more likely to develop coronary heart disease and much more likely to develop bone problems at an early age than are premenopausal women whose ovaries are intact. If the procedure is performed through a laparoscope, the surgeon can avoid a large abdominal incision and can shorten recovery. With this technique, the surgeon makes a small cut through the abdominal wall just below the navel. A tube containing a tiny lens and light source (a laparoscope) is then inserted through the incision. A camera can be attached that allows the surgeon to see the abdominal cavity on a video monitor. When the ovaries and fallopian tubes are detached, they are removed though a small incision at the top of the vagina. When the laparoscope is used, the patient can be given either regional or general anesthesia; if there are no complications, the patient can leave the hospital in a day or two. If a laparoscope is not used, the surgery involves an incision 46 in (1015 cm) long into the abdomen extending either vertically up from the pubic bone toward the navel, or horizontally (the 'bikini incision') across the pubic hairline. The scar from a bikini incision is less noticeable, but some surgeons prefer the vertical incision because it provides greater visibility while operating. A disadvantage to abdominal salpingo-oophorectomy is that bleeding is more likely to be a complication of this type of operation. Women who have had many gynecological surgeries or chronic pelvic pain seem to have a higher tendency to develop psychological problems after the surgery. Salpingo-oophorectomy Risks Major surgery always involves some risk, including infection, reactions to the anesthesia, hemorrhage, and scars at the incision site. Almost all pelvic surgery causes some internal scars, which in some cases can cause discomfort years after surgery. Potential complications after a salpingo-oophorectomy include changes in sex drive, hot flashes, and other symptoms of menopause if both ovaries are removed. Women who have both ovaries removed and who do not take estrogen replacement therapy run an increased risk for cardiovascular disease and osteoporosis. Women with a history of psychological and emotional problems before an oophorectomy are more likely to experience psychological difficulties after the operation. Alternatives Depending on the specific condition that warrants an oophorectomy, it may be possible to modify the surgery so at least a portion of one ovary remains, allowing the woman to avoid early menopause. In the case of endometriosis, there are a number of alternative treatments that are usually pursued before a salpingo-oophorectomy (with or without hysterectomy) is performed. These include excising the growths without removing any organs, blocking or destroying the nerves that provide sensation to some of the pelvic structures, or prescribing drugs that decrease estrogen levels. Morbidity and mortality rates Studies have shown that the complication rate following salpingo-oophorectomy is essentially the same as that following hysterectomy. The risk of death is about one in every 1,000 (1/1,000) women having a hysterectomy. It is called a syndrome because it is a constellation of symptoms that form a recognizable pattern, as distinct from a clinically well-defined disease. The syndrome may have a slight female preponderance, but the male/female ratio is not known for certain; one rheumatologist in Missouri reported on a series of three patients, all diagnosed within a 12-month period, which included a 17-yearold male, a 59-year-old female, and a 77-year-old male. The most common location of the pain is the front of the chest where the sternum (breastbone) joins the ribs and the clavicles (collarbones); however, the pain may also affect the jaw, in particular the temporomandibular joint. Children are more likely to experience pain in the long bones of the legs, and both children and adults may experience arthritis-like pain in the thoracic region of the spine or in the lower back where the spine joins the hips. While there is no universal definition of the number of persons required to have a disease before it is considered rare-with researchers offering figures ranging from one person in every 1,000 to one in every 200,000-the Rare Diseases Act of 2002 defined a rare disease in the United States as one that affects fewer than one person in every 1,500 or fewer than 200,000 for the country as a whole. Typical findings are hyperostosis of the bone in the anterior chest wall (6590%) of patients; a combination of bone loss (osteolysis) and increased bone density (osteosclerosis) in the spine and sacroiliac joints; swelling (edema) of the bone marrow; and arthritic lesions in the peripheral joints of the body (92% of patients). Some rheumatologists recommend both oral and intravenous bisphosphonates as first-line treatment for the bone loss found in some patients as well as for the bone pain. Tumor necrosis factor inhibitors and azithromycin are effective in treating both the dermatologic and rheumatologic symptoms in some patients. Patients with severe involvement of the spinal column or the long bones may require surgical treatment if medications prove ineffective. The onset of the syndrome is usually insidious, which means that the symptoms appear gradually. Laboratory tests are not useful in the differential diagnosis because the results are often unremarkable.
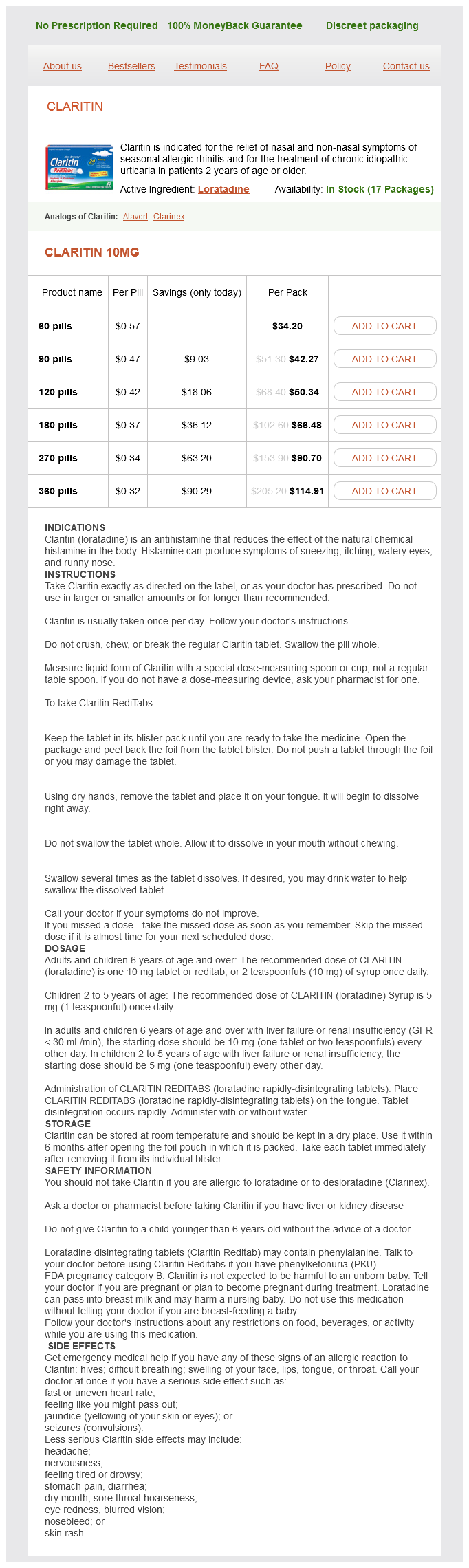
Loratadine Dosage and Price
Claritin 10mg
- 60 pills - $34.20
- 90 pills - $42.27
- 120 pills - $50.34
- 180 pills - $66.48
- 270 pills - $90.70
- 360 pills - $114.91
Bethany Thivierge Tooth replantation Definition Tooth replantation is the reinsertion and splinting of a tooth that has been avulsed (knocked or torn out) of its socket allergy testing asthma buy cheap loratadine 10 mg line. Purpose Teeth are replanted to prevent permanent loss of the tooth, and to restore the landscape of the mouth so that the patient can eat and speak normally. Demographics the patient should see the dentist for an adjustment if there is any discomfort or irritation resulting from a restoration. Otherwise, the patient should see the dentist at least twice a year for an oral examination. According to the National Center for Health Statistics, about five million teeth are accidentally avulsed in the United States each year. Most teeth that are replanted are lost through trauma, usually falls and other types of accidents. The most common trauma resulting in tooth avulsion are sports accidents that result in falls or blows to the head. The mandatory use of mouth guards, which are plastic devices that protect the upper teeth, has prevented approximately 200,000 oral injuries each year in football alone. The American Dental Association recommends the use of mouth guards for any sport that involves speed, contact, or the potential for falls. These categories include not only contact sports like football, wrestling, and boxing, but also gymnastics, baseball, hockey, bicycling, skateboarding, and skiing. Without a mouth guard, a person is 60 times more likely to experience dental trauma if he or she participates in these sports. A very small number of people are allergic to one or more of the metals used in a dental restoration. Results A well-made restoration should feel comfortable and last a relatively long time with proper care. Domestic violence is the most common cause of avulsed teeth in women over the age of 21. Canine tooth-In humans, the tooth located in the mouth next to the second incisor. Endodontist-A dentist who specializes in the diagnosis and treatment of disorders affecting the pulp of a tooth, the root of the tooth, or the tissues surrounding the root. Fibroblasts-Connective tissue cells that help to hold the teeth in their sockets in the jawbone. Mouth guard-A plastic device that protects the upper teeth from injury during athletic events. Description Tooth replantations are performed by general dentists, endodontists, and oral surgeons, usually as office or outpatient procedures. Primary teeth (baby teeth) do not usually have long enough roots for successful replantation. The only exception may be the canine teeth, which have longer roots and a better chance of staying in place. He or she will then reinsert the avulsed tooth in its socket and anchor it within the mouth by installing a splint made of wire and composite resin. Some dentists remove the root canal nerve of the tooth and replace it with a plastic material before reinserting the tooth. Preparation When a tooth is dislodged, it is critical to recover the tooth, preserve it under proper conditions, and get the patient to a dentist immediately. The tooth should be handled carefully; it should be picked up or touched by its crown (the top part of the tooth), not by its root. The use of toothpaste, soap, mouthwash, or other chemicals can remove the fibroblasts clinging to the root of the tooth. Fibroblasts are connective tissue cells that act as a glue between teeth and the underlying bone. The avulsed tooth can be placed in milk or a â special Save-a-Tooth kit, which is a tooth-preserving cup that contains a medium for preserving the fibroblasts around the tooth. The tooth and the patient should go to the dentist within 30 minutes of the accident since fibroblasts begin to die within that time. The dentist should be consulted to determine whether the tooth should be replanted by examining the gums and the emergent tooth. The dentist will take a set of x rays to determine how soon the permanent tooth is likely to emerge. Sometimes an artificial spacer is placed where the primary tooth was lost until the permanent tooth comes in. The dentist may give the patient an antibiotic medication to reduce the risk of infection. The dentist may also take x rays of the mouth to see if there are other injuries to the jawbone or nearby teeth. The patient should avoid rinsing the mouth, spitting, or smoking for the first 24 hours after surgery. Patients with heart disease or disorders of the immune system should be monitored following tooth replantation. Dentists recommend consulting a physician within 48 hours of the dental surgery to determine the risk of tetanus, particularly if the patient has not received a tetanus booster within the past five years. According to the American Association of Endodontists, it takes 23 years after replantation before the dentist can fully evaluate the outcome of treatment. An additional risk is that the root of the tooth may become fused to the underlying bone.
© 2025 Adrive Pharma, All Rights Reserved..