General Information about Lagevrio
Despite its promising outcomes, Lagevrio nonetheless has its limitations. It will not be suitable to be used in patients with severe or important COVID-19, as they might require more intensive remedies. Additionally, the drug isn't recommended to be used in pregnant or lactating girls, in addition to sufferers with severe liver or kidney problems. More research is needed to know the potential side effects and long-term effects of Lagevrio.
One of the major advantages of Lagevrio is its methodology of administration. Being an oral drug, it might be simply taken at home, making it a more convenient option for sufferers than other therapies, such as the monoclonal antibody infusion therapy, which requires patients to go to a healthcare facility to receive the therapy. Additionally, Lagevrio does not must be given early in the center of the infection, as it works at all levels of the disease.
The approval and availability of Lagevrio offers a new software within the fight towards COVID-19. It has the potential to alleviate the burden on hospitals and healthcare techniques by providing a protected and effective remedy choice for non-hospitalized sufferers. However, this does not imply that we must always let our guard down. Vaccines remain the simplest method to forestall severe sickness and dying from COVID-19, and we should proceed to observe public well being tips similar to wearing masks and social distancing.
Since the start of the COVID-19 pandemic, scientists and researchers have been tirelessly working to search out an effective treatment for the virus. One of the newest promising developments is the antiviral drug Lagevrio, also called Lagevrio, which has proven promising leads to its clinical trials.
The efficacy of Lagevrio is not restricted to treating the virus but also has proven potential in stopping the unfold of the virus. Recent research have shown that the drug can cut back the quantity of virus particles in a affected person's saliva, probably reducing their contagiousness and talent to spread the virus to others.
In preclinical research, Lagevrio has shown exercise against a wide range of viruses, together with SARS-CoV-2, the virus answerable for COVID-19. This led to its analysis in a section 2/3 scientific trial, which enrolled over 1,seven hundred non-hospitalized adult sufferers with gentle to reasonable COVID-19 signs. The examine confirmed that Lagevrio reduced the chance of hospitalization or death by roughly 50% compared to placebo.
In the face of a worldwide pandemic, the event of Lagevrio is a significant achievement. It is only one of many ongoing efforts to find efficient treatments for COVID-19. The approval of Lagevrio highlights the significance of research and collaboration in overcoming the challenges posed by the virus. Hopefully, with continued efforts and developments, we will soon be succesful of put an end to this pandemic.
These promising results prompted Merck to request emergency use authorization from the united states Food and Drug Administration (FDA). In October 2021, the FDA granted emergency use authorization for Lagevrio for the therapy of mild to reasonable COVID-19 in adults who are at excessive danger for extreme disease or hospitalization. This authorization marks a big step ahead in the battle in opposition to COVID-19, as it is the first oral antiviral drug permitted for use in treating the virus.
Lagevrio is an oral antiviral drug developed by the pharmaceutical company Merck & Co. It was originally created to treat one other viral an infection, influenza, however has now been repurposed for COVID-19. The drug works by inhibiting the replication of the virus, stopping it from spreading and causing more harm to the body.
Transient small-bowel obstruction or ileus has been noted in up to 8% of patients with ileostomies anti smoking viral video order discount lagevrio online. Data from a 30-year surveillance program in the United Kingdom calculated the risk of colorectal cancer to be 7. Annual or biennial colonoscopy with multiple biopsies is recommended for patients with >810 years of extensive colitis (greater than one-third of the colon involved) or 1215 years of proctosigmoiditis (less than one-third but more than just the rectum) and has been widely used to screen and survey for subsequent dysplasia and carcinoma. High-definition and high-magnification colonoscopes and dye sprays have increased the rate of dysplasia detection. These symptoms should be improved with defecation and/or have their onset associated with a change in frequency or form of stool. It is frequently episodic and crampy, but it may be superimposed on a background of constant ache. Pain is often exacerbated by eating or emotional stress and improved by passage of flatus or stools. The most common pattern is constipation alternating with diarrhea, usually with one of these symptoms predominating. At first, constipation may be episodic, but eventually it becomes continuous and increasingly intractable to treatment with laxatives. Stools are usually hard with narrowed caliber, possibly reflecting excessive dehydration caused by prolonged colonic retention and spasm. Most patients also experience a sense of incomplete evacuation, thus leading to repeated attempts at defecation in a short time span. Patients whose predominant symptom is constipation may have weeks or months of constipation interrupted with brief periods of diarrhea. Although some patients with these symptoms actually may have a larger amount of gas, quantitative measurements reveal that most patients who complain of increased gas generate no more than a normal amount of intestinal gas. Severity of symptoms varies and can significantly impair quality of life, resulting in high health care costs. Advances in basic, mechanistic, and clinical investigations have improved our understanding of this disorder and its physiologic and psychosocial determinants. Onset associated with a change in form (appearance) of stool a Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis. When patients were grouped according to sensory threshold, hyposensitive individuals had distention significantly more than those with hypersensitivity and this was observed more in the constipation subgroup. Although the prevalence of functional gastrointestinal disorders is stable over time, the turnover in symptom status is high. Many episodes of symptom disappearance are due to subjects changing symptoms rather than total symptom resolution. The frequency of perceptions of food intolerance is at least twofold more common than in the general population. Postprandial pain has been temporally related to entry of the food bolus into the cecum in 74% of patients. Long-term hyperalgesia Tonic cortical regulation Neuroplasticity elsewhere in the body. The mechanisms responsible for visceral hypersensitivity are still under investigation. It has been proposed that these exaggerated responses may be due to (1) increased end-organ sensitivity with recruitment of "silent" nociceptors; (2) spinal hyperexcitability with activation of nitric oxide and possibly other neurotransmitters; (3) endogenous (cortical and brainstem) modulation of caudad nociceptive transmission; and (4) over time, the possible development of longterm hyperalgesia due to development of neuroplasticity, resulting in permanent or semipermanent changes in neural responses to chronic or recurrent visceral stimulation (Table 352-2). Modulation of this region is associated with changes in the subjective unpleasantness of pain. These may represent a form of cerebral dysfunction leading to the increased perception of visceral pain. Abuse is associated with greater pain reporting, psychological distress, and poor health outcome. Patients with mild to moderate symptoms usually have intermittent symptoms that correlate with altered gut physiology. Patients who have severe symptoms usually have constant pain and psychosocial difficulties. These abnormalities may contribute to abnormal epithelial secretion and visceral hypersensitivity. Psychological stress and anxiety can increase the release of proinflammatory cytokine, and this in turn may alter intestinal permeability. This finding, however, has been challenged by a number of other studies that found no increased incidence of bacterial overgrowth based on jejunal aspirate culture. Abnormal H2 breath test can occur because of small-bowel rapid transit and may lead to 1967 erroneous interpretation. A temporary reduction in lactobacilli has been reported in animal models of early-life stress. On the other hand, Firmicutes is the dominant phylum in adults consuming a diet high in animal fat and protein. However, it is still unclear whether such changes in fecal microbiota are causal, consequential, or merely the result of constipation and diarrhea. In addition, the stability of the change in the microbiota needs to be determined. A careful history and physical examination are frequently helpful in establishing the diagnosis. The quality, location, and timing of pain may be helpful to suggest specific disorders.
More commonly encountered are intestinal and colonic ischemia that are consequences of arterial embolus stages hiv infection graph buy generic lagevrio 200 mg on-line, arterial thrombosis, venous thrombosis, or hypoperfusion from dehydration, sepsis, hemorrhage, or reduced cardiac output. In the United States, colorectal cancer is most common and usually presents after age 50 years. Esophageal cancer develops with chronic acid reflux or after an extensive alcohol or tobacco use history. Pancreatic and biliary cancers elicit severe pain, weight loss, and jaundice and have poor prognoses. Hepatocellular carcinoma usually arises in the setting of chronic viral hepatitis or cirrhosis secondary to other causes. These disorders exhibit altered gut motor function; however, the pathogenic relevance of these abnormalities is uncertain. Exaggerated visceral sensory responses to noxious stimulation may cause discomfort in these disorders. Symptoms in other patients result from altered processing of visceral pain sensations in the central nervous system. Family members of inflammatory bowel disease patients show a genetic predisposition to disease development themselves. Visceral pain generally is midline in location and vague in character, whereas parietal pain is localized and precisely described. Common inflammatory diseases with pain include peptic ulcer, appendicitis, diverticulitis, inflammatory bowel disease, and infectious enterocolitis. The most common causes of abdominal pain are irritable bowel syndrome and functional dyspepsia. Heartburn Heartburn, a burning substernal sensation, is reported intermittently by at least 40% of the population. Irritable bowel syndrome produces constipation, diarrhea, or an alternating bowel pattern. Fecal mucus is common in irritable bowel syndrome, whereas pus characterizes inflammatory disease. However, briskly bleeding upper sites can elicit voluminous red rectal bleeding, whereas slowly bleeding ascending colon sites may produce melena. Other etiologies include portal hypertensive causes, malignancy, tears across the gastroesophageal junction, and vascular lesions. Other causes include neoplasm, inflammatory bowel disease, infectious colitis, drug-induced colitis, and other vascular lesions. Posthepatic causes of jaundice include biliary diseases, such as choledocholithiasis, acute cholangitis, primary sclerosing cholangitis, other strictures, and neoplasm, and pancreatic disorders, such as acute and chronic pancreatitis, stricture, and malignancy. Weight loss, anorexia, and fatigue are nonspecific symptoms of neoplastic, inflammatory, gut motility, pancreatic, small-bowel mucosal, and psychiatric conditions. In these individuals, validated symptom profiles are used to confidently diagnose a functional bowel disorder. Symptoms of short duration commonly result from acute infection, toxin exposure, or abrupt inflammation or ischemia. Long-standing symptoms point to underlying chronic inflammatory or neoplastic conditions or functional bowel disorders. Symptoms from mechanical obstruction, ischemia, inflammatory bowel disease, and functional bowel disorders are worsened by meals. Ulcer pain occurs at intermittent intervals lasting weeks to months, whereas biliary colic has a sudden onset and lasts up to several hours. Diarrhea from malabsorption usually improves with fasting, whereas secretory diarrhea persists without oral intake. Obstructive symptoms with prior abdominal surgery raise concern for adhesions, whereas loose stools after gastrectomy or gallbladder excision suggest dumping syndrome or postcholecystectomy diarrhea. Celiac disease is prevalent in people of northern European descent, whereas inflammatory bowel disease is more common in certain Jewish populations. When tested against findings of struc- tural investigations, the Rome criteria exhibit diagnostic specificities exceeding 90% for many of the functional bowel disorders. Abnormal vital signs provide diagnostic clues and determine the need for acute intervention. Cardiopulmonary disease may present with abdominal pain or nausea; thus lung and cardiac exams are important. Rectal exam may detect blood, indicating gut mucosal injury or neoplasm or a palpable inflammatory mass in appendicitis. Metabolic conditions and gut motor disorders have associated peripheral neuropathy. Inspection of the abdomen may reveal distention from obstruction, tumor, or ascites or vascular abnormalities with liver disease. Auscultation can detect bruits or friction rubs from vascular disease or hepatic tumors. Loss of bowel sounds signifies ileus, whereas high-pitched, hyperactive sounds characterize intestinal obstruction. Patients with visceral pain may exhibit generalized discomfort, whereas those with parietal pain or peritonitis have directed pain, often with involuntary guarding, rigidity, or rebound. Patients with musculoskeletal abdominal wall pain may note tenderness exacerbated by Valsalva or straight-leg lift maneuvers. Table 344-2 lists the most common indications for the major endoscopic procedures. Upper endoscopy evaluates the esophagus, stomach, and duodenum, whereas colonoscopy assesses the colon and distal ileum. Sigmoidoscopy examines the colon up to the splenic flexure and is currently used to exclude distal colonic inflammation or obstruction in young patients not at significant risk for colon cancer. Radiography/Nuclear Medicine Radiographic tests evaluate diseases of the gut and extraluminal structures.
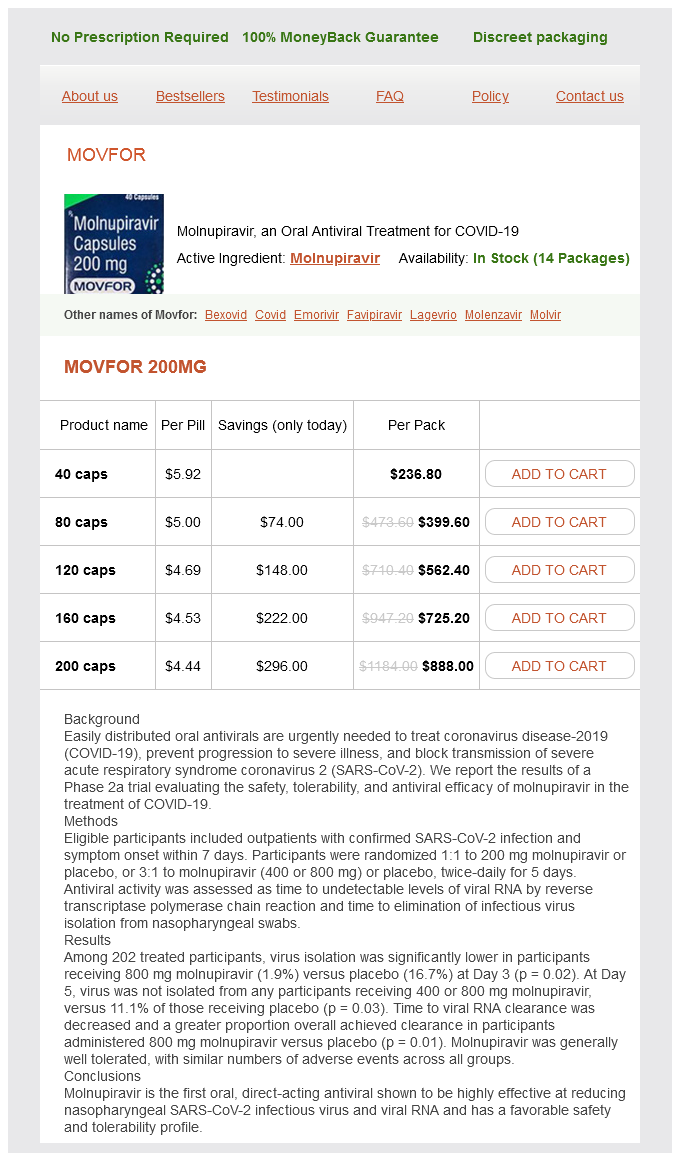
Lagevrio Dosage and Price
Movfor 200mg
- 40 caps - $236.80
- 80 caps - $399.60
- 120 caps - $562.40
- 160 caps - $725.20
- 200 caps - $888.00
Severe inflammation of the ileocecal region may lead to localized wall thinning hiv transmission statistics oral buy lagevrio 200 mg with visa, with microperforation and fistula formation to the adjacent bowel, the skin, or the urinary bladder, or to an abscess cavity in the mesentery. Nutritional deficiencies can also result from poor intake and enteric losses of protein and other nutrients. Intestinal malabsorption can cause anemia, hypoalbuminemia, hypocalcemia, hypomagnesemia, coagulopathy, and hyperoxaluria with nephrolithiasis in patients with an intact colon. Vertebral fractures are caused by a combination of vitamin D deficiency, hypocalcemia, and prolonged glucocorticoid use. Pellagra from niacin deficiency can occur in extensive small-bowel disease, and malabsorption of vitamin B12 can lead to megaloblastic anemia and neurologic symptoms. Levels of minerals such as zinc, selenium, copper, and magnesium are often low in patients with extensive small-bowel inflammation or resections, and these should be repleted as well. Most patients should take a daily multivitamin, calcium, and vitamin D supplements. Diarrhea is characteristic of active disease; its causes include (1) bacterial overgrowth in obstructive stasis or fistulization, (2) bileacid malabsorption due to a diseased or resected terminal ileum, and (3) intestinal inflammation with decreased water absorption and increased secretion of electrolytes. Not all patients with perianal fistula will have endoscopic evidence of colonic inflammation. Colonoscopy allows examination and biopsy of mass lesions or strictures and biopsy of the terminal ileum. Upper endoscopy is useful in diagnosing gastroduodenal involvement in patients with upper tract symptoms. Strictures 4 cm and those at anastomotic sites respond better to endoscopic dilation. Most endoscopists dilate only fibrotic strictures and not those associated with active inflammation. An abdominal x-ray can be taken at around 30 h after ingestion to see if the capsule is still present in the small bowel, which would indicate a stricture. In more advanced disease, strictures, fistulas, inflammatory masses, and abscesses may be detected. As the disease progresses, aphthous ulcers become enlarged, deeper, and occasionally connected to one another, forming longitudinal stellate, serpiginous, and linear ulcers. The radiographic "string sign" represents long areas of circumferential inflammation and fibrosis, resulting in long segments of luminal narrowing. The lack of ionizing radiation is particularly appealing in younger patients and when monitoring response to therapy where serial images will be obtained. Percutaneous drainage has an especially high failure rate in abdominal wall abscesses. Other complications include intestinal obstruction in 40%, massive hemorrhage, malabsorption, and severe perianal disease. There are potential risks of biologic therapies such as infection and malignancy, and it would be optimal to determine at the time of diagnosis which patients will require more aggressive medical therapy. She presented with abdominal pain, distension, vomiting, and small-bowel obstruction. The image reveals a 7- to 10-cm long stricture at the terminal ileum (white arrows) causing obstruction and significant dilatation of the proximal small bowel (white asterisk). He was being treated with 6-mercaptopurine and presented with abdominal distention and diarrhea. Multifocal involvement of the small bowel and terminal ileum is also present (dashed white arrows). In the absence of a key diagnostic test, a combination of features is used (Table 351-5). Shigellosis causes watery diarrhea, abdominal pain, and fever followed by rectal tenesmus and by the passage of blood and mucus per rectum. All three are usually self-limited, but 1% of patients infected with Salmonella become asymptomatic carriers. Yersinia enterocolitica infection occurs mainly in the terminal ileum and causes mucosal ulceration, neutrophil invasion, and thickening of the ileal wall. Distal ileal and cecal involvement predominates, and patients present with symptoms of small-bowel obstruction and a tender abdominal mass. Symptoms include anorectal pain, tenesmus, constipation, inguinal adenopathy, difficulty with urinary voiding, and sacral paresthesias. Diagnosis is made by rectal biopsy with identification of characteristic cellular inclusions and viral culture. Small intestinal biopsies show partial villous atrophy; small bowel bacterial overgrowth and fat malabsorption may also be noted. Colonoscopy reveals focal punctate ulcers with normal intervening mucosa; diagnosis is made by biopsy or serum amebic antibodies. In severely immunocompromised patients, Candida or Aspergillus can be identified in the submucosa. Ischemic bowel disease should be considered in the elderly following abdominal aortic aneurysm repair or when a patient has a hypercoagulable state or a severe cardiac or peripheral vascular disorder. It occurs in persons of all ages and may be caused by impaired evacuation and failure of relaxation of the puborectalis muscle. Single or multiple ulcerations may arise from anal sphincter overactivity, higher intrarectal pressures during defecation, and digital removal of stool. Patients complain of constipation with straining and pass blood and mucus per rectum.
© 2025 Adrive Pharma, All Rights Reserved..