General Information about Kaletra
Kaletra has been a game-changer in the therapy of HIV, because it has significantly lowered the mortality fee related to the disease. Studies have proven that combining this treatment with other antiretroviral drugs can reduce the quantity of HIV in the body to undetectable ranges, which is essential in stopping the development of the disease and the development of AIDS.
In addition to its major use in HIV treatment, Kaletra has additionally shown promising ends in the remedy of different emerging viruses, such as SARS, MERS, and Ebola. This has fueled ongoing analysis into its potential use in addressing new and rising viral outbreaks.
While Kaletra has been successful in managing HIV, it is not a cure for the disease. Patients are suggested to continue taking the medication as prescribed by their doctors and to apply secure intercourse to forestall transmission of the virus.
Kaletra has been a life-changing medicine for millions of people residing with HIV/AIDS, providing them hope for a better high quality of life. Its effectiveness, security, and potential to be used in treating other ailments make it a priceless addition to the arsenal against viral infections. However, you will want to do not forget that prevention is healthier than treatment, and training secure sex, regular testing, and early diagnosis are essential steps within the fight against HIV/AIDS. Let us continue to unfold consciousness and help the development of new and improved therapies for this disease.
Ritonavir and Lopinavir, the two lively components in Kaletra, belong to a category of antiviral medications called protease inhibitors. They work by inhibiting an enzyme called HIV protease, which is liable for the manufacturing of new viral particles. Without this enzyme, the virus can not replicate, thereby preventing the spread of the illness.
Kaletra: A Powerful Combination for Fighting HIV/AIDS
Apart from its effectiveness in treating HIV, Kaletra has also been found to have a favorable security profile. In clinical trials, the commonest unwanted side effects reported had been diarrhea, nausea, and headache, which had been largely gentle and manageable. However, like another medication, it could trigger serious unwanted facet effects in some individuals, similar to liver problems and modifications in heart rhythm. Therefore, it is crucial to consult a healthcare skilled earlier than starting Kaletra and to often monitor for any opposed effects.
The combination of Ritonavir and Lopinavir in Kaletra presents a novel strategy to treating HIV. Ritonavir acts as a booster, growing the levels of Lopinavir within the body, making it more practical in inhibiting the virus. This mixture has been found to be particularly efficient towards HIV strains that have developed resistance to different treatment options.
HIV/AIDS, a global epidemic for over three many years, has claimed countless lives and continues to pose a major menace to public health. However, scientific breakthroughs have led to the event of therapies that may effectively handle the disease and enhance the standard of life for these living with it. One such treatment is Kaletra, a mix of Ritonavir and Lopinavir, two antiviral medicines which were proven to be highly effective in combating HIV/AIDS.
Kaletra, marketed by AbbVie Inc., was first permitted by the U.S. Food and Drug Administration (FDA) in 2000 for the remedy of HIV-1 infection in adults. It is out there in tablet and oral resolution form, and it is typically utilized in mixture with other antiretroviral drugs to form a extremely potent regimen for the administration of HIV.
None of the cases of osteomyelitis occurred in patients who received isotonic solutions xanax medications for anxiety buy kaletra discount. In addition, the safety, ease, and effectiveness of the technique have led to its use in prehospital emergency care. They are capable of accepting large volumes of fluid and rapidly transporting fluid or drugs to the central circulation. The artery pierces the cortex and divides into ascending and descending branches, which further subdivide into arterioles that pierce the endosteal surface of the stratum compactum to become capillaries. The capillaries drain into medullary venous sinusoids throughout the medullary space, which in turn drain into a central venous channel. Crystalloid infusion studies in animals have demonstrated that infusion rates of 10 to 17 mL/min may be achieved with gravity infusion and rates as high as 42 mL/min with pressure infusion. After successful resuscitation, bone marrow blood flow decreased after high-dose epinephrine but was maintained after high-dose vasopressin. Once the patient has been stabilized, percutaneous peripheral or central intravascular access may be achieved. Obtaining venous access can be a difficult task even under the best circumstances. This difficulty is compounded during high-stress situations or low-flow states such as cardiac arrest. Gestational age ranged from 32 to 41 weeks and birth weight ranged from 515 to 4050 g. This may include adult patients with burns, trauma, shock, dehydration, or status epilepticus. In addition to logistic constraints that limit the volume of isotonic crystalloid fluids available to resuscitate injured soldiers, hypotension, environmental and tactical conditions, and the presence of mass casualties can lead to excessive delay in obtaining vascular access. The participants rated no individual device as being significantly better than the others. A complete blood cell count may not be reliable because it reflects the marrow cell count rather than the cell count in the peripheral circulation. Furthermore, the aspirated blood usually clots within seconds, even if placed in a tube that contains heparin. Until more information becomes available, practitioners are encouraged to review the products available and choose those that best meet their needs. These needles are large enough (16 gauge) to be used in older children and adults and are suitable for rapid administration of fluid. Illinois Sternal/Iliac Aspiration Needle the Illinois Sternal/Iliac Aspiration Needle (Monojet, Division of Sherwood Medical, St. Osteoporosis and osteogenesis imperfecta are associated with a high potential for fracture; therefore unless absolutely necessary, the procedure should be avoided when these diagnoses are known. A fractured bone should be avoided because as fluid is infused, it increases intramedullary pressure and forces fluid to extravasate at the fracture site. This may slow the healing process, cause nonunion of the bone, or lead to a compartment syndrome. It has an adjustable plastic sleeve to prevent the needle from penetrating through the opposite bony cortex. However, its long shaft and poorly designed handle make it prone to dislodgement during transport and other procedures. It comes in either 15- or 18-gauge and also features an adjustable plastic sleeve to prevent overpenetration. Once inserted the needle protrudes approximately 2 inches from the skin, which increases the risk for accidental dislodgement. It comes in a variety of sizes from 18- to 14-gauge and can be inserted to a depth of 3 to 4 cm. It has a detachable handle, which reduces the risk of it being dislodged, and a depth marker to help ensure proper placement. It has a threaded shaft that helps secure the needle in the bone and a detachable handle that may be reused with multiple needles. Once the device is positioned against the sternum, additional pressure triggers the release of a hollow needle into the medullary space. The handle is automatically released from the stylet and infusion tubing once the needle has met its preset depth. However, if the device is not carefully stabilized before and during insertion, incorrect placement can easily occur. In addition, there is the potential for operator and patient injury if the device is accidentally triggered or mistargeted. It is lightweight, does not require batteries, and is a self-contained unit designed for a single use and ease of deployment. There were no differences in provider comfort or provider assessed device performance between the two devices. The site of needle insertion is the medial surface at the junction of the medial malleolus and the shaft of the tibia, posterior to the greater saphenous vein. The needle is inserted perpendicular to the long axis of the bone or 10 to 15 degrees cephalad to avoid the growth plate. If chosen, the needle should be inserted 2 to 3 cm above the femoral condyles in the midline and directed cephalad at an angle of 10 to 15 degrees from the vertical. The close proximity of the greater tubercle of the humerus to the heart provides rapid infusion of medication and fluid into the general circulation.
Place an additional three (single) throws and then cut the sutures while leaving 1- to 2-cm tails medicine 666 discount 250 mg kaletra visa. Continue to place additional sutures by further bisecting each segment of the laceration. After the last stitch has been placed, cleanse the area and apply an appropriate dressing. Rotate the needle driver 90 degrees and grasp the short suture end on the opposite side of the laceration. Tighten only enough to approximate the skin edges; avoid overtightening, which may lead to tissue strangulation. To begin the second throw, again place the needle driver parallel to the laceration. Remember to place the needle driver parallel to the wound and pull the long suture end over the driver; this will ensure that all knots tied are square knots. Avoid cutting the ends too short, which may lead to knot unraveling or difficulty during suture removal. The scalpel is used to find an appropriate site; a natural plane often exists at the junction of the epidermis and dermis. A, this child sustained a superficial forehead laceration just through the epidermis. As the laceration was healing, it became red and more noticeable (as do all scars), but eventually faded. The best cosmetic result occurs when the long axis of a wound happens to be parallel to the direction of maximal skin tension; such alignment brings the edges of the wound together. Swelling after an injury creates additional tension within the circle of each suture. Tension can be reduced during wound closure in two ways: undermining of the wound edges and layered closure. The force required to reapproximate the edges of a wound correlates with the subsequent width of the scar. T undermine a wound, o the clinician frees a flap of tissue from its base at a distance from the edge of the wound approximately equal to the width of the gap that the laceration presents at its widest point. The depth of the incision can be modified, depending on the orientation of the laceration to skin tension lines and the laxity of skin in the area. The clinician can also accomplish this technique by spreading scissors in the appropriate tissue plane. Because undermining may harm the underlying blood supply, this technique should be reserved for relatively uncontaminated wounds when no other methods adequately relieve wound tension. Minimizing Tissue Trauma the importance of carefully handling tissue has been emphasized since the early days of surgery. When choosing suture size, the clinician should select the smallest size that will hold the tissues in place. Skin stitches should incorporate no more tissue than is needed to coapt the wound edges with little or no tension. Knots should be tied securely enough to approximate the edges of the wound without blanching or indenting the skin surface. Tie and bury the knot by pulling the sutures in the long axis of the wound as shown. Finally, layered closure provides support to the wound and considerably reduces tension at the skin surface. A "fat stitch" is not necessary because little support is provided by closure of the adipose layer and additional suture material may increase the possibility of infection. Layered closure is not recommended for wounds without tension, those with poor vascularity, and those with a moderate or high risk for infection. One approach is to close the length of this layer in segments by placing the first stitch in the middle of the wound and bisecting each subsequent segment until closure of the layer has been completed. Approximation of a lacerated muscle hastens healing and return of function to the muscle. A, In most situations, the needle should be loaded perpendicular to the needle driver. B, If the wound is narrow, the needle can be grasped at a slightly obtuse, 135-degree angle to the needle driver. Once the suture has been placed on one side of the wound, it can be pulled across the wound to the opposite side (or the edges of the wound pushed together) to determine the matching point on the opposite side. The needle should enter the dermis at the same depth as it exited from the opposite side, pass through the tissue, and exit at the bottom of the wound (or the base of the flap). The edges of the wound can be closely apposed by pulling the two tails of the suture in the same direction along the axis of the wound. Hand and instrument knot-tying techniques are described and illustrated in wound care texts. Slide the blade of the scissors down the tail of the suture until the knot is reached. This technique prevents the scissors from cutting the knot itself and leaves a 3-mm tail, which protects the knot from unraveling. The index finger is placed on the side of the needle holder, where it guides placement of the needle. C, Hold the forceps in your nondominant hand as you would hold a pencil or a dart. Pull the suture across the wound to determine the correct level of dermal entry on the opposite side. Pass the needle downward through the dermis on the opposite side so that it exits at the bottom of the wound. B Start here If the wound has been undermined, the needle enters at the base of the flap and is passed upward through the dermis.
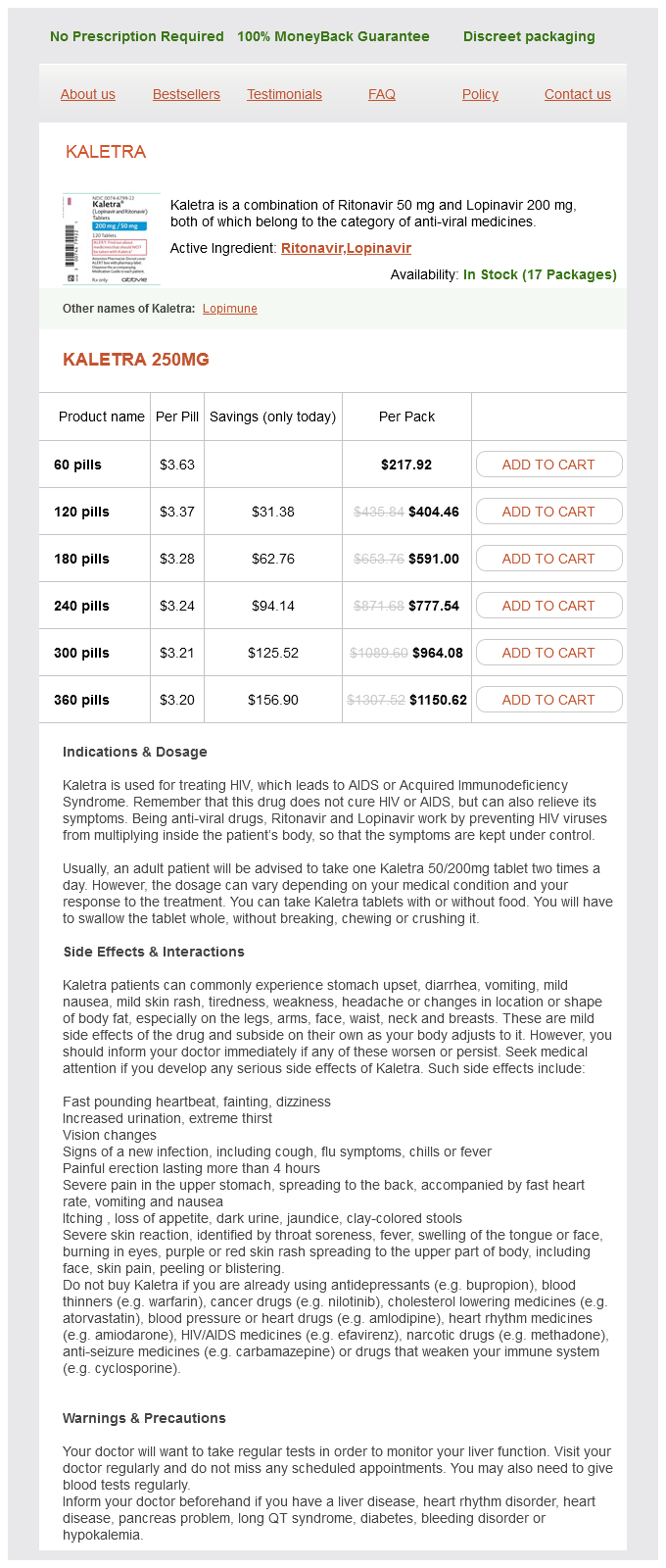
Kaletra Dosage and Price
Kaletra 250mg
- 60 pills - $217.92
- 120 pills - $404.46
- 180 pills - $591.00
- 240 pills - $777.54
- 300 pills - $964.08
- 360 pills - $1150.62
Mortality in patients receiving fewer than 5 units is currently approximately 10% medications band buy kaletra 250 mg with mastercard, in those receiving 6 to 9 units it is approximately 20%, and in those receiving 10 or more units it is greater than 50%. Despite the challenges of treating the expected posttransfusion inflammatory and immunologic complications, patients requiring massive transfusions can have good outcomes. Transfusion Coagulopathy Pathologic hemostasis occurs following massive blood transfusions. Moreover, in patients who are given a transfusion equal to 2 blood volumes, only approximately 10% of the original elements remain. The development of transfusion coagulopathy is multifactorial; important factors include tissue injury, acidosis, the duration of shock, and hypothermia, in addition to activation, consumption, and dilution of coagulation factors. Dilutional thrombocytopenia is a wellrecognized complication of massive transfusion, and a platelet count should be obtained routinely if more than 5 units of blood are transfused. Disseminated intravascular coagulation (from a hemolytic reaction) may play a secondary role in posttransfusion bleeding. Plasma has been used to correct clotting factor abnormalities secondary to dilution from massive transfusions, but its effectiveness has not been firmly established. Cryoprecipitate may be required if fibrinogen levels fall below 100 mg/dL despite the use of plasma. Although blood component therapy can be based on measured coagulopathy parameters, as a general guide 1 to 2 units of plasma for each 5 to 6 units of blood may be given empirically. Traditionally, transfusion-related coagulopathies have been evaluated and treated as per laboratory indicators, but rapid or massive transfusions do not allow equilibration or timely laboratory analysis. Although this approach is quite acceptable in most patients, the aim of transfusion protocols is to prevent transfusion-related coagulopathy before it occurs. In patients with major trauma and severe bleeding they found no significant differences in mortality at 24 hours or 30 days using either strategy. They did note in the 1: 1: 1 group, "more patients achieved hemostasis and fewer experienced death due to exsanguination by 24 hours. Strict adherence to any protocol must be balanced against the risk for multisystem organ failure and infection associated with high doses of platelets and plasma. All protocols recommend warming of blood and blood products because hypothermia occurs quickly during massive transfusions and can contribute to further coagulopathy. Severe Trauma and Coagulopathy A transfusion coagulopathy often develops in individuals who are injured during military combat and receive transfusions because of widespread tissue trauma. Emergency Transfusions In an emergency, three alternatives to fully crossmatched blood exist. Many institutions are now using this procedure as their standard crossmatch for most patients. The safety and utility of the type-specific abbreviated crossmatch have been demonstrated repeatedly, with transfusion reactions occurring only rarely. Type-specific blood that has not been crossmatched has been used in numerous military and civilian series without serious consequences. While the type-specific blood is being transfused, the antibody screen and crossmatch are carried out in the laboratory. A third alternative to fully crossmatched blood is group O blood, although type-specific blood is generally preferable. Thus, despite the theoretical preference for type-specific blood in emergency situations, type O is often a reasonable and practical alternative. One may transfuse both Rh-positive and Rh-negative group O packed cells into patients who are in critical condition. It is a common misconception that patients who are Rh negative will have an immediate transfusion reaction if given Rh-positive blood. There is no particular advantage in determining the Rh factor because preformed, naturally occurring anti-Rh antibodies do not exist. Theoretically, individuals who are Rh negative may become sensitized either through pregnancy or by previous transfusions, and a delayed hemolytic transfusion reaction will result if Rh-positive blood is transfused. However, this scenario is very rare and is of little significance when compared with life-threatening blood loss. Sensitization to the Rh factor is most problematic for Rh-negative women of reproductive age. However, significant subsequent transfusion reactions with Rh-incompatible blood in men sensitized to the Rh factor are very rare. Many advise routine use of the more widely available type O Rh-positive packed cells in all patients in whom the Rh factor has not been determined, except in females of childbearing age, for whom future Rh sensitization may be an important consideration. Once resuscitated with Rh-positive packed cells, patients may receive their own type without a problem. Because individuals with type O Rh-negative blood represent only 15% of the population and the blood may be in short supply, it is reasonable to save type O Rh-negative blood for Rh-negative females of childbearing potential and to use type O Rh-positive packed cells routinely as the first choice for emergency transfusions. In a study of emergency blood needs, Schmidt and colleagues reported 601 units of blood into 262 untyped patients, including 8 Rh-negative women, before the blood type was determined. A nonemergency-based study found the rate of Rh sensitization in Rh-negative recipients receiving Rh-positive blood to be approximately 8% and this figure may be reduced if Rh immune globulin is given after transfusion. Standard doses are 50 µg for women up to 12 weeks of pregnancy and 300 µg in the second and third trimester. In the setting of fetal-maternal transfusion greater than 15 mL (usually only in the third trimester when fetal blood volume becomes more substantial), higher doses may be necessary. Theoretically, citrate salts, which are the usual anticoagulants in donor blood, may combine with ionized calcium in plasma and produce hypocalcemia and rarely hypocalcemic-related cardiovascular depression. In clinical practice the hemodynamic consequences of citrate-induced hypocalcemia are minimal, although the qT interval may be prolonged on the electrocardiogram with citrate infusion.
© 2025 Adrive Pharma, All Rights Reserved..