General Information about Isoniazid
Isoniazid is primarily used for the therapy of tuberculosis, which is a extremely infectious bacterial illness that primarily affects the lungs but also can have an effect on different elements of the body. It is often utilized in combination with other TB drugs such as rifampin, ethambutol, and pyrazinamide to realize maximum effectiveness.
Isoniazid works by killing the micro organism that trigger TB, known as Mycobacterium tuberculosis. It does this by inhibiting a particular bacterial enzyme known as enoyl-acyl provider protein reductase, which is crucial for the micro organism's survival and replication. By blocking this enzyme, the bacteria are unable to supply sure important proteins, resulting in their dying.
Furthermore, Isoniazid can also be used for preventive treatment in individuals who have been uncovered to TB but have not yet developed the infection. This is commonly the case for individuals who repeatedly come in contact with TB sufferers, similar to health care staff. It can additionally be utilized in combination with different medication for the remedy of latent TB infection (LTBI), which signifies that the bacteria are present within the body but not presently lively.
Certain precautions must be taken before beginning Isoniazid therapy. Individuals with liver disease, a historical past of alcoholism, or who are taking other medicines that may affect the liver ought to inform their physician before taking Isoniazid. It can also be essential to tell the physician if you have diabetes, kidney disease, or HIV infection, as these conditions could affect the choice of treatment or dosage.
In conclusion, Isoniazid is a vital medication within the therapy and prevention of tuberculosis. Its effectiveness and relatively low value have made it an important drug for each creating and developed international locations in the fight towards TB. However, it is crucial to seek the guidance of with a health care provider before taking this treatment to make sure its secure and effective use. Along with correct diagnosis and administration, Isoniazid can play a major function in eradicating TB and saving lives.
How does it work?
Side Effects of Isoniazid
What is Isoniazid?
Precautions
Uses of Isoniazid
Furthermore, individuals who are pregnant or breastfeeding should focus on with their doctor in regards to the potential risks and advantages of taking Isoniazid. While this treatment is usually considered secure, warning should be exercised during pregnancy or breastfeeding.
Isoniazid, also called INH, is an antibiotic treatment commonly used for treating or stopping tuberculosis (TB) an infection. This drug has been in use for over 50 years and has been a pivotal component in the treatment of TB. In this text, we will discover what Isoniazid is, the means it works, its uses, side effects, and precautions.
More severe unwanted effects may also occur, though they're much less common. These might embody liver injury and allergic reactions. Signs of liver harm may include yellowing of the skin or eyes, darkish urine, abdomen ache, or unusual tiredness. Individuals should search medical attention immediately if these signs happen. Allergic reactions to Isoniazid may present with problem respiration, swelling of the face, lips, tongue, or throat.
Like another medication, Isoniazid might trigger some unwanted aspect effects in some individuals. The most typical unwanted effects embrace nausea, vomiting, and loss of appetite, which usually subside after a quantity of weeks of treatment. Other side effects might include rash, fever, headache, adjustments in imaginative and prescient, and numbness or tingling in the hands and ft. These side effects should be reported to a health care provider in the event that they turn into bothersome or severe.
Isoniazid is a first-line antibiotic drug used within the treatment of tuberculosis. It was first developed in 1912 however was not broadly used till the Nineteen Fifties. Isoniazid is a half of the class of medicines called antimycobacterials, which are medicine used particularly to treat TB. It is available in varied types, including tablets, injections, and syrups.
Otherwise treatment time will be prolonged medicine 0027 v purchase isoniazid on line, while shock wave generation is suspended, until the stone returns or is retargeted to the treatment focal zone; or if shocks are continued, adjoining tissues may become injured from the energy of the shock waves. Using controlled ventilation during a general anesthetic may cause stone excursion to surpass 60 mm. Spontaneous ventilation has been observed to displace stones over 12 mm, whereas in patients with adequate sedation, stone excursion is limited to approximately 5 mm. The flank area should be kept free of any medium that would provide an interface for the dissipation of shock wave energy. Nephrostomy dressings should be removed, and the nephrostomy catheter should be taped clear of the blast path. Although shock waves pass through most tissues relatively unimpeded, they do cause tissue injury, the extent of which depends on the tissue exposed and the shock wave energy at the tissue level. Hematuria is almost always present at the end of the procedure and results from shock waveinduced endothelial injury to the kidney and ureter. The intricate grounding system of the lithotripter ensures that any current-induced dysrhythmias are unlikely. Even patient-controlled analgesia with alfentanil and a combination of propofol and alfentanil has been used. Newer Generations of Lithotripters Newer generations of lithotripters have no water bath, use fluoroscopy and/or ultrasonography to visualize and target the stone, and tend to use multifunctional tables that allow other procedures, such as cystoscopy and stent placement, to be accomplished without moving the patient off the table. The shock waves are tightly focused; therefore, they cause less pain at the entry site, and intravenous analgesiasedation is the mainstay of anesthesia with these newer lithotripters. Other incidental interventions, such as cystoscopy, stone manipulation, or stent placement, may alter anesthetic requirements. Because these newer lithotripters have a much smaller focal zone for the shock waves, it is essential that adequate analgesia and sedation be provided so that stone excursion with respiration is limited to the focal zone. Contraindications Pregnancy, active urinary tract infection, and untreated bleeding disorders are the major contraindications to lithotripsy. Women of childbearing age must have a pregnancy test that is documented to be negative before lithotripsy. Standard tests of coagulation, such as the platelet count, prothrombin time, and partial thromboplastin time, should be obtained as indicated by medical history. Patients with pacemakers can be treated safely if the pacemaker is pectorally placed and the following precautions are observed. Although most pacemakers located pectorally are at a safe distance from the blast path, some may be damaged. Weber and coworkers175 examined 43 different pacemakers and found that three were affected. Treatment should be started at a low energy level and gradually increased while observing pacemaker function. Orthopedic prostheses, such as hip prostheses and even Harrington rods, are not a problem if they are not in the blast path, which is usually the case. Not only do extremely obese patients present anesthetic challenges related to obesity, but also focusing of the stone may be extremely difficult in the very obese. It is prudent for focusing of the stone to be attempted before administering any anesthetic in this highrisk population. Open Radical Surgery in Urology Radical surgery is the excision of a tumor or diseased organ and possibly adjacent structures, along with their blood supply and lymphatic drainage. These procedures are generally performed for patients with malignant rather than benign disease and may be lengthy with sudden and significant blood loss. Although the trend over the past decades has been from open to laparoscopic or robotic-assisted approaches, there are still cases where major open urologic procedures are indicated. Radical Nephrectomy the most common malignancy of the kidney is renal cell carcinoma, comprising 80% to 85% of all solid renal masses. The procedure involves removal of the kidney, the ipsilateral adrenal gland, perinephric fat, and the surrounding fascia. Respiratory changes include decreases in thoracic compliance, tidal volume, vital capacity, and functional residual capacity. Pneumothorax may occur and can have significant respiratory and hemodynamic consequences intraoperatively. In addition, hepatic encroachment on the vena cava and mediastinal shift may reduce venous return and stroke volume further. Cervical plexus, brachial plexus, and common peroneal neuropathies can occur because of stretch or compression of nerves in the lateral position. In 5% to 10% of patients with renal cell carcinoma, the tumor extends into the renal vein and the inferior vena cava and right atrium. Tumor extension into the inferior vena cava and atrium occurs more frequently with rightsided renal cell carcinoma. Several problems can occur in these patients, ranging from circulatory failure as a result of complete occlusion of the vena cava by tumor to acute pulmonary embolization of tumor fragments during surgery. To operate on these patients safely, the extent of the lesion must be defined preoperatively. Venous obstruction can lead to dilation of the epidural veins and the development of abdominal wall and retroperitoneal collaterals. The emphasis should center on appropriate preoperative preparation, which is possible only when the full extent of the lesion has been defined. Radical cystectomy with urinary diversion is considered one of the most complex urologic procedures and involves removal of the entire bladder, the distal ureters, and lymph nodes, as well as the prostate, and seminal vesicles in men or urethra, adjacent vagina, and uterus in women. For urinary diversion, either an orthotopic neobladder or ileal conduit are commonly created. One large study looking at a data registry in England of 2537 patients with an open radical cystectomy over a 2-year period (2014-2015) reported a median blood loss of 500 to 1000 mL with a transfusion rate of 21.
Patients already on paralytic medications should await the return of neuromuscular function before extubation unless doing so causes undue burden on the patient medicine 2410 purchase isoniazid australia. A child younger than 2 years of age has no concept of death, whereas a 10-yearold child may be interested in the details of the dying process. The decision to forgo treatment with curative intent is generally difficult for families, and prognostication is similarly difficult for providers. In a retrospective survey of parents of deceased children, parents noted that their children suffered "a lot" or "a great deal," mostly from pain, fatigue, and dyspnea. Regional anesthesia has been reported as being of benefit to pediatric patients with pain that is difficult to manage with systemic treatment. Increased access to palliative care and hospice services: opportunities to improve value in health care. In their own words: patients and families define high-quality palliative care in the intensive care unit. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Improving the availability and accessibility of opioids for the treatment of pain: the International Pain Policy Fellowship. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Palliative care consultation for goals of care and future acute care costs: a propensity-matched study. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Comparison of early versus late palliative care consultation in end-of-life care for the hospitalized frail elderly patients. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the center to advance palliative care. Changing end-of-life care practice for liver transplant service patients: structure palliative care intervention in the surgical intensive care unit. Addressing access to palliative care services in the surgical intensive care unit. Palliative and end-of-life care in lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. White paper on standards and norms for hospice and palliative care in Europe: part 1. Development of a prognostic model for six-month mortality in older adults with declining health. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. The palliative triangle: improved patient selection and outcomes associated with palliative operations. A prospective, symptom related, outcomes analysis of 1022 palliative procedures for advanced cancer. Engaging patients, health care professionals, and community members to improve preoperative decision making for older adults facing high-risk surgery. Surgical "buy-in": the contractual relationship between surgeons and patients that influences decisions regarding life-supporting therapy. Surgeons expect patients to buy-in to postoperative life support preoperatively: results of a national survey. A conceptual framework for appropriateness in surgical care: reviewing past approaches and looking ahead to patient-centered shared decision making. The effects of perioperative regional anesthesia and analgesia on cancer recurrence and survival after oncology surgery: a systematic review and meta-analysis. Physical functioning, depression, and preferences for treatment at the end of life: the Johns Hopkins Precursors Study. Study to understand prognoses and preferences for outcomes and risks of treatment. Quality of end-of-life care for patients with advanced cancer in an academic medical center. Physician attitudes regarding advance directives for high-risk surgical patients: a qualitative analysis. Use of advance directives for high-risk operations: a national survey of surgeons. A failing medical educational model: a self-assessment by physicians at all levels of training of ability and comfort to deliver bad news. Outcomes from a national multispecialty palliative care curriculum development project. Teaching palliative care and end-of-life issues: a core curriculum for surgical residents. Surgical intensive care unit clinician estimates of the adequacy of communication regarding patient prognosis. Directly observed patient-physician discussions in palliative and end-of-life care: a systematic review of the literature. Outcomes, preferences for resuscitation, and physician-patient communication among patients with metastatic colorectal cancer. Study to understand prognoses and preferences for outcomes and risks of treatments.
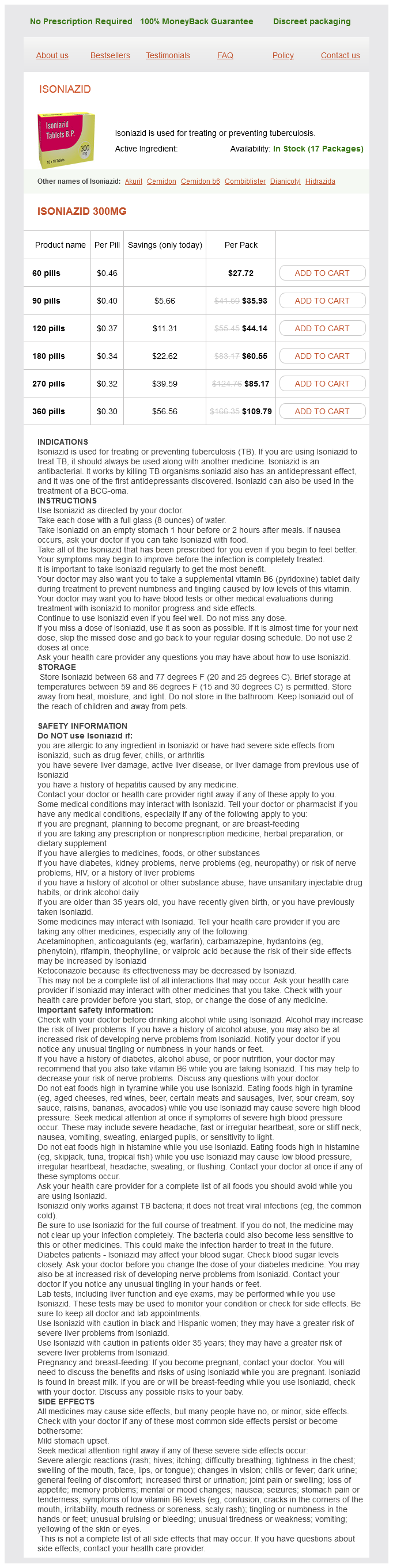
Isoniazid Dosage and Price
Isoniazid 300mg
- 60 pills - $27.72
- 90 pills - $35.93
- 120 pills - $44.14
- 180 pills - $60.55
- 270 pills - $85.17
- 360 pills - $109.79
Intravenous administration of crystalloid or colloid can reduce the degree of hypotension after spinal anesthesia for cesarean delivery symptoms throat cancer order isoniazid 300 mg with mastercard. Of note, fluid co-loading is thought to have limited efficacy in consistently preventing postspinal hypotension and is typically utilized in combination with a vasopressor. Historically, ephedrine was considered the vasopressor of choice to manage hypotension caused by neuraxial anesthesia in pregnancy; however, prophylactic or therapeutic phenylephrine in boluses or as an infusion is not only effective in reducing hypotension but also has less transfer to the fetus and results in less fetal acidosis than ephedrine. There is increasing interest in norepinephrine as an alternative vasopressor for treating spinal hypotension. Compared to phenylephrine, norepinephrine had similar efficacy for maintaining arterial blood pressure during spinal anesthesia for cesarean delivery and was associated with a greater heart rate and cardiac output. Although various local anesthetics can be used for spinal blockade, hyperbaric bupivacaine 10 to 12 mg is frequently used to achieve an adequate (T4) level block. Neither patient height nor weight affect block extension,169 although dosing may require adjustment at extremes of the height spectrum. Lipid soluble opioids (such as fentanyl or sufentanil) may be added to enhance neuraxial blockade by reducing local anesthetic dose and decreasing stimulation from surgical traction of the viscera. Typical epidural local anesthetic volumes required for cesarean delivery range between 10 and 20 mL, depending on whether the epidural is already in use. The administration of epidural local anesthetic should occur in divided doses to ensure that the catheter has not migrated into the intravascular or intrathecal space. Block quality can be improved with addition of epinephrine 1:200,000, fentanyl 50 to 100 g, or sufentanil 10 to 20 g. Epidural clonidine 50 to 100 g can be useful in patients with preexisting chronic pain or severe hypertension if the benefit is judged to outweigh the risk for hypotension, bradycardia, and sedation. Epidural morphine 2 to 5 mg is frequently administered to improve postoperative pain. This technique allows for the rapid onset of a dense reliable block while allowing the block time or height to be extended with use of the epidural catheter. In addition, it allows for a controlled airway, controlled ventilation, and in some scenarios such as massive hemorrhage, improved hemodynamic control and perhaps decreased maternal psychological stress in comparison to neuraxial anesthesia. Appropriate equipment preparation, knowledge of patient comorbidities, airway examination, and familiarity with the difficult airway algorithm are necessary preparation for delivering a safe general anesthetic. Clear, concise communication among all members of the perioperative team is especially critical in urgent or emergent situations to maximize patient safety and minimize procedural complications. A catheter-based technique allows for the ability to titrate the local anesthetic to the proper block height and provide additional local anesthetic administration during the case. For patients who do not already have a catheter in place, this technique may be chosen if the procedure is anticipated to take additional time, or if maternal comorbidities would favor a more gradual, controlled onset of epidural anesthesia. Achieving surgical block conditions takes longer with an epidural than spinal technique but can be rapid enough for use in many urgent situations if already in place and used for maternal analgesia. However, if the airway has not been traumatized, good oxygenation is being well maintained, and there is a high likelihood of success at a third attempt, then a third attempt may be reasonable. This latter course of action may clearly put the fetus at great risk but follows the principle of "Mother comes first. Unanticipated difficult airway in obstetric patients: development of a new algorithm for formative assessment in high-fidelity simulation. A rapid-sequence induction commences with preoxygenation, followed by the application of cricoid pressure and the administration of an intravenous induction drug (typically propofol) and a neuromuscular-blocking drug (typically succinylcholine or rocuronium). For example, although the overall risk of intraoperative awareness is estimated to be 1:19,000 general anesthetics, the awareness risk for cesarean delivery is estimated at 1:670 (1:380-1:1300). Improper monitoring, provider inexperience, emergent situations, and patient obesity all increase patient risk. Care should be taken if used for analgesia and conscious sedation so that repeated dosing does not result in loss of consciousness with an unprotected airway increasing the risk for pulmonary aspiration. Induction of Anesthesia: Intravenously Administered Drugs Premedication with lidocaine or fentanyl is typically avoided in cesarean delivery to limit fetal exposure. In scenarios in which hemodynamic stability is prioritized, such as preeclampsia or heart disease, remifentanil 1 to 2 g/kg or fast-acting antihypertensives such as esmolol or labetalol can be used. Propofol is most commonly used for induction of general anesthesia for cesarean delivery and is able to induce unconsciousness in approximately 45 seconds. Sodium thiopental 4 to 6 mg/kg intravenously is still used in many countries for induction of anesthesia. Unlike propofol and thiopental, etomidate has minimal direct effects on maternal hemodynamics and significant hypertension can occur when etomidate is used without adjuvant premedication in the healthy parturient. Etomidate has higher rates of nausea and vomiting and can increase risk for seizures in patients with decreased seizure threshold. This helps maintain arterial pressure, heart rate, and cardiac output but could result in hypertension in the preeclamptic patient. It is an ideal choice for a pregnant woman in hemodynamic compromise resulting from bleeding. After administration, it is hydrolyzed in the plasma by pseudocholinesterase and only small amounts cross to the fetus because it is highly ionized and poorly lipid soluble. It is undetectable in umbilical cord samples unless larger maternal doses are administered (2-3 mg/kg), and exceedingly high maternal doses (10 mg/kg) are needed to inadvertently create neonatal neuromuscular blockade. Rocuronium may be considered as an alternative to succinylcholine for muscle relaxation. It allows adequate relaxation for endotracheal intubation in less than 60 seconds at intravenous doses of 0. Like succinylcholine, nondepolarizing muscle relaxants do not cross to the fetal circulation in amounts that would cause neonatal weakness. Although cholinesterase inhibitors may be administered to the neonate, treatment is primarily respiratory support until the drug is eliminated. Neonatal elimination of muscle relaxants may take significantly longer than adult elimination.
© 2025 Adrive Pharma, All Rights Reserved..