General Information about Indocin
Additionally, Indocin might interact with other medicines, together with blood thinners, diuretics, and antidepressants. It is important to inform your physician of some other medicines you take to keep away from any potential drug interactions.
Indocin, also identified as indomethacin, is a non-steroidal anti-inflammatory drug (NSAID) that is generally used to reduce fever, stiffness, pain, and swelling. It is commonly used to treat a wide range of circumstances similar to arthritis, gout, bursitis, and tendonitis. As with any medication, you will need to understand the benefits and potential risks related to Indocin before starting therapy.
Furthermore, Indocin can be generally used to treat acute gout assaults. Gout is a sort of arthritis that occurs when too much uric acid builds up in the body, resulting in sudden and extreme attacks of joint ache and irritation. Indocin helps to reduce the ache and swelling attributable to gout, and can be used to forestall future assaults.
In conclusion, Indocin is a helpful NSAID that provides relief from fever, stiffness, pain, and inflammation. It has proven to be efficient in treating a wide range of conditions and is available in varied varieties for convenience. However, like any medicine, it is important to make use of Indocin as directed and to focus on its potential side effects. Consult along with your doctor to find out if Indocin is the proper remedy for you.
One of the major benefits of Indocin is its ability to supply reduction from ache and irritation. It is commonly used to treat situations such as arthritis, which causes continual joint ache and inflammation. Indocin is also effective in reducing ache and stiffness associated with other circumstances similar to bursitis and tendinitis. This makes it a popular selection amongst people coping with these kind of discomfort.
Indocin is available in numerous types corresponding to oral capsules, suppositories, and intravenous injections. The dosage and period of treatment will depend upon the precise situation being treated, as properly as the individual's medical historical past. It is important to observe the recommended dosage and duration of therapy prescribed by your physician to keep away from any potential side effects.
While Indocin has proven to be efficient in providing reduction from numerous situations, you will need to pay consideration to its potential risks and unwanted effects. Like all NSAIDs, Indocin carries a small danger of gastrointestinal unwanted effects such as abdomen ache, nausea, and diarrhea. It can even enhance the risk of cardiovascular occasions, particularly in individuals with a history of coronary heart illness or stroke. Therefore, it is essential to discuss any pre-existing medical conditions together with your physician earlier than starting Indocin.
First and foremost, let's understand how Indocin works. As an NSAID, Indocin works by reducing the manufacturing of prostaglandins, that are chemical substances within the body that trigger inflammation and ache. By blocking the production of prostaglandins, Indocin helps to alleviate the signs of varied situations and promotes a discount in fever.
Recovery was also related to the baseline left ventricular end-diastolic diameter arthritis in dogs natural cures discount 25 mg indocin free shipping. Subsequent Pregnancy From the largest studies on the topic, approximately one third of women with a history of peripartum cardiomyopathy will suffer relapse with worsening of symptoms and deterioration of left ventricular function during another pregnancy (Elkayam, 2014a). The risk of relapse in women with persistent left ventricular dysfunction is substantially higher than in those who have developed normal ventricular function before a subsequent pregnancy (Hilfiker-Kleiner, 2017). But, normalization of left ventricular function does not guarantee an uncomplicated pregnancy, because approximately 20 percent of these women are at risk for deterioration in left ventricular function. Other Cardiomyopathy Types Arrhythmogenic right ventricular dysplasia is a unique cardiomyopathy defined histologically by progressive replacement of right ventricular myocardium with adipose and fibrous tissue. It has an estimated population prevalence of 1 in 5000, predisposes to ventricular tachyarrhythmias, and is a cause of sudden death, particularly in younger individuals (Agir, 2014; Elliott, 2008). The additional risk of pregnancy in women with arrhythmogenic right ventricular cardiomyopathy is unknown, however, based on their systematic review, Krul and coworkers (2011) counsel against pregnancy. This inherited cardiomyopathy is characterized by a ventricular filling pattern in which worsening myocardial stiffness raises ventricular pressure precipitously and allows only a small filling volume (Elliott, 2008). Because of the severe clinical course and poor prognosis in general, pregnancy is not advised (Krul, 2011). Takotsubo cardiomyopathy is a rare form of acute reversible left ventricular apical wall ballooning (Kraft, 2017). Indeed, findings from the Registry on Pregnancy and Cardiac Disease indicate that women with preexisting heart disease who develop preeclampsia have a 30-percent risk of developing heart failure during pregnancy (Ruys, 2014). Moreover, high-output states caused by hemorrhage and acute anemia elevate cardiac workload and magnify the physiological effects of compromised ventricular function. Similarly, infection and sepsis syndrome raise cardiac output and oxygen utilization and depress myocardial function. In many populations, chronic hypertension with superimposed preeclampsia is the most frequent cause of heart failure in pregnancy. In some, mild antecedent undiagnosed hypertension causes covert cardiomyopathy, and when superimposed preeclampsia develops, together they may cause otherwise inexplicable peripartum heart failure. Obesity is a frequent cofactor with chronic hypertension, and it too is associated with ventricular hypertrophy (Kenchaiah, 2002). Diagnosis Congestive heart failure can have a gradual onset or may present as acute "flash" pulmonary edema. Heart failure onset is most likely at the end of the second/beginning of the third trimester and peripartum (Ruys, 2014). Of symptoms, dyspnea is universal and others are orthopnea, palpitations, substernal chest pain, a sudden decline in the ability to complete usual duties, and nocturnal cough. Clinical findings include persistent basilar rales, hemoptysis, progressive edema, tachypnea, and tachycardia (Sheffield, 1999). Acutely, there is usually systolic failure, and echocardiography shows an ejection fraction <0. Coincidental diastolic failure may also be found, depending on the underlying cause (Redfield, 2016). Management Pulmonary edema from heart failure usually responds promptly with diuretic administration to reduce preload. Hypertension is common, and afterload reduction is accomplished with hydralazine or another vasodilator. Because of marked fetal effects, angiotensin-converting enzyme inhibitors are withheld until after delivery. With chronic heart failure, the incidence of associated thromboembolism is high, and thus prophylactic heparin is often recommended. Left ventricular assist devices are now employed more frequently for acute and chronic heart failure treatment. Subacute bacterial endocarditis usually stems from a low-virulence bacterial infection superimposed on an underlying structural lesion. Organisms that cause indolent endocarditis are most often viridans-group streptococci or Staphylococcus or Enterococcus species. Among intravenous drug abusers and those with catheterrelated infections, Staphylococcus aureus predominates. Streptococcus pneumoniae and Neisseria gonorrhoeae may occasionally cause acute, fulminating disease. Others have reported Neisseria sicca and N mucosa, group B streptococcus, and Escherichia coli endocarditis during pregnancy or peripartum (Cox, 1988; Deger, 1992; Kangavari, 2000; Kulas, 2006). Diagnosis and Management Infective endocarditis symptoms vary and often develop insidiously. Fever, often with chills, is seen in 80 to 90 percent of cases, a murmur is heard in up to 85 percent, and anorexia, fatigue, and other constitutional symptoms are common (Karchmer, 2015). Clinical clues are anemia, proteinuria, and manifestations of embolic lesions that include petechiae, focal neurological changes, chest or abdominal pain, and ischemia in an extremity. Symptoms may persist for several weeks before the diagnosis is found, and a high index of suspicion is necessary. Diagnosis is made using the Duke criteria, which include positive blood cultures for typical organisms and evidence of endocardial involvement (Hoen, 2013; Pierce, 2012). Echocardiography may be diagnostic, but lesions <2 mm or those on the tricuspid valve may be missed. Treatment is primarily medical, and ascertainment of the infecting organism and its sensitivities is imperative for antimicrobial selection. Guidelines for appropriate antibiotic treatment are published by professional societies and updated regularly (Habib, 2015; Karchmer, 2015). Recalcitrant bacteremia and heart failure due to valvular dysfunction are but a few reasons that persistent valvular infection may require replacement.
Assume that when examining a first polar body you saw that it had one copy (dyad) of each chromosome but two dyads of chromosome 21 arthritis zehengrundgelenk buy cheap indocin 25 mg on-line. What would you expect to be the chromosomal 21 complement in the secondary oocyte What consequences are likely in the resulting zygote, if the secondary oocyte was fertilized Assume that you were examining a first polar body and noted that it had one copy (dyad) of each chromosome except chromosome 21. What would you expect to be the chromosome 21 complement (only with respect to chromosome 21) in the secondary oocyte What consequences are likely in the resulting zygote if the secondary oocyte was fertilized Kuliev and Verlinsky (2004) state that there was a relatively high number of separation errors at meiosis I. Regarding chromosome 21, what would you expect to be the chromosome 21 complement in the secondary oocyte in which you saw a single chromatid (monad) for chromosome 21 in the first polar body If this secondary oocyte was involved in fertilization, what would be the expected consequences Inheritance is governed by information stored in discrete unit factors called genes. Genes are transmitted from generation to generation on vehicles called chromosomes. Chromosomes, which exist in pairs in diploid organisms, provide the basis of biparental inheritance. During gamete formation, chromosomes are distributed according to postulates first described by Gregor Mendel, based on his nineteenth-century research with the garden pea. Mendelian postulates prescribe that homologous chromosomes segregate from one another and assort independently with other segregating homologs during gamete formation. Genetic ratios, expressed as probabilities, are subject to chance deviation and may be evaluated statistically. The analysis of pedigrees allows predictions concerning the genetic nature of human traits. A 36 lthough inheritance of biological traits has been recognized for thousands of years, the first significant insights into how it takes place only occurred about 150 years ago. In 1866, Gregor Johann Mendel published the results of a series of experiments that would lay the foundation for the formal discipline of genetics. Since then, the ways in which genes, as segments of chromosomes, are transmitted to offspring and control traits have been clarified. Research continued unabated throughout the twentieth century and into the present-indeed, studies in genetics, most recently at the molecular level, have remained at the forefront of biological research since the early 1900s. When Mendel began his studies of inheritance using Pisum sativum, the garden pea, chromosomes and the role and mechanism of meiosis were totally unknown. Nevertheless, he determined that discrete units of inheritance exist and predicted their behavior in the formation of gametes. An excellent student in high school, he studied philosophy for several years afterward and in 1843, taking the name Gregor, was admitted to the Augustinian Monastery of St. In 1849, he was relieved of pastoral duties, and from 1851 to 1853, he attended the University of Vienna, where he studied physics and botany. He returned to Brno in 1854, where he taught physics and natural science for the next 16 years. Mendel received support from the monastery for his studies and research throughout his life. In 1856, Mendel performed his first set of hybridization experiments with the garden pea, launching the research phase of his career. Although he retained his interest in genetics, his new responsibilities demanded most of his time. The local newspaper paid him the following tribute: His death deprives the poor of a benefactor, and mankind at large of a man of the noblest character, one who was a warm friend, a promoter of the natural sciences, and an exemplary priest. Mendel first reported the results of some simple genetic crosses between certain strains of the garden pea in 1865. Mendel showed remarkable insight into the methodology necessary for good experimental biology. The pea plant is self-fertilizing in nature, but it is easy to cross-breed experimentally. For the character stem height, for example, he experimented with the traits tall and dwarf. He selected Character Seed shape Seed color Pod shape round/wrinkled yellow/green full/constricted Contrasting traits F1 results all round all yellow all full F2 results 5474 round 1850 wrinkled 6022 yellow 2001 green 882 full 299 constricted 428 green 152 yellow 705 violet 224 white F2 ratio 2. From local seed merchants, Mendel obtained true-breeding strains, those in which each trait appeared unchanged generation after generation in self-fertilizing plants. In addition to his choice of a suitable organism, he restricted his examination to one or very few pairs of contrasting traits in each experiment. From the analysis of his data, Mendel derived certain postulates that have become the principles of transmission genetics. A monohybrid cross is made by mating true-breeding individuals from two parent strains, each exhibiting one of the two contrasting forms of the character under study. Initially, we examine the first generation of offspring of such a cross, and then we consider the offspring of selfing, that is, of self-fertilization of individuals from this first generation. The original parents constitute the P1, or parental generation; their offspring are the F1, or first filial generation; the individuals resulting from the selfed F1 generation are the F2, or second filial generation; and so on. Unless tall or dwarf plants are crossed together or with another strain, they will undergo self-fertilization and breed true, producing their respective traits generation after generation. However, when Mendel crossed tall plants with dwarf plants, the resulting F1 generation consisted of only tall plants. When members of the F1 generation were selfed, Mendel observed that 787 of 1064 F2 plants were tall, while 277 of 1064 were dwarf. In this particular example, many identical P1 crosses were made and many F1 plants-all tall-were produced. As noted, of the 1064 F2 offspring, 787 were tall and 277 were dwarf-a ratio of approximately 2. For the character of interest, all F1 offspring expressed the same trait exhibited by one of the parents, but in the F2 offspring, an approximate ratio of 3:1 was obtained.
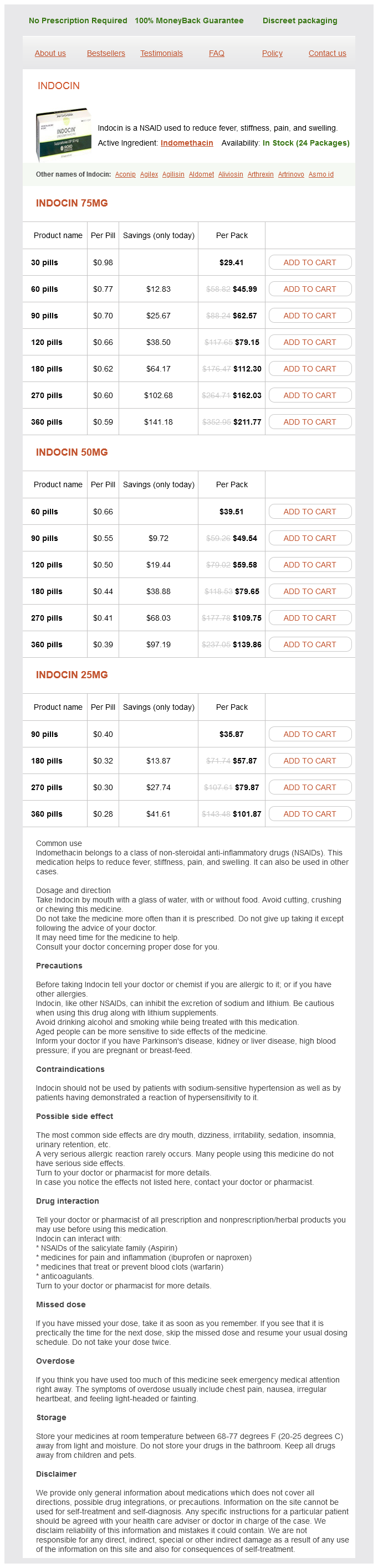
Indocin Dosage and Price
Indocin 75mg
- 30 pills - $29.41
- 60 pills - $45.99
- 90 pills - $62.57
- 120 pills - $79.15
- 180 pills - $112.30
- 270 pills - $162.03
- 360 pills - $211.77
Indocin 50mg
- 60 pills - $39.51
- 90 pills - $49.54
- 120 pills - $59.58
- 180 pills - $79.65
- 270 pills - $109.75
- 360 pills - $139.86
Indocin 25mg
- 90 pills - $35.87
- 180 pills - $57.87
- 270 pills - $79.87
- 360 pills - $101.87
Low risk was defined as no requirement for antithyroid medications during the third trimester or an absence of antithyroid antibodies arthritis paleolithic diet discount indocin 50 mg buy on-line. Seven of these 11 fetuses were determined to be hypothyroid, and the remaining fetuses were hyperthyroid. The American College of Obstetricians and Gynecologists (2017), however, does not recommend such testing. If the fetus is thyrotoxic, maternal thionamide drugs are adjusted even though maternal thyroid function may be within the targeted range (Mestman, 2012). Although usually short-lived, neonatal thyrotoxicosis may require shortcourse antithyroid drug treatment (Levy-Shraga, 2014; Nathan, 2014). A second presentation is goitrous hypothyroidism caused by fetal exposure to maternally administered thionamides. Although there are theoretical neurological implications, reports of adverse fetal effects seem to have been exaggerated. For example, in at least 239 treated thyrotoxic women shown in Table 58-1, evidence of hypothyroidism was found in only four newborns. Furthermore, at least four long-term studies report no abnormal intellectual and physical development of these children (Mestman, 1998). If maternal hypothyroidism developed, the fetus can be treated by a reduced maternal antithyroid medication dose and injections of intraamnionic thyroxine if necessary. And finally, fetal thyrotoxicosis after maternal thyroid gland ablation, usually with 131I radioiodine, may result from transplacental thyroid-stimulating antibodies. In one report of early fetal exposure to radioiodine, neonatal thyroid studies indicated transient hyperthyroidism from maternal transfer of stimulating antibodies (Tran, 2010). Although the fetal thyroid volume can be measured sonographically in women taking thionamide drugs or in those with thyroid-stimulating antibodies, most investigators do not currently recommend this routinely (Cohen, 2003; Luton, 2005). Kilpatrick (2003) recommends umbilical cord blood sampling and fetal antibody testing only if the mother has previously undergone radioiodine ablation. Because fetal hyper- or hypothyroidism may cause hydrops, growth restriction, goiter, or tachycardia, fetal blood sampling may be appropriate if these are identified (Brand, 2005). The Endocrine Society clinical practice guidelines recommend umbilical cord blood sampling only when the diagnosis of fetal thyroid disease cannot be reasonably ascertained based on clinical and sonographic data (Garber, 2012). Thyroid Storm and Heart Failure Both of these are acute and life-threatening in pregnancy. In contrast, pulmonary hypertension and heart failure from cardiomyopathy caused by the profound myocardial effects of thyroxine are common in pregnant women (Sheffield, 2004). As shown in Table 58-2, heart failure developed in 8 percent of 90 women with uncontrolled thyrotoxicosis. In these women, cardiomyopathy is characterized by a high-output state, which may lead to a dilated cardiomyopathy (Fadel, 2000; Klein, 1998). The pregnant woman with thyrotoxicosis has minimal cardiac reserve, and decompensation is usually precipitated by preeclampsia, anemia, sepsis, or a combination of these. Fortunately, thyroxine-induced cardiomyopathy and pulmonary hypertension are frequently reversible (Sheffield, 2004; Siu, 2007; Vydt, 2006). Treatment is similar for thyroid storm and heart failure and should be carried out in an intensive care area that may include special-care units within labor and delivery (American College of Obstetricians and Gynecologists, 2017). An hour or two after initial thionamide administration, iodide is given to inhibit thyroidal release of T3 and T4. With a history of iodine-induced anaphylaxis, lithium carbonate, 300 mg every 6 hours, is given instead. Most authorities recommend dexamethasone, 2 mg intravenously every 6 hours for four doses, to further block peripheral conversion of T4 to T3. If a -blocker drug is given to control tachycardia, its effect on heart failure must be considered. Coexisting severe preeclampsia, infection, or anemia should be aggressively managed before delivery is considered. Hyperemesis Gravidarum and Gestational Transient Thyrotoxicosis Transient biochemical features of hyperthyroidism may be observed in 2 to 15 percent of women in early pregnancy (Fitzpatrick, 2010). Even if associated with hyperemesis, antithyroid drugs are not warranted (American College of Obstetricians and Gynecologists, 2017). Thyrotoxicosis and Gestational Trophoblastic Disease the prevalence of increased thyroxine levels in women with a molar pregnancy ranges between 25 and 65 percent (Hershman, 2004). Because these tumors are now usually diagnosed early, clinically apparent hyperthyroidism has become less common. These biochemically defined extremes usually represent normal biological variations but may herald the earliest stages of thyroid dysfunction. Long-term effects of persistent subclinical thyrotoxicosis include osteoporosis, cardiovascular morbidity, and progression to overt thyrotoxicosis or thyroid failure. Importantly, subclinical hyperthyroidism was not associated with adverse pregnancy outcomes. In separate retrospective analyses of almost 25,000 women who underwent thyroid screening throughout pregnancy, Wilson and colleagues (2012) and Tudela and coworkers (2012) also found no relationship between subclinical hyperthyroidism and preeclampsia or gestational diabetes. Treatment of subclinical hyperthyroidism is unwarranted in pregnancy because antithyroid drugs may affect the fetus. Hypothyroidism Overt or symptomatic hypothyroidism, as shown in Table 58-3, has been reported to complicate between 2 and 12 per 1000 pregnancies. It is characterized by insidious nonspecific clinical findings that include fatigue, constipation, cold intolerance, muscle cramps, and weight gain. A pathologically enlarged thyroid gland depends on the etiology of hypothyroidism and is more likely in women in areas of endemic iodine deficiency or those with Hashimoto thyroiditis. Other findings include edema, dry skin, hair loss, and prolonged relaxation phase of deep tendon reflexes. Autoimmune euthyroid disease represents a new investigative frontier in screening and treatment of thyroid dysfunction during pregnancy.
© 2025 Adrive Pharma, All Rights Reserved..