General Information about Hydrea
In addition to those makes use of, Hydrea is also effective in treating ovarian and first squamous cell cancer. Ovarian most cancers is a type of cancer that happens within the ovaries, the female reproductive organs that produce eggs. Primary squamous cell most cancers, then again, is a kind of cancer that may develop in numerous parts of the physique, including the pores and skin, lungs, and digestive tract.
As with any treatment, Hydrea could trigger unwanted effects in some sufferers. These might embody nausea, vomiting, diarrhea, pores and skin rash, and headache. More critical, however uncommon, unwanted effects might include bone marrow suppression, which may lead to an increased threat of an infection and anemia. It is essential to hunt medical attention if any of those unwanted side effects occur.
It is important to notice that Hydrea is a powerful treatment that ought to only be taken as prescribed by a doctor. It is often given in the type of a capsule that's taken orally once a day. The dosage might vary relying on the situation being handled and the patient's response to the medicine. It is important to take Hydrea at the similar time daily and to not miss any doses to ensure its effectiveness.
In conclusion, Hydrea is a highly efficient medication in the remedy of various types of most cancers, including melanoma, CML, ovarian and first squamous cell cancer, and carcinoma of the head and neck (excluding the lip). It is also beneficial in managing sickle cell anemia. However, as with all medication, you will need to take Hydrea as prescribed and to report any unwanted effects to a healthcare skilled.
Furthermore, Hydrea can additionally be used to deal with carcinoma of the top and neck, excluding the lip. This sort of most cancers can have an effect on the mouth, throat, nose, sinuses, and salivary glands. Hydrea works by preventing the growth and spread of cancer cells in these areas, decreasing the risk of complications and improving the chances of survival.
Hydrea, also referred to as Hydroxyurea, is a medication that's primarily used to deal with a range of cancers, together with melanoma, chronic myelocytic leukemia, ovarian and primary squamous cell cancer, and carcinoma of the head and neck (excluding the lip). It is also used to deal with chronic myelogenous leukemia and sickle cell anemia. Hydrea works by slowing down or stopping the expansion and unfold of cancer cells in the body.
Hydrea can be used to treat sickle cell anemia, a genetic disorder that impacts the purple blood cells. Sickle cell anemia causes the pink blood cells to become abnormally shaped, leading to a decreased oxygen provide to the body. Hydrea helps by growing the production of fetal hemoglobin, which may enhance the symptoms of sickle cell anemia.
Hydrea can be generally used to treat continual myelogenous leukemia (CML), a sort of cancer that affects the blood and bone marrow. CML is characterized by the overproduction of white blood cells, which can lead to anemia, bleeding, and an elevated risk of an infection. Hydrea helps to decelerate the expansion of these irregular white blood cells, allowing the body to supply healthy cells.
One of the primary uses of Hydrea is within the remedy of melanoma, a sort of pores and skin most cancers that develops in melanocytes, the cells that produce pigment within the skin. Melanoma is the most serious type of skin most cancers and might spread to different components of the physique if not treated early. Hydrea is usually used in combination with other remedies, similar to surgery and radiation remedy, to assist forestall the unfold of melanoma and increase the probabilities of survival.
The lesions are commonly associated with infections of the upper respiratory tract and pneumonia medicine 834 purchase hydrea with paypal. The virus may be in a dormant state in the squamous cells of many individuals and is activated by febrile illness. Tumours Squamous-cell carcinoma is the most common malignant tumour of the oral cavity, the most frequent sites being the lower lip and tongue. They are initially painless and hence may be missed until late especially those occurring in the posterior third of the tongue. Malignant ulcers in the oral cavity characteristically have an indurated base and a raised and everted margin. Microscopically squamous-cell carcinoma appear as epithelial clusters showing active keratinisation. Metastasis occurs unilaterally to the submental, submandibular and then to the lower deep cervical lymph nodes. Rarer posterior one-third tumours spread bilaterally to the upper deep cervical nodes. Sialolithiasis Primary calculi are more commonly seen in the submandibular gland ducts than in the parotid. They may be caused by stasis of salivary secretion associated with changes in its physiochemical characteristics. Secondary salivary gland stone formation may occur in hyperparathyroidism, hyperuricaemia and hypercalcaemia. Sialolithiasis will manifest as recurrent and progressive glandular swelling which in the early stages is associated with meals. Stones in the distal part of the duct can be excised and the opening may be stented or marsupialised. Stones in the proximal region are best treated by excision of the gland and the duct. The incubation period is about 21 days and the active state of the disease when viruses are present in the saliva lasts about ten days. There is diffuse interstitial parotid inflammation in mumps which is usually bilateral but occasionally unilateral. This condition comprises a clinical syndrome affecting the salivary glands and lacrimal glands associated with dry eyes (keratoconjunctivitis sicca) and a dry mouth (xerostomia). It is often associated with rheumatoid arthritis, systemic lupus erythematosus and other systemic auto-immune diseases. Microscopical features include glandular atrophy, lymphocyte infiltration and duct proliferation. This disease usually follows a slow benign progression, but there is a significant risk of development of lymphoma. Tumours Tumours of the salivary glands account for less than 4% of all tumours of the head and neck. Acute bacterial sialadenitis Acute bacterial sialadenitis is often caused by infection spreading in to the parotid or submandibular gland from the oral cavity. The condition is associated with poor dental hygiene, periodontal disease, hyposecretion of saliva due to any cause, and stones in the duct causing obstruction. Neonates, elderly and post-surgical patients have a higher risk of developing this condition. Acute bacterial sialadenitis manifests with fever, trismus, dysphagia and painful enlargement of parotid or submandibular gland. The common organisms involved are Staphylococcus aureus, Streptococcus viridans, and Eschericia coli. The condition usually responds to treatment with broad spectrum antibiotics and restoration Pleomorphic adenoma or mixed parotid tumour About 70% of the benign salivary gland tumours are of this type. The lateral or superficial lobe of the parotid gland (lying superficial to the facial nerve) is most commonly affected. The stroma, rich in proteoglycan, is thought to be derived from myoepithelial cells surrounding the acini and early duct system. Recurrent tumour may encapsulate the facial nerve and its removal will necessitate sacrificing the nerve and its branches. It is an adenolymphoma characterised by cystic spaces surrounded by eosinophilic columnar cells. The stroma in between these cysts contain lymphoid tissue including lymphoid follicles. Malignant transformation is rare and the treatment of choice is long term observation or surgical removal. The condition is rare in children and if seen in a child is associated with cystic fibrosis. Inverted papilloma Inverted papillomas resemble unilateral polyps, but about 3% of them are malignant and 3% of the rest may turn malignant. Histologically the epithelium is hyperplastic and invaginates to invade the underlying fibrous stroma. Muco-epidermoid tumour this is the most common malignant tumour of the parotid gland. Histologically the tumour consists of sheets of squamous cells and mucous secreting cells surrounding cystic spaces.
In general medicine in the middle ages order 500 mg hydrea with visa, proximal limb muscles and trunk muscles tend to act in groups for stabilisation, while distal limb muscles act more precisely when the hand or foot is free-moving. The central neurological representation and control of these different groups reflect their functional differences. All muscles act from their fixed end to their mobile end: the latter need not always be distal to the former. Think of the actions of the lower limb muscles when the foot is bearing weight, or of the pectoralis major and latissimus dorsi when the arms are fixed and the chest is moving. The body is very economical: if gravity can supply the force necessary for a movement, then the muscles will let it do so. Stages and events in the life of a bone include its development and growth, its response to physical stress, its changes with age from maturity to senility, and its response to injury both macroscopic and microscopic. New bone must be formed throughout life: the process and sequence of events are always the same, involving both the laying down and the removal of bone. Development and growth entail the modelling of bone morphogenesis and ossification as well as remodelling to maintain its overall shape, proportion and soft tissue relationships as it grows. Change as part of the second, the rôle of bone as an ion reserve, particularly with respect to calcium and phosphate, is dealt with elsewhere, especially in Chapter 14. Change as part of the third, the rôle of bone in haemopoiesis, is discussed in Chapter 10. All three groups of changes are inextricably linked, as all ultimately involve change in the structure of bone and in overall bone mass by the normally coupled mechanisms of bone formation and resorption. Physiological remodelling occurs during biochemical homeostasis and during haemopoiesis, as well as during the constant process of micro-repair and damage limitation which accompanies the normal response of bone to loading. Adaptive changes occur as loading promotes bone formation or unloading its resorption. Reparative remodeling occurs on both a microscopic and a macroscopic scale during the process of fracture healing. The concept of bone mass is an important one, linking the anatomy, physiology and pathology of bone, especially as the latter relates to metabolic bone disease. Total bone mass, including organic and inorganic constituents, increases during development and growth to a maximum reached at 2030 years of age. There is then normally a steady state for about 20 years, but even during this period, turnover of about 15% of the total bone mass occurs every year. In later life, bone mass decreases, hormonal influences such as that of oestrogen withdrawal being particularly important. Bone formation and resorption There are two main mechanisms by which bone mass can alter physiologically or pathologically: · · · · physiological; adaptive; age-related; and reparative. Change occurring as part of the first is integral to the development and maintenance of the form of bone, both macroscopic and microscopic, and will be the the process of bone formation, and the nature of the final product mature bone, cortical and cancellous is generally consistent, though there are two distinct mechanisms of ossification distinguished by the local tissue environment in which the process occurs (see below). Bone, as a connective tissue, has a cellular component and an extracellular matrix. The cellular agents of bone formation and bone resorption are the osteoblasts and osteoclasts, respectively. The osteoblasts belong to a mesenchymal lineage which includes both the surface lining cells of bone and the osteocytes in their lacunae. Osteoclasts develop from extraskeletal blood-borne precursors, sharing their stem cells with circulating monocytes and macrophages. Active osteoblasts produce the organic matrix of bone, based on Type I collagen and osteocalcin, to form a framework of osteoid on which mineralisation later occurs in the presence of normal plasma calcium and phosphate concentrations. Osteoclasts resorb bone as a whole, releasing the inorganic ions and breaking down the matrix proteins. The coupling mechanism must require communication between cells of the osteoblast and osteoclast lineages, the chemical basis of which remains to be elucidated. It is now thought that initial determinant factors act upon cells of the osteoblast series in all cases, and that osteoclast activity is thus under secondary control. Major regulating agents include hormones such as parathyroid hormone and the active metabolite of vitamin D, together with local autocrine and paracrine agents such as growth factors and other cytokines. In addition, bone both produces and transmits electrical signals, usually as a result of loadingrelated microdeformation. The structurally linked osteocytes, communicating via processes in canaliculi in the bone, are probably involved in transduction of mechanical stimuli. The endothelial cells lining the copious blood vessels of bone are increasingly implicated in cellular processes of remodelling and of fracture healing. The extracellular matrix is also now being seen to have a rôle which exceeds that of passive support: it may also be involved in the sensation and transduction of mechanical stimuli. The two mechanisms of ossification are: the former is a direct mechanism in which bone develops in vascularised mesenchyme without an intermediary stage. In the latter, bone develops on the template of a cartilage model: the developing bone replaces the pre-existing cartilage. The remainder of the skeleton ossifies in cartilage, but not exclusively so, as all subperiosteal deposition of new bone (by which bones grow in thickness) is intramembranous. Note that in growing tubular bones this deposition must be accompanied by coupled endosteal resorption to maintain the relative size of the medullary cavity. Intramembranous ossification begins in an area of mesenchymal cell condensation vascularised by capillaries.
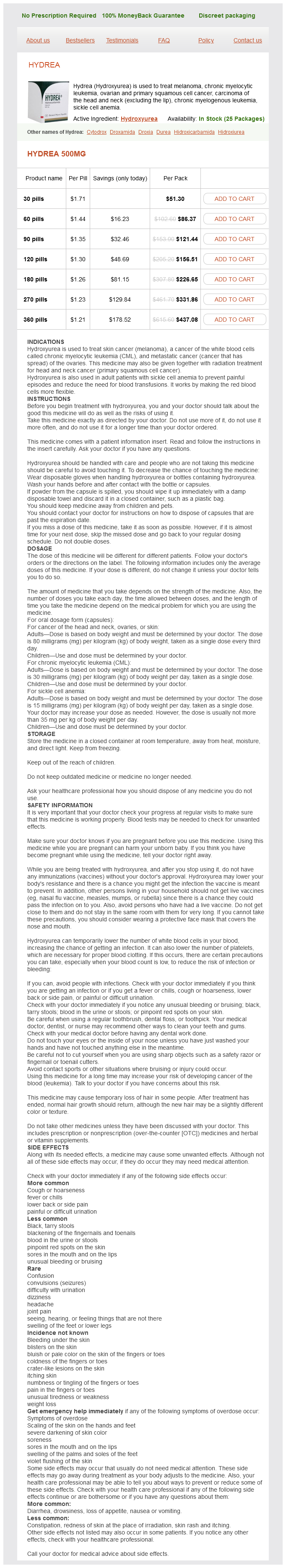
Hydrea Dosage and Price
Hydrea 500mg
- 30 pills - $51.30
- 60 pills - $86.37
- 90 pills - $121.44
- 120 pills - $156.51
- 180 pills - $226.65
- 270 pills - $331.86
- 360 pills - $437.08
They may have little effect on the initial treatment of closed nonangulated lesser toe injuries but may help predict the duration of pain and disability symptoms viral infection order hydrea 500 mg on line. Adult patients who are simply worried about their "purple" toe, when there is little or no pain or swelling and there is no angulation, should be encouraged to forgo the unnecessary irradiation of their foot, because the treatment will be essentially the same whether or not a fracture is present. They can use whatever footwear provides them with the greatest comfort and protection. Buddy taping (described next) can be offered to the patient if it provides any improvement in comfort; otherwise, it is an unnecessary inconvenience. Uncomplicated fractures of the great toe can be managed in the same manner as "turf toe," described in this chapter under the Discussion. Angulation can be further corrected by using a finger as a fulcrum to reverse the direction of the distal fragment. The broken toe should fall in to its normal position when it is released after reduction. The nail bed of the fractured toe should lie in the same plane as the nail bed of the corresponding toe on the opposite foot. If it does not, rotational deformity should be suspected and corrected by further manipulation. Postreduction, splint the broken toe by taping it to an adjacent, nonaffected toe (buddy taping). Slide one thickness of gauze or Webril cotton pads between the two toes, and, using half-inch tape, bind the toes together. Give the patient additional padding and tape so that he may revise the splinting, and (if there is a fracture) advise him that he will require such immobilization for approximately 1 week, by which time there should be good callus formation around the fracture and less pain with motion. Inform the patient that he must keep the padding dry between his toes while they are taped together or the skin will become macerated and break down. If the toe required reduction, warn him not to separate his toes when replacing the padding. A cane, crutches, or hard-soled shoe that minimizes toe flexion may also provide greater comfort. Let the patient know that, in many cases, a soft slipper or an old sneaker with the toe cut out may be more comfortable. If the fracture is not of a phalanx but of the metatarsal, buddy taping is not effective. Orthopedic or podiatric referral is indicated in patients with circulatory compromise, open fractures, significant soft tissue injury, fracture-dislocations, displaced intra-articular fractures, or fractures of the first toe that are unstable or involve more than 25% of the joint surface. What Not To Do: Do not tape toes together without padding between them, unless the tape is changed frequently and the skin is dried thoroughly if it becomes wet. Do not let the patient overdo ice, which should not be applied directly to skin and should not be used for more than 10 to 20 minutes per hour. It is questionable whether or not cryotherapy provides any benefit, and it should be used only if it reduces discomfort. The same mechanisms that produce toe fractures may cause a ligament sprain, contusion, dislocation, tendon injury, or other soft tissue injury. With a clinically significant injury, radiographs are often required to distinguish these injuries from toe fractures. If there is no toe fracture, the treatment is the same, but the pain, swelling, and ability to walk may improve in 3 days rather than 1 to 2 weeks. Although patients call the emergency department or clinic wanting to know whether or not their toe may be broken, if there is no deformity, they can usually be managed adequately over the telephone and seen the next day. They typically involve the medial base of the proximal phalanx and usually occur in athletes. Stress fractures have a more insidious onset and may not be visible on radiographs for the first 2 to 4 weeks after the injury. More severe injuries will exhibit marked swelling, limited range of motion, and an antalgic gait. Radiographs should be obtained to rule out associated fractures and possible degenerative arthritis. Moderate sprains require additional immobilization with cast padding, Ace wrap, and use of a stiff cast boot. These symptoms may have developed gradually, after minor turning of the head, after vigorous exercise, or overnight during sleep. What To Do: Ask the patient about precipitating factors, and perform a thorough physical examination, looking for muscle spasm, point tenderness, signs of injury, nerve root compression, masses, or infection. Include a careful nasopharyngeal examination as well as a basic neurologic examination. When forceful trauma is involved and fracture, dislocation, or subluxation is possible, obtain lateral, anteroposterior, and odontoid radiographic views of the cervical spine. When there is no suspicion of a serious illness or injury, carefully examine the side of the neck in spasm for tender trigger points. Press your examining finger firmly and deeply in to the neck muscles along muscular borders and their origins and insertions, searching for one or two spots approximately the size of your fingertip that cause the patient to wince in pain. If a localized trigger point is discovered, you may consider treating this as for any other source of myofascial pain and thus inject these areas with 5 to 10 mL of bupivacaine (Marcaine) 0. Trigger-point injection can often partially or completely relieve the symptoms of the acute and painful form of torticollis. After trigger-point injection or when a trigger point cannot be found (or the patient elects not to have the injection), have the patient apply ice to decrease inflammation and spasm for the first 48 hours; then switch to heat. Alternating heat with ice massages may also be helpful, as well as gentle range-of-motion exercises and friction massage. Position the wider segment of the collar on the side that produces the greatest comfort for the patient. Inform the patient that with successful trigger-point injection, there may be mild soreness the next day and complete resolution of discomfort over the next week.
© 2025 Adrive Pharma, All Rights Reserved..