General Information about Glyset
Glyset is a medicine that has been making waves within the area of diabetes administration. It is an FDA-approved drug used as an adjunct to food regimen and exercise to improve glycemic management in adults with sort 2 diabetes mellitus. In simpler terms, it helps to control blood sugar levels in individuals residing with diabetes, allowing them to higher handle their condition and improve their overall health.
This is the place Glyset is out there in. It belongs to a category of medicine referred to as alpha-glucosidase inhibitors, which work by slowing down the digestion and absorption of carbohydrates in the body. Carbohydrates are the main source of sugar in our food regimen, so by slowing down their absorption, Glyset helps to stop a sudden spike in blood sugar levels after a meal. This, in flip, helps to keep blood sugar ranges within a wholesome range.
In conclusion, Glyset is a useful medication in the therapy of sort 2 diabetes. It presents an effective way to manage blood sugar ranges, with out inflicting hypoglycemia. Its flexible dosing and good security profile make it a handy and protected choice for a lot of people with diabetes. If you or a loved one has sort 2 diabetes, speak to your healthcare supplier to see if Glyset might be a helpful addition to your treatment plan. Remember, a combination of a healthy diet, common train, and correct medicine might help you keep better management of your diabetes and lead a happier, healthier life.
Like any medicine, Glyset does include some potential side effects, corresponding to bloating, diarrhea, and gas. These side effects are normally delicate and can be managed by adjusting the dosage or taking the medicine with meals. It is important to discuss any potential side effects with a healthcare provider and report any concerning signs.
Type 2 diabetes is a chronic situation that affects tens of millions of individuals worldwide. It is characterized by high blood sugar ranges due to the body's incapability to supply enough insulin or correctly use the insulin it produces. Over time, this could lead to critical well being problems, corresponding to coronary heart illness, nerve harm, and even blindness. Managing diabetes requires a combination of way of life adjustments, including a healthy diet and common train, and sometimes medication to regulate blood sugar levels.
In addition to its effectiveness in controlling blood sugar ranges, Glyset also has a great safety profile. It has been on the market for over 20 years and has been studied in quite a few medical trials. It has additionally been proven to be safe for use in combination with other diabetes medicines, making it a versatile treatment option.
One of the primary advantages of Glyset is that it doesn't cause hypoglycemia (low blood sugar) on its own. This is a common concern for many individuals with diabetes, particularly those who take insulin or different medications that may lead to low blood sugar. With Glyset, this danger is significantly lowered, making it a safer option for many people.
Another benefit of Glyset is that it can be taken without regard to meals. This signifies that it does not need to be taken earlier than or with meals like another diabetes medicines. This added flexibility can be very helpful for folks with busy schedules or those that wrestle with remembering to take their medicine on time.
Clinical research have proven that Glyset can successfully decrease A1C ranges in individuals with type 2 diabetes. A1C is a measure of average blood sugar ranges over the previous 2-3 months and is used to assess long-term glycemic control. By decreasing A1C ranges, Glyset can help to prevent or delay the onset of diabetic complications, bettering the overall health and high quality of life for these living with the situation.
To isolate neutrophils buy discount glyset 50 mg,12 whole blood is diluted with saline and underlaid with Ficoll-Paque solution. After centrifugation for 30 minutes at 500 g, the lessdense monocytes, lymphocytes, basophils, and platelets remain at the upper interface of the Ficoll-Paque solution, whereas the denser erythrocytes and neutrophils pass through the solution and pellet at the bottom. The mononuclear cells are carefully harvested and the remaining Ficoll-Paque solution aspirated. The erythrocyte/neutrophil pellet is resuspended with saline and mixed with 3% dextran. Dextran promotes the formation of rouleaux by the erythrocytes, causing them to sediment more rapidly than the neutrophils at 1 g. The neutrophil-enriched supernatant fluid is harvested from the bulk of the erythrocytes. Contaminating erythrocytes are removed by a brief (30-second) hypotonic lysis with 0. All procedures are performed at room temperature, and the isolated cells are maintained in a balanced salt solution without divalent cations. In a band neutrophil, the nucleus is horseshoe shaped, with no indication of constriction into lobes. The pinkviolet staining of the cytosol is associated with numerous, evenly distributed, specific granules; occasionally a dark-staining primary granule may be present. Neutrophils from a patient with myeloperoxidase deficiency fail to stain for myeloperoxidase in the neutrophils. Endothelial cell monolayers harvested from human umbilical veins may serve as a more physiological substrate for the measurement of cell adhesion. Nonspecific esterases in the cytosol cleave the ester linkage, trapping the fluorescent probe in the cytosol. At the end of the incubation, the wells are washed three times to remove nonadherent cells. The fluorescence of each well is determined with a fluorescent microplate reader and compared with the fluorescence of a control well with a fixed number of fluorescent cells. This adherence assay is valuable in the diagnosis of patients with leukocyte adhesion deficiency. Both enzymatic assays and immunoassays are available to determine the cellular content of many of these granule constituents. Patients with leukocyte chemotactic defects usually show recurrent skin abscesses and occasional life-threatening, invasive infections. Principles and Interpretation of Laboratory Assessment the cellular content of neutrophils can be determined by solubilization of a neutrophil pellet with 0. Analysis of the lysate using commercial immunoassays can identify deficiencies of certain granule contents. Diagnosis of myeloperoxidase deficiency can be confirmed by analysis of neutrophil lysates. The wells of a 96-well plate were coated for 1 hour at 37°C with 32 µL of either buffer alone, fetal bovine serum, or fibrinogen (2. The wells were washed three times, and then cells were added to each well (160 µL/well, 3. The percentage of adherent cells was determined by the ratio of the fluorescence of the well compared with the fluorescence of a known standard well. The lower chamber contains the chemoattractant and is separated from the cellular compartment by a filter. However, instead of a top chamber, the filter has a hydrophobic mask around each filter site that creates surface tension in the cell suspension and aligns the suspension on the hydrophilic filter located directly above the chemoattractant chamber. Nonmigrating neutrophils atop the filter are rinsed off with buffer, and then the plate is read in a fluorescence microplate reader. The number of migrating neutrophils can be determined by comparison of the fluorescence to a standard well with a known number of fluorescent neutrophils. The advantages of this assay are high sensitivity, rapid acquisition and analysis of data, and reduced labor in loading the cell suspension. The 96-well format also allows for multiple comparisons to be made under identical conditions. By acquiring digital images over time and analyzing them using imaging software, the coordinates of individual cells can be determined. Changes in the distance (and velocity) in the direction of the chemoattractant (directed migration) and orthogonal to the direction of the chemoattractant (random migration) can be determined. Adding time as a dimension in the analysis of chemotaxis provides a mechanism to evaluate simultaneously both chemotactic and chemokinetic responses in neutrophils and to detect more subtle defects. Flow cytometric analysis of adhesion molecules on the neutrophil cell surface can indirectly reflect neutrophil adhesion function. Principles and Interpretation of Laboratory Assessment the expression of cell surface antigens is determined on neutrophils stained with specific fluorescent monoclonal antibodies (mAbs) and analyzed by flow cytometric analysis. The antibody 7D5 recognizes an extracellular epitope of gp91phox and can be used to identify surface expression of gp91phox as well as mobilization of latent pools of gp91phox stored in the specific granules. Antigen expression can be upregulated because of translocation of latent antigen to the plasma membrane or downregulated because of either internalization or shedding of the antigen. Lactoferrin that is released from specific granules can chelate iron, resulting in a bactericidal or bacteriostatic effect. Elevation of plasma lactoferrin is an indication of intravascular activation and degranulation of neutrophils. Using the acquired images, 10 randomly chosen cells were electronically tracked and the paths of the cells plotted with their position at t = 0 anchored at the origin. Presented in the bottom panel are scattergrams of the average velocities of the individual cells that were tracked in the top panel.
The cause of Crohn disease is unknown 50 mg glyset with visa, but it is thought to result from a dysregulated immune response to gut microbes. However, it seems clear that the complex interactions of environmental exposures (including the gut microbiome and its metabolome), innate and adaptive immune dysfunction, and complex genetic and epigenetic features are all complicit in disease causation and expression. Abdominal pain may indicate bowel obstruction (especially if the pain is postprandial), an inflamed viscus, or a penetrating complication, such as an abscess or fistula. Diarrhea is related to malabsorption and dysmotility secondary to the effects of inflammatory cytokines on gut function. Conversely, constipation in Crohn disease can be a sign of stricturing of the bowel. Extraintestinal manifestations of Crohn disease include arthritis, uveitis, inflammatory skin lesions (pyoderma gangrenosum and erythema nodosum), and stomatitis. The arthritis can affect the axial (spine and pelvis) and articular skeleton, with the latter more often mirroring the activity of the gut disease. The joint complaints range from usual arthralgias to frank synovitis with swelling and tenderness (without erosive joint destruction). Many of these lesions will subside with effective therapy aimed at the gut, but they can also have independent courses that require site-targeted treatment. The incidence of Crohn disease in North American populations has been estimated to be 3. Ashkenazi Jewish heritage confers increased risk in Caucasians, whereas African Americans seem to have rates similar to those of non-Jewish Caucasians, and Hispanics and Asians have much lower rates. The only environmental exposure that has been repeatedly linked to risk of Crohn disease has been tobacco use. The majority (up to 70%) of Crohn patients experience a remitting and relapsing course, but some have chronically active symptoms refractory to medication. The recognized phenotypes of disease include inflammatory (manifesting primarily as intestinal edema and ulceration), fibrostenotic (luminal narrowing by fibrous strictures dominate with symptoms of painful obstruction), and fistulizing (inflammatory tracts between the bowel and other intestines, the bladder, vagina, skin, and other structures). Although the majority of patients have inflammatory disease at the time of diagnosis, over time this phenotype changes so that after 20 years of disease duration, up to 70% and 18% of patients with Crohn disease report penetrating and fibrostenotic complications, respectively. However, it was further estimated that all the loci together could account for no more than 13. The roles of antibiotics, probiotics, prebiotics, or actively changing the microbiota through fecal transplant have not been clarified sufficiently to employ these strategies as conventional treatments in Crohn disease. Diagnosis the diagnosis of Crohn disease is based on findings from radiographic, endoscopic, and histological examinations. Currently, medically refractory inflammatory disease may be treated with natalizumab, an anti-4 integrin antibody, although this is being supplanted by vedolizumab, an anti-47 antibody inhibiting the trafficking of lymphocytes from the blood specifically into the gut lamina propria. An established approach to immunosuppressant- and biological-naïve patients is to begin with a combination of azathioprine and infliximab, as this has been shown to be superior to either a single agent alone for inducing remission, especially 1 year later. Surgery is required in cases of complications, such as bleeding, pain/obstruction, and fistulae that are refractory to medical therapy. Surgery typically involves resection limited to inflamed segments of small intestine and colon; small strictures can be treated in situ by stricturoplasty. In addition, surgery is required for treatment of intestinal adenocarcinoma, which also complicates the chronic inflammation of the bowel. Endoscopically, mucosal ulceration and friability in a patchy distribution separated by unaffected mucosa ("skip areas") are hallmarks of the disease. Radiographically, evidence of patchy bowel wall thickening, mucosal hyperemia, stricturing, and penetrating complications, such as fistulae, abscesses, and extraintestinal inflammatory masses involving the bowel, all suggest Crohn disease. Histologically, although the appearance of noncaseating granulomata is highly supportive of a diagnosis of Crohn disease, in practice, they are not often detected by endoscopic biopsy, particularly in adults. More often evidence of chronic inflammation, such as architectural crypt distortion and basal lymphoplasmacytosis, are sought to differentiate the inflammation from an acute, self-limiting colitis or enteritis. Treatment the treatment of Crohn disease includes medical and surgical approaches. The goal is to induce quick remission of symptoms and establish therapy to maintain the remission with aggressive initial therapy commensurate with the extent and activity of the disease. It can affect the rectum alone (ulcerative proctitis), the distal transverse colon to rectum (left-sided colitis), or the entire colon (pancolitis). However, there can be ongoing complications of the surgery, such as pouchitis, when an ileal pouchanal anastomosis is performed. Bloody stool and diarrhea (including nocturnal) are common symptoms, with proctitisspecific complaints of rectal urgency and incomplete evacuation also being prominent. Extraintestinal manifestations may include arthritis, uveitis, inflammatory skin lesions, and stomatitis. Total colectomy is performed to treat refractory symptoms or development of epithelial dysplasia. This is best accomplished by colonoscopy (ileal intubation can confirm that the inflammation is limited to the colon). Biopsy specimens should contain histological features of chronic inflammation, including crypt distortion, crypt dropout, and lymphoplasmacytosis. The presence of acute inflammatory features alone (polymorphonuclear cells, crypt abscess, and cryptitis) may also be seen but, when in isolation, these features suggest other etiologies, such as acute infectious, drug-induced, ischemia, and toxic exposures. Most often with more extensive colonic involvement, oral mesalamine is required, which can be useful for induction and maintenance of remission.
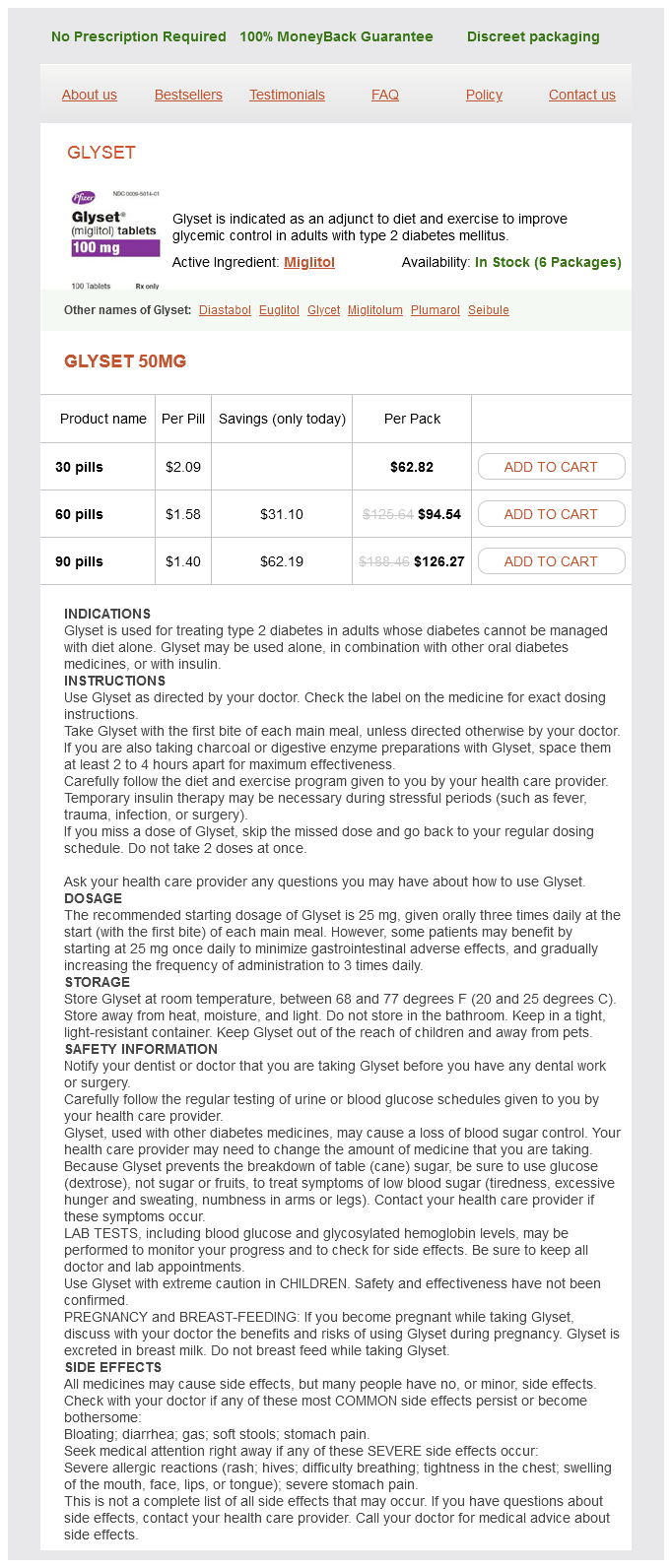
Glyset Dosage and Price
Glyset 50mg
- 30 pills - $62.82
- 60 pills - $94.54
- 90 pills - $126.27
These methodologies could not have been developed without elucidation of the scientific basis of the developmental phenotype of immune cells (Chapters 7 and 8) and of the elaborate process of Ig gene rearrangements (Chapter 4) purchase glyset once a day. Thus any single T or B lymphocyte carries a unique rearrangement that is not shared by any other lymphoid cell. The two major clinical parameters of prognostic significance are age at diagnosis and leukocyte count. A presenting age between 1 and 9 years and a leukocyte count <50 × 109/L are favorable prognostic factors. In adults, the outcome of therapy worsens with increasing age and leukocyte count. Patients >60 years of age and/or a leukocyte counts >100 × 109/L have a particularly poor response to treatment. The prognostic significance of the major genetic aberrations has been described above. Flow cytometric analysis of these immunophenotypes allows the detection of one leukemic cell among 10-4 or more normal cells. It may be difficult to distinguish between regenerating B-cell progenitors and leukemic blasts. More than 90% of the children with low-risk leukemia and 70% of those with high-risk leukemia are cured. Most relapses occur during treatment or within the first 2 years after completion of therapy. Leukemic relapse occasionally occurs at other sites, including the eye, ear, ovary, uterus, bone, muscle, tonsil, kidney, mediastinum, pleura, and paranasal sinuses. Treatment Sequelae In the 1990s, improvements in supportive care reduced the rate of early death to <2%. However, the death rate among older patients during remission induction therapy remains as high as 30% because of hematological, hepatic, and cardiac toxicities. Aseptic necrosis of various bones has emerged as a common late toxicity of glucocorticoids, especially in adolescent girls treated with dexamethasone. The rate of long-term neurotoxicity has been reduced as a result of replacement of cranial irradiation with high-dose and intrathecal methotrexate. However intensive methotrexate therapy can also have late neurodegeneration effects. Children who received cranial irradiation at 6 years of age or younger are most susceptible to the development of brain tumors. It is the most common leukemia in adults living in countries in the Western hemisphere. Some patients have an indolent course, whereas other have a more rapid and aggressive disease. A further increase in cure rates will require efforts to maximize the efficacy and minimize the toxicity of current therapy. However, about half the patients belong to an "intermediate risk" group in which most of the relapses occur. Optimization of diagnosis and treatment of this group of patients is one of the current major challenges. Advanced genomic technologies carry the promise of discovering the full spectrum of leukemogenic pathways and the identification of targets for new therapies. The identification and specific targeting of these resistant cells is a major future challenge. There is a male predilection, and the disease appears to have geographical and ethnic variations in incidence. Because many of these patients may never require tissue diagnosis or inpatient treatment, cases among them are not likely to be recorded in a tumor registry, thus making the true annual incidence of the disease higher than previously thought (6. B-cell lymphoproliferative disorders are related to different stage of normal B-cell development. ProB and preB cells give rise to acute lymphoblastic leukemia; intermediate stages give rise to mantle zone lymphoma; and late and more mature stages give rise to marginal zone lymphomas and plasma cellderived multiple myelomas. However, as with other forms of malignancy, there is increasing evidence for the role of inherited factors in its development. Family surveys show a genetic predisposition in first-degree relatives, who also demonstrate increased susceptibility to other lymphoproliferative disorders, including other lymphomas. When an antigen of adequate affinity engages the receptor, the cell enters a germinal center located in a lymphoid follicle. There, as a centroblast, it rapidly divides and the V domains of its Ig undergo somatic hypermutation. Cells with receptors that have enhanced antigen-binding affinity proliferate in the presence of the antigen, whereas centrocytes with receptors that no longer bind the antigen (or bind autoantigens) are normally eliminated. These differences in the extent of V domain mutation suggest differing entities with two different developmental histories. The mutational status of the V domains strongly correlates with prognosis in that patients with an unmutated clone have a much worse prognosis compared with patients with mutated clones. These patients may differ also in their association with specific genetic aberrations. These chromosomal aberrations have independent prognostic significance (unrelated to the mutational status). The pathological features of biopsy specimens of lymph nodes are those of a small lymphocytic lymphoma. Interaction with and evasion from the normal immune system has been shown to be of significance. Hyperleukocytosis, which causes leukostasis and necessitates emergency treatment, is extremely rare. Other organs that are involved include other lymphoid tissues and rarely solid organs or skin.
© 2025 Adrive Pharma, All Rights Reserved..