General Information about Gabapentin
Apart from epilepsy, Gabapentin has additionally been discovered to be helpful in treating nerve ache, also referred to as neuropathic ache. This sort of ache is caused by harm or dysfunction in the nerves, and it might be fairly challenging to manage. Gabapentin has been found to be effective in decreasing this type of pain, and it's typically prescribed to individuals with diabetic neuropathy, postherpetic neuralgia, and different kinds of nerve ache.
The effectiveness of Gabapentin in treating epilepsy has been extensively studied, and it has proven to be extremely efficient. In a review of sixteen research, it was discovered to minimize back seizure frequency by 50% or extra in 40 to 50% of sufferers. Moreover, it has been shown to be well-tolerated, with very few unwanted aspect effects.
Gabapentin is mostly well-tolerated, and most people experience minimal unwanted effects, similar to dizziness, drowsiness, and fatigue. However, it is essential to observe the prescribed dosage and inform your healthcare supplier should you experience any concerning unwanted effects. In uncommon cases, it might possibly additionally cause extra severe side effects, corresponding to suicidal ideas, confusion, and breathing difficulties.
In conclusion, Gabapentin, or Neurontin, is a useful treatment for the therapy of epilepsy and different neurological situations. It has been proven to be highly efficient in controlling seizures and managing nerve pain. However, it is essential to work closely along with your healthcare supplier to find out the proper dosage and to monitor for any potential unwanted side effects. With correct use, Gabapentin can significantly improve the standard of life for people residing with these difficult situations.
Epilepsy is a neurological dysfunction characterised by recurrent episodes of seizures. It affects hundreds of thousands of individuals everywhere in the world, with an estimated 50 million individuals living with the situation. The precise cause of epilepsy remains to be unknown, but various elements similar to genetics, head accidents, and brain infections are thought to contribute to its growth. One of the first treatments for this condition is a medicine known as Gabapentin, generally recognized by the commerce name Neurontin.
Gabapentin belongs to a class of medicines known as anticonvulsants. It works by altering the degrees of neurotransmitters in the mind, corresponding to GABA, which helps to manage electrical activity within the brain. In individuals with epilepsy, abnormal electrical exercise within the mind could cause seizures. Gabapentin helps to calm this activity, thereby preventing seizures.
It can be price noting that Gabapentin can work together with different drugs, so it is essential to inform your doctor about any other drugs you are taking before beginning treatment. People with kidney issues should also use Gabapentin with warning, as it is primarily excreted via the kidneys.
In addition to its major use, Gabapentin has also been discovered to be helpful in managing signs of other conditions, corresponding to stressed leg syndrome, alcohol withdrawal syndrome, and fibromyalgia. Its mechanism of action is believed to play a task in relieving the symptoms of those situations, making it a flexible medication within the administration of assorted neurological disorders.
How does Gabapentin work?
Gabapentin was first approved by the US Food and Drug Administration (FDA) in 1993 to treat seizures associated with epilepsy. It is a prescription medication that has confirmed to be efficient in controlling seizures, especially in sufferers whose signs are not adequately controlled by different anti-seizure medicines. Over the years, it has also been discovered to be useful in treating other conditions, such as nerve pain and restless leg syndrome.
However symptoms leukemia purchase gabapentin with paypal, in 20% of the population, the vertebral artery bends too medially, posteriorly, or rostrally,13 a variant that is termed a high riding vertebral artery. The presence of a high riding vertebral artery must alert the clinician to changes in the normal pedicle anatomy. The ligamentous restraints of the upper cervical spine are crucial to normal physiologic motion. Routine orthogonal X-rays are recommended, which should consider the open mouth view to include the odontoid and lateral masses of C1. Independent of vertebral artery variants, the C2 pedicle diameter is often too narrow to safely instrument. The C2 translaminar screw technique was described by Wright in 2004 (the first report of C2 translaminar screw placement in which 10 patient cases were presented and no neurologic or vascular injuries were encountered). This process is repeated on the opposite side at a more inferior position on the C2 lamina to allow for an un-impeded path for the second screw. In a study of 50 patients, 24% had vertebral artery anatomy that would preclude safe pedicle screw placement. Posterior laminar wiring was commonly practiced earlier, but it is performed less commonly now due to a 10 to 30% pseudoarthrosis rate and a lack of rotational control. Using a posterior approach, a screw is placed from the inferior facet of C2 through the C1C2 facet joint, and into the C1 lateral mass. Complications of C2 Translaminar Screw Placement compared lateral mass/translaminar screw constructs with lateral mass/pedicle screws in a cadaveric model. In contrast, Claybrooks et al found that translaminar screws had less stiffness in lateral bending and axial rotation, a strong trend toward less anterior/posterior stiffness translation that did not reach statistical significance, and no difference in flexion/extension strength. The biomechanics of C2 translaminar screws when the instrumentation is extended into the subaxial spine have been studied as well. However, they were found to be more rigid in axial rotation and equivalent in flexion and extension when compared to 20-mm C2 pedicle screws. However, he noted a decreased pull-out strength and torque when compared to the index pedicle screw. A higher percent of patients are candidates for this compared to pedicle screws, simply due to the vertebral artery proximity to the pedicle. As with any surgical technique, however, a thorough understanding of potential complications is vital. This was noticed prior to instrumentation and was not associated with either a dural tear or neurologic symptoms. Along the same lines, Bransford et al have documented 0% neurologic injury in 63 C2 translaminar screws. Additionally, the added space taken by offset connectors may also decrease the space for bone grafting at the C2C3 joint. Some authors have reported 0% infection rates in large studies,42 while others have reported rates as high as 18%. In comparison to the other common C2 fixation strategies, translaminar screws seem to have an unfavorable infection profile. Thus, infection rates have not been definitively shown to be higher with this technique. However, further studies need to be performed to clarify the putative increased infection rate trend observed in the literature. Emphasizing ambulation, physical therapy, and pulmonary toilet will minimize pulmonary complications. Obtaining the support of nutritionists as well as speech pathologists will help avoid postoperative complications. Therefore, there is concern for increased neck pain from the translaminar hardware itself. Both muscles have been implicated as generators of neck pain in the postoperative laminoplasty patient. Although more dorsal screw heads are in consideration, the literature is sparse in this area. With proper surgical technique, there is essentially no risk to the vertebral artery. However, a trend toward increased pseudoarthrosis rates has been shown when compared to C2 pedicle screw constructs and C1C2 transarticular fusion, likely from biomechanical weakness in lateral bending. Using the lamina as a guide, ventral breech is rare and neurologic deficit has not been reported. Instability of the cervical spine after decompression in patients who have Arnold-Chiari malformation. Anatomic study of the axis for surgical planning of transarticular screw fixation. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Translaminar versus pedicle screw fixation of C2: comparison of surgical morbidity and accuracy of 313 consecutive screws. The quantitative anatomy of the vertebral artery groove of the atlas and its relation to the posterior atlantoaxial approach. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients: modification of the Harms and Goel techniques. Complications of Subaxial Lateral Mass Screw Fixation 8 Complications of Subaxial Lateral Mass Screw Fixation Adewale O. Thorough knowledge of the relevant anatomy is crucial to avoid potentially devastating complications of neural element and vertebral artery injury. Berthold Ernest Hadra1,2 of Chicago first reported posterior instrumentation of the subaxial cervical spine in 1891 after successfully treating a patient with a fracture by wiring the spinous processes of C6 and C7 together using a silver wire and demonstrating the technique on cadavers.
T1-weighted imaging may help identify bone invasion particularly in marrow-rich bone such as the clivus medications definition buy gabapentin on line. Fatty infiltration of the pterygoid or temporalis muscles, for example, may suggest a loss of function of the motor branch of the trigeminal nerve due to chronic denervation. T2-weighted imaging can also help differentiate between trapped mucous secretions and soft-tissue tumor. Secretions are typically hyperintense on T2-weighted imaging in comparison to solid tumor, which is mildly hyperintense to intermediate in signal. Tumor adjacent to the periorbita, extraocular muscle involvement, and orbital fat obliteration may suggest orbital invasion. Special nuclear imaging such as technetium-99 m, gallium67, indium-111 scans can also be helpful in certain situations to better help delineate infectious processes such as osteomyelitis of the skull base. Technetium-99 bone scans are typically positive focally shortly after an acute infection. These scans, however, may remain positive long after the clearance of the infectious process. Gallium-67 scans, on the other hand, may be helpful in monitoring responses to therapy and may be used to monitor the progress of infectious processes. Indium-111labeled scans are helpful in identifying acute or chronic processes but may be more specific than the other two modalities in identifying infection. Compared to the open approach, endoscopic approaches may be associated with fewer complications and shorter hospital stays. Tumor erosion through the posterior wall of the frontal sinus may be resectable, but extensive tumor extension into the frontal sinus abutting the anterior wall requires an open approach through either a frontal craniotomy or an osteoplastic flap. For anterior skull base meningiomas, relative contraindications include meningiomas with extensive encasement of critical vascular structures. The principles of the endoscopic craniofacial resection for sinonasal malignancies generally involve debulking of tumor to the pedicle point followed by resecting a margin around the tumor pedicle and achieving negative surgical margins. Intraoperative frozen sections may help confirm the absence of microscopic residual disease at the margins of resection. Resection of the bony skull base is necessary for tumors pedicled on the skull base, and often resection of dura is also necessary for adequate clearance of the margins, although this is dependent on the structures involved by the tumor and the biology of the tumor. This entails wide opening of the frontal recess from the lamina papyracea of one orbit to the other side. The floor of the frontal sinuses, the intersinus septum, and the superior nasal septum are removed. The lamina papyracea is skeletonized bilaterally, and may be removed depending on tumor extent. The ethmoid sinuses are resected such that the skull base can be visualized superiorly. On the nasal aspect of the tumor, the lesion may be debulked up to the pedicle point on the skull base. Ligation and division of the anterior and posterior ethmoidal arteries is usually necessary to reduce the blood supply to tumor on the skull base and to facilitate resection of the bony skull base. Posteriorly, the planum sphenoidale is the limit of resection for sinonasal malignancies. Once the bony cuts Endoscopic Anterior Craniofacial Resection Endoscopic anterior craniofacial resection is typically used for midline tumors of the nasal cavity or ethmoid sinuses with skull base involvement. However, many sinonasal malignancies as well as anterior skull base meningiomas may now be accessed with this approach. This allows for resection of skull base pathology as well as intracranial resection when necessary. Limits of resection for this approach include the frontal sinus anteriorly, the planum sphenoidale posteriorly, and the midline of the orbits laterally. Clinical and/or imaging findings 144 Open and Endoscopic Approaches to the Sinonasal Cavity and Skull Base have been made, the underlying dura and olfactory nerves are resected if it is suspected they are involved with tumor. A meningioma that spans the anterior cranial fossa floor is approached slightly differently, with the basic tenet of internal debulking followed by a capsular dissection. They are then typically debulked internally and then approached by a capsular dissection after allowing the tumor and surrounding dura to descend intranasally. This approach may be used for access to tumors, encephaloceles, and skull base trauma. These approaches require careful incision placement and bony osteotomies either for extirpation of tumors or for surgical access. These approaches may be used when patients have contraindications for endoscopic approaches, or depending on surgeon comfort and experience. Endoscopic Lateral Approaches Tumors with lateral extension can now also be approached endoscopically. Removal of the posterior wall of the maxillary sinus and drilling of the pterygoid plates may facilitate access to these areas. Therefore, by following the nerve, the internal carotid artery can be located and protected during dissection. This approach is performed by making an incision in the nasal vestibular mucosa over the piriform aperture and drilling the bone of the piriform aperture to enlarge the working area and facilitate lateral access. More posteriorly, the inferior turbinate may be resected and the nasolacrimal duct transected. A Caldwell-Luc approach can be used to facilitate access to the lateral maxillary sinus. A bony window is then made into the maxillary sinus, which can be used for the endoscope or for instrumentation.
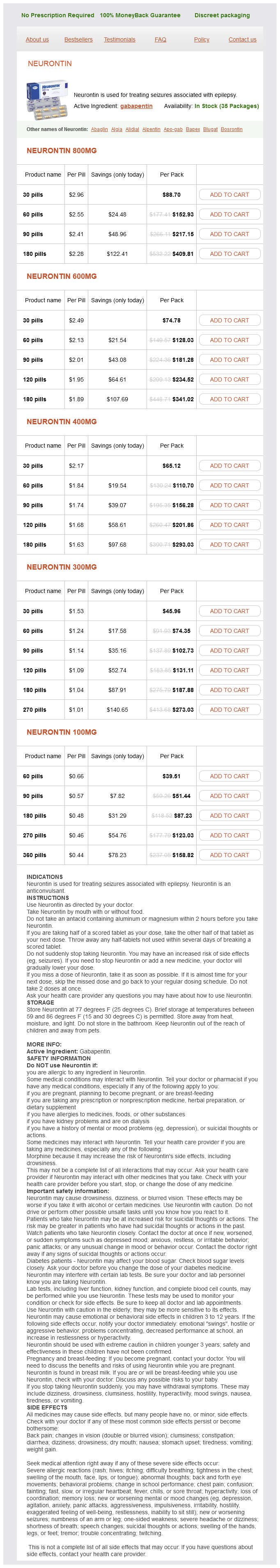
Gabapentin Dosage and Price
Neurontin 800mg
- 30 pills - $88.70
- 60 pills - $152.93
- 90 pills - $217.15
- 180 pills - $409.81
Neurontin 600mg
- 30 pills - $74.78
- 60 pills - $128.03
- 90 pills - $181.28
- 120 pills - $234.52
- 180 pills - $341.02
Neurontin 400mg
- 30 pills - $65.12
- 60 pills - $110.70
- 90 pills - $156.28
- 120 pills - $201.86
- 180 pills - $293.03
Neurontin 300mg
- 30 pills - $45.96
- 60 pills - $74.35
- 90 pills - $102.73
- 120 pills - $131.11
- 180 pills - $187.88
- 270 pills - $273.03
Neurontin 100mg
- 60 pills - $39.51
- 90 pills - $51.44
- 180 pills - $87.23
- 270 pills - $123.03
- 360 pills - $158.82
Dysphagia is managed by modifying the diet to consist mostly of liquids until the symptoms resolve medicine 627 order cheap gabapentin online. Heller Cardiomyotomy Clinical Vignette A 28yearold woman presents with acid reflux and a 15 lb (6. Prior to closing the diaphragmatic crura, the muscular layer of the lower esophagus and the seromuscular layer of the gastric cardia are completely divided, leaving the mucosal layer intact. Whenever possible, a partial fundoplication is performed to reduce the amount of acid reflux into the esophagus. Furthermore, young patients generally tolerate complications better than the elderly. Myotomy Squamocolumnar junction Common Upper Gastrointestinal Surgeries 57 Complications Immediate postmyotomy complications include gastric or esophageal perforations. Persistent dysphagia, even several months after surgery, may be the result of an incomplete myotomy or adhesion formation. Procedure Surgical resection of gastric neoplasms or for complicated peptic ulcer disease involves a partial resection of the stomach and reestablishment of gastrointestinal continuity by reconnecting the gastric pouch to the small intestine. The duodenal bulb, gastric pylorus, antrum, and a small portion of the body of the stomach are resected, and an anastomosis between the gastric remnant and proximal portion of the remaining duodenum is made, thereby preserving a physiologic flow of chyme. The remaining duodenum containing the ampulla of Vater drains into the stomach as the afferent limb; the loop of jejunum connected by an endtoside anastomosis to the stomach forms the efferent limb. Common Upper Gastrointestinal Surgeries 59 In the case of a gastrectomy for malignancy, lymphadenectomy is often added and involves removal of the pyloric, portal, celiac, splenic, and cardiac lymph nodes. In the case of a gastrectomy for ulcer disease, truncal vagotomy may be performed. Vagotomy is not required when gastrectomy is performed for gastric adenocarcinoma because the patients are often achlorhydric. Indications Complicated peptic ulcer disease: this is defined as an ulcer associated with bleeding, perforation, or gastric outlet obstruction or refractory to medical and endoscopic management. Complications Anastomotic Leak this is a dreaded postoperative complication that can result in peritonitis and septic shock. Postgastrectomy Syndromes Postvagotomy diarrhea likely results from colonic hypersecretion due to excess bile acids and bile salts that are unabsorbed in the small intestine (see Chapter 20). Initial treatment consists of small, frequent, lowfat meals in conjunction with fluid restriction and bulking agents. Alkaline reflux gastritis results from the reflux of bile into the gastric remnant. In patients who do not respond to medical therapy for alkaline reflux gastritis, the gastrojejunostomy can be converted to a RouxenY configuration, which diverts the bile further downstream. Dumping syndrome is defined as a constellation of symptoms that include lightheadedness, palpitations, hypoglycemia, and diarrhea that occurs after a meal. Dumping syndrome results from the reduced capacity of the stomach and a dysregulated hormonal response to caloriedense nutrients. Afferent loop syndrome results from obstruction of the afferent limb that prevents emptying of biliary and pancreatic fluid into the stomach. The obstruction, caused by a stricture, kinking of the bowel, adhesions, or narrowing of the anastomosis (due to recurrent ulcer or malignancy), may lead to bowel ischemia, pancreatitis, or cholangitis. Roux stasis syndrome occurs after RouxenY reconstruction and manifests as nausea, vomiting, early satiety, and abdominal pain. Prokinetic agents, anti emetics, and limiting use of narcotics may improve symptoms. Mechanical obstruction of the Roux limb should be ruled out; such mechanical obstructions can occur from adhesions, intussusception, or internal hernia. WeightLoss Surgery Clinical Vignette A 45yearold man with morbid obesity, diabetes mellitus, hypertension, and dyslipidemia presents for a routine annual health checkup. He routinely visits a nutritionist but is unable to lose weight despite aggressive dietary modifications. The pouch is then connected to a jejunal limb to create a gastrojejunal anastomosis. Weight loss occurs due to the restrictive nature of the gastric pouch as well as intestinal malabsorption. There is no nutrient absorption within the Roux limb, and caloric and nutrient absorption can be further reduced by creating a longer Roux limb. A longer Roux limb portends greater malabsorption; thus, patients need lifelong micronutrient and vitamin supplementation. Because the procedure has no malabsorptive properties and is solely restrictive, patients who continue on a soft, liquid, highcaloric diet may not lose weight despite a restricted gastric capacity. Prior to bariatric surgery, patients must have attempted and failed prior weightloss programs, including strict compliance with a lowcalorie diet as well as an aggressive exercise program. Mental illness and the inability to cope can be contraindications to a weight loss procedure. Intrinsic factor, the peptide necessary for intestinal absorption of vitamin B12, is synthesized by the parietal cells of the stomach. The tumor does not involve lymph nodes or invade vascular structures or distant organs. A conventional Whipple resection involves resection of the head and uncinate process of the pancreas, distal third (antrum and pylorus) of the stomach, duodenum, gallbladder, and distal bile duct.
© 2025 Adrive Pharma, All Rights Reserved..