General Information about Fulvicin
Fulvicin is available in several forms, including oral tablets, capsules, and topical creams. The dosage and length of therapy depend on the sort and severity of the fungal an infection. It is important to follow the directions of a healthcare professional when using Fulvicin to ensure the best possible end result.
Like any treatment, Fulvicin could trigger unwanted effects in some individuals. These can include stomach upset, headache, dizziness, and pores and skin rash. It is beneficial to talk with a doctor if these unwanted facet effects turn into extreme or persist for an extended period.
Fungal infections are a standard drawback that affect many individuals, inflicting discomfort and irritation to the affected areas. These infections, also called mycoses, can occur on the skin, hair, and nails, and could be caused by quite so much of fungal species. Fulvicin, also identified as griseofulvin, is an antifungal antibiotic that is used to treat mycoses of the pores and skin, hair, and nails. Let's take a closer take a glance at this medicine and how it works to struggle against fungal infections.
Fulvicin belongs to a bunch of antibiotics known as antifungals, which are particularly designed to treat fungal infections. It is primarily used to deal with infections brought on by fungi of the Trichophyton, Microsporum, Epydermophyton, and Achorionum species. These fungi are responsible for situations corresponding to favus, trichophytosis, microsporia of a pilar part of the top, microsporia of clean pores and skin, dermatomycosis of beard and moustaches, epidermophitia of easy skin, inguinal epidermophitia, and onychomycosis.
Fulvicin works by inhibiting the growth and reproduction of fungi. It does this by interfering with the synthesis of fungal cell walls and the formation of the mitotic spindle, an integral a half of the cell division process. This disruption of the cell wall and mitotic spindle results in the death of fungal cells, permitting the an infection to be treated successfully.
In addition, Fulvicin additionally interferes with the manufacturing of proteins in fungal cells by disrupting their capability to link with template-RNA. This is essential as a outcome of proteins are essential for the survival and performance of cells. Without the flexibility to produce proteins, fungal cells turn into vulnerable and unable to operate, leading to their eventual demise.
In conclusion, Fulvicin is a potent antifungal antibiotic that is highly effective in treating a wide range of fungal infections. Its capability to interfere with the production and performance of fungal cells makes it a dependable treatment choice for many fungal infections of the pores and skin, hair, and nails. With correct utilization and underneath the steerage of a healthcare skilled, Fulvicin might help alleviate the discomfort and irritation caused by fungal infections.
Not solely does Fulvicin goal fungal cells, however it additionally suppresses the division and development of fungal cells in the metaphase stage of cell division. This is an important step in the reproduction of fungi, as it is liable for the formation of new cells. By inhibiting this course of, Fulvicin successfully stunts the expansion and spread of fungal infections.
However fungus gnats on indoor plants buy fulvicin 250 mg amex, the effect is small, occurs at ranolazine concentrations more than 5-fold higher than do therapeutic effects, and can be assessed in the absence of fatty acid oxidation (Belardinelli et al. The last effect is stronger than that seen after administration of nitrovasodilators and partially explained by (reflex) tachycardia. Experimental and clinical studies indicated that nicorandil has cardioprotective effects (Matsubara et al. Nicorandil is rapidly absorbed after sublingual or oral administration and has a short t1/2 (1 h), which does not provide relevant trough levels at the usual regimen of twice-daily dosing at 20 mg/dose. Numerous small studies provided evidence for the efficacy of the compound to reduce angina and increase exercise tolerance, particularly in patients with diabetes and heart failure. However, differences did not extend to Ca2+ channel blockers other than nifedipine. Of note, no significant differences were observed in outcome between long-acting nitrates, Ca2+ channel blockers, and blockers. Concurrent administration of nitrates also can alleviate the increase in coronary vascular resistance associated with blockade of adrenergic receptors. They can therefore be well combined with all other antianginal drugs where permitted. Because nitrates primarily reduce preload, whereas Ca2+ channel blockers reduce afterload, the net effect on reduction of O2 demand should be additive; however, excessive vasodilation and hypotension can occur. The latter diagnosis is essentially based on the presence or absence of increases in plasma levels of cardiac troponin (I or T). The most important interventions are as follows: · Antiplatelet agents, including aspirin and thienopyridines. Nitrates are useful in reducing vasospasm and in reducing myocardial O2 consumption by decreasing ventricular wall stress. If coronary vasospasm is present, intravenous nitroglycerin is likely to be effective, although the addition of a Ca2+ channel blocker may be required to achieve complete control in some patients. The mainstay in these patients is immediate reperfusion by primary angioplasty and stenting or, in the absence of invasive options, fibrinolytic therapy. These patients have a better long-term prognosis and benefit less from early invasive procedures and intensified antiplatelet therapy. Interestingly, neither intensive treatment of diabetes mellitus nor antihypertensive therapy appears to alter the progression of symptoms of claudication. However, the effects of pentoxifylline on lower extremity claudication appear to be modest and not sufficiently supported by prospective evidence (Salhiyyah et al. Milrinone therapy was associated with an increase in sudden cardiac death, and the oral form of the drug was withdrawn from the market. However, the long-term efficacy of intracoronary stents is limited by subacute luminal restenosis within the stent, which, in bare metal stents, occurs in 20%30% of patients during the first 69 months of follow-up (Montalescot et al. Local antiproliferative therapies at the time of stenting have been explored over many years; several drug-eluting stents and, more recently, biodegradable stents have been introduced in the market. The drugs currently used in intravascular stents are paclitaxel, sirolimus (rapamycin), and the two sirolimus derivatives everolimus and zatarolimus. Paclitaxel and sirolimus differ markedly in their mechanisms of action but share common chemical properties as hydrophobic small molecules. Many patients with advanced peripheral arterial disease are more limited by the consequences of peripheral ischemia than by myocardial ischemia. The painful symptoms of peripheral arterial disease in the lower extremities (claudication) typically are provoked by exertion, with increases in skeletal muscle O2 demand exceeding blood flow that is impaired by proximal stenoses. When flow to the extremities becomes critically limiting, peripheral ulcers and rest pain from tissue ischemia can become debilitating. The inhibition of cellular proliferation by paclitaxel and sirolimus or derivatives not only affects vascular smooth muscle cell proliferation but also attenuates the formation of an intact endothelial layer within the stented artery and thereby markedly reduces the rate of restenosis compared with bare metal stents. Dual antiplatelet therapy (aspirin, typically with clopidogrel) is recommended for one year after intracoronary stenting with drug-eluting stents, similar to bare metal stents. Quantitative analysis of vascular to cardiac selectivity of L- and T-type voltage-operated calcium channel antagonists in human tissues. Collateral and collateral-adjacent hyperemic vascular resistance changes and the ipsilateral coronary flow reserve. Prognostic value of dipyridamole stress cardiovascular magnetic resonance imaging in patients with known or suspected coronary artery disease. The bioavailability and pharmacokinetics of slow release nifedipine during chronic dosing in volunteers. Selective inhibition of myocardial contractility by competitive divalent Ca++ antagonists (iproveratril, D 600, prenylamine) [in German]. Selectivity scale of calcium antagonists in the human cardiovascular system based on in vitro studies. Use of nicorandil is associated with increased risk for gastrointestinal ulceration and perforation-a nationally representative population-based study. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Attenuation of anti-ischemic efficacy during chronic therapy with nicorandil in patients with stable angina pectoris. Trimetazidine, a metabolic modulator, has cardiac and extracardiac benefits in idiopathic dilated cardiomyopathy. Treatment with the 3-ketoacyl-CoA thiolase inhibitor trimetazidine does not exacerbate whole-body insulin resistance in obese mice. Direct and indirect effects of calcium entry blocking agents on isovolumic left ventricular relaxation in conscious dogs.
It is recommended that dosage in patients with moderate-to-severe liver disease should be reduced to approximately 20%30% of the usual dose antifungal meaning fulvicin 250mg buy lowest price, with careful monitoring. In contrast to other adverse responses to quinidine therapy, cinchonism usually is related to elevated plasma quinidine concentrations and can be managed by dose reduction. Studies in the early 20th century identified quinidine, a diastereomer of the antimalarial quinine, as the most potent of the antiarrhythmic substances extracted from the cinchona plant, and by the 1920s, quinidine was used as an antiarrhythmic agent. However, in most patients with congestive heart failure, quinidine is well tolerated, perhaps because of its vasodilating actions. Quinidine prolongs refractoriness in most tissues, probably as a result of both prolongation of action potential duration and Na+ channel blockade. In intact animals and humans, quinidine also produces adrenergic receptor blockade and vagal inhibition. Thus, the intravenous use of quinidine is associated with marked hypotension and sinus tachycardia. Quinidine undergoes extensive hepatic oxidative metabolism, and approximately 20% is excreted unchanged by the kidneys. Concentrations of unbound 3-hydroxyquinidine equal to or exceeding those of quinidine are tolerated by some patients. Other metabolites are less potent than quinidine, and their plasma concentrations are lower; thus, they are unlikely to contribute significantly to the clinical effects of quinidine. Some of this variability may be assay dependent because not all assays exclude quinidine metabolites. In patients with advanced renal disease or congestive heart failure, quinidine clearance is decreased only modestly. Diarrhea usually occurs within the first several days of quinidine therapy but can occur later. Occasional cases occur at low dosages, often in patients with renal dysfunction, because sotalol is eliminated by renal excretion of unchanged drug. The other adverse effects of sotalol therapy are those associated with adrenergic receptor blockade (see previous discussion and Chapter 12). Vernakalant Vernakalant is an inhibitor of multiple ion channels and prolongs atrial refractory periods without significantly affecting ventricular refractoriness. Intravenous vernakalant has modest efficacy in terminating atrial fibrillation (Roy et al. Inhibition of P-glycoprotein-mediated drug transport: a unifying mechanism to explain the interaction between digoxin and quinidine. Flecainide acetate prevents recurrence of symptomatic paroxysmal supraventricular tachycardia. Genetic and molecular basis of cardiac arrhythmias: impact on clinical management. Advantages of beta blockers versus antiarrhythmic agents and calcium antagonists in secondary prevention after myocardial infarction. Sex differences in cardiac electrophysiology and clinical arrhythmias: epidemiology, therapeutics, and mechanisms. Pulmonary Hypertension Classification Pulmonary hypertension is a primary disorder of the pulmonary vasculature and a complication of other cardiopulmonary, vascular, and inflammatory diseases. Hence, inhalational delivery of therapeutic compounds can directly target the lung vasculature and pulmonary circulation, limit systemic side effects, and preferentially affect well-ventilated parts of the lung to improve ventilation-perfusion matching (see Chapter 40). This group of patients is the most well-studied subset and the primary target of available therapeutics (Frumkin, 2012). Mechanisms of Pulmonary Arterial Hypertension Pulmonary arterial hypertension is thought to arise from pathophysiological changes in the small pulmonary arteries and arterioles. In addition, ion channels, particularly Ca2+-permeable cation channels and K+-permeable channels. Sequential combination therapy with the addition of separate classes of medications is often utilized for severe or progressive disease (Ghofrani and Humbert, 2014). Modest effects with single agents may be enhanced with the use of up-front combinations and could lead to more dramatic improvements in both symptoms and hemodynamics (Sitbon et al. In patients with no functional limitation, there is no specific therapy that has shown benefit in clinical trials. Alternatively, combination therapy using multiple agents has been shown to be effective in small clinical trials and one phase 3 clinical trial combining ambrisentan and tadalafil. The drug is rapidly absorbed and reaches a peak plasma concentration 1 h after oral administration. Both the parent compound and the major metabolite are highly bound to plasma proteins (96%) (Cockrill and Waxman, 2013). Clearance is reduced in the elderly (>65 years), leading to an increase in area-under-the-curve values for the parent drug and the N-desmethyl metabolite. The mean reduction in the bioavailability of sildenafil (80 mg three times a day) when coadministered with epoprostenol was 28% (Cockrill and Waxman, 2013). Subcutaneous treprostinil has similar efficacy to intravenous formulations of epoprostenol and treprostinil (Simonneau et al. Endothelin 1 was discovered as a potent, endo- Iloprost Clinical Use, Adverse Effects and Precautions. The effects of a single inhalation decline to baseline over 60120 min, and current dosing strategies suggest 69 inhalations daily.
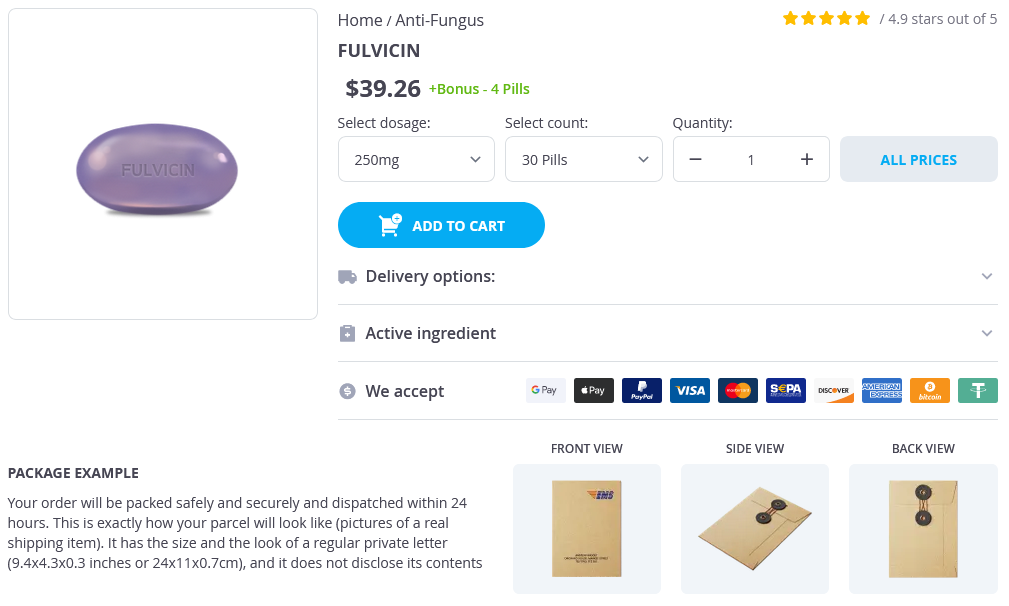
Fulvicin Dosage and Price
Fulvicin 250mg
- 30 pills - $43.62
- 60 pills - $68.21
- 90 pills - $92.79
- 120 pills - $117.38
- 180 pills - $166.55
- 270 pills - $240.31
- 360 pills - $314.06
Usually fungus gnats cannabis coco 250 mg fulvicin, only short-term treatment with adrenergic receptor antagonists or Ca2+ channel blockers is required, 26 weeks, and it should be discontinued once the patient is euthyroid. The B-lymphocytedepleting agent rituximab, when used with methimazole, prolongs remission of Graves disease. Thyroid storm is an uncommon but life-threatening complication of thyrotoxicosis in which a severe form of the disease is usually precipitated by an intercurrent medical problem. Precipitating factors associated with thyrotoxic crisis include infections, stress, trauma, thyroidal or nonthyroidal surgery, diabetic ketoacidosis, labor, heart disease, and, rarely, radioactive iodine treatment. Thyroid function abnormalities are similar to those found in uncomplicated hyperthyroidism. Treatment includes supportive measures such as intravenous fluids, antipyretics, cooling blankets, and sedation. Oral iodides are used after the first dose of an antithyroid drug has been administered. Because agranulocytosis usually occurs rapidly and is not associated with a gradual reduction in granulocyte count, periodic prospective monitoring of granulocyte count is not generally helpful. Antithyroid drugs are the treatment of choice; radioactive iodine is clearly contraindicated. Both propylthiouracil and methimazole cross the placenta equally, and either may be used safely in the pregnant patient. These agents are anions that resemble iodide: thiocyanate, perchlorate, and fluoroborate, all monovalent hydrated anions of a size similar to that of iodide. Perchlorate can be used to control hyperthyroidism; however, when given in excessive amounts (23 g daily), it has caused fatal aplastic anemia. Perchlorate in doses of 750 mg daily has been used in the treatment of Graves disease, although it is not available in North America. Lithium decreases secretion of T4 and T3, which can cause overt hypothyroidism in some patients taking Li+ for the treatment of mania (see Chapter 16). Thyrotoxicosis in Pregnancy Iodine Iodide is the oldest remedy for disorders of the thyroid gland. In high concentration, iodide can influence several of the important functions of the thyroid gland. Iodide limits its own transport and acutely and transiently inhibits the synthesis of iodotyrosines and iodothyronines (the Wolff-Chaikoff effect) (Pramyothin et al. An important clinical effect of high [I-]plasma is inhibition of the release of thyroid hormone. Adjuvant Therapy Several drugs that have no intrinsic antithyroid activity are useful in the symptomatic treatment of thyrotoxicosis. The effect is exerted directly on the thyroid gland and can be demonstrated in the euthyroid subject as well as in the hyperthyroid patient. The response to iodine in patients with hyperthyroidism is often striking and rapid: Release of thyroid hormone into the circulation is rapidly blocked, and its synthesis is mildly decreased. In the thyroid gland, vascularity is reduced, the gland becomes much firmer, the cells become smaller, and colloid reaccumulates in the follicles as iodine concentration increases. Another use of iodide is to protect the thyroid from radioactive iodine fallout following a nuclear accident or military exposure. A potassium iodide product (Thyroshield) is available over the counter to take in the event of a radiation emergency and block the uptake of radioiodine into the thyroid gland. The adult dose is 2 mL (130 mg) every 24 h, as directed by public health officials. The severity of symptoms of chronic intoxication with iodide (iodism) is related to the dose. Increased salivation, coryza, sneezing, and irritation of the eyes with swelling of the eyelids commonly occur. In addition, the parotid and submaxillary glands may become enlarged and tender, and the syndrome may be mistaken for mumps parotitis. The lesions are bizarre; they resemble those caused by bromism and generally involute quickly when iodide is withdrawn. The chemical behavior of the radioactive isotopes of iodine is identical to that of the stable isotope, 127I. The radiation passes through the tissue and can be quantified by external detection. With properly selected doses of 131I, it is possible to destroy the thyroid gland completely without detectable injury to adjacent tissues. The clearest indication for radioactive iodine treatment is hyperthyroidism in older patients and in those with heart disease. Stable iodide (nonradioactive) may preclude treatment and imaging with radioactive iodine for weeks after the stable iodide has been discontinued. The optimal dose of 131I, expressed amount taken up, varies in different laboratories from 80 to 150 Ci per gram of thyroid tissue. Beginning a few weeks after treatment, the symptoms of hyperthyroidism gradually abate over a period of 23 months. Adrenergic antagonists, antithyroid drugs, or both can be used to hasten the control of hyperthyroidism. The response to these drugs does not seem to be dependent on the presence or absence of specific oncogene mutations. Adverse reactions include palmar-plantar erythrodysesthesia, diarrhea, alopecia, fatigue, weight loss, hypertension, and others. The recommended daily dose of lenvatinib is 24 mg once daily with or without food, reduced to 14 mg in those with severe renal or hepatic impairment.
© 2025 Adrive Pharma, All Rights Reserved..