General Information about Forxiga
Forxiga, additionally identified by its generic name dapagliflozin, is a medicine that has been permitted for the therapy of type 2 diabetes. This medicine is a half of a category of medicine known as sodium-glucose cotransporter 2 (SGLT2) inhibitors, which work by blocking the reabsorption of glucose by the kidneys, thereby rising the amount of sugar excreted within the urine and reducing blood glucose levels.
This is where Forxiga comes into play as a useful remedy choice. It can be used alone or in combination with different diabetes medications to assist management blood glucose ranges in folks with sort 2 diabetes. The drug works by focusing on the kidneys to filter out extra glucose from the blood, thus decreasing the amount of sugar within the body and decreasing the danger of complications.
According to the World Health Organization, international diabetes prevalence has been rising steadily over the previous couple of a long time and is estimated to affect over 422 million individuals worldwide. Type 2 diabetes, particularly, is the most typical type of the disease and is characterized by the body's lack of ability to use insulin properly to control blood sugar levels. Left unmanaged, type 2 diabetes can result in a host of serious problems, including coronary heart disease, nerve damage, kidney failure, and blindness.
However, like any medicine, Forxiga may also have some opposed effects. The commonest unwanted effects include urinary tract infections, increased urination, and genital infections. These antagonistic effects are typically delicate and do not require medical consideration until they persist or turn out to be extra severe.
It is crucial to note that Forxiga is not an various alternative to a wholesome life-style. While it could assist to improve blood sugar management, it shouldn't be used as the only type of treatment for diabetes. To get probably the most out of this medication, it must be used as a half of an general diabetes administration plan that contains a nutritious diet and common physical activity.
If you have a historical past of significant kidney problems or are allergic to dapagliflozin, you ought to not take Forxiga. Pregnant and breastfeeding women must also keep away from this treatment, as there's limited data out there on its safety in these populations.
In conclusion, Forxiga is an efficient and widely used medicine for the administration of type 2 diabetes. It works by targeting the kidneys to reduce glucose levels within the physique, thus lowering the danger of issues related to diabetes. With correct use and beneath the steerage of a healthcare skilled, Forxiga may help enhance the quality of life for individuals living with kind 2 diabetes.
Forxiga is taken orally, usually once a day, with or with out meals. The dosage may range depending on elements such as the affected person's age, medical historical past, and response to remedy. Forxiga is on the market in pill kind, and sufferers are advised to swallow the whole pill with a glass of water and to not crush or chew it.
One of essentially the most important benefits of Forxiga is its ability to advertise weight loss, making it a super remedy for overweight or overweight individuals with type 2 diabetes. It works by lowering the quantity of glucose within the body, which in flip encourages the physique to burn fats as an alternative for power. Coupled with a nutritious diet and train regime, Forxiga could be a powerful device in attaining and sustaining a healthy weight.
The combination of ground-glass opacity and mosaic perfusion constitutes the headcheese sign blood glucose reference range 10 mg forxiga otc. B: Expiratory scan at the same level shows air trapping in the lucent lung regions. Progression of subacute hypersensitivity pneumonitis to fibrosis in a bird fancier. Focal fibrosis is present in the left upper Radiographic Findings On chest radiographs, radiographic findings of fibrosis include irregular reticular opacities that predominate in the middle lung or lower lung zones and may be parahilar, peri bronchovascular, or peripheral in distribution. A: Chest radiograph shows marked reduction in lung volume with poorly defined reticular opacities at the lung bases. B: At the lung bases, irregular reticular opacities indicative of fibrosis, and areas of mosaic perfusion predominate. Traction bronchiectasis is visible bilaterally, with a patchy and parahilar predominance (arrows). B: At the lung bases, areas of fibrosis (arrows) are patchy and lack the subpleural predominance of idiopathic pulmonary fibrosis. Although similar findings can Eosinophilic lung disease with a known cause Drugs Parasitic disease and tropical pulmonary eosinophilia Fungi Bronchocentric granulomatosis be seen in association with a number of etiologic agents, particularly parasites and drugs, use of the term simple pul monary eosinophilia should be limited to cases in which the cause is unknown. Patients typically have cough and mild shortness of breath; often a history of asthma or atopic disease is present. Pathologically, eosinophils and histiocytes accumulate in the alveolar walls and alveoli. Chronic eosinophilic pneumonia is usually associated with increased eosinophils in the peripheral blood. Clinically, patients present with fever, cough, weight loss, malaise, and shortness of breath. These conditions reflect a spectrum, being associated with symptoms ranging from mild to severe and radiographic abnormalities ranging from focal to diffuse. Other idiopathic diseases also may be associated with blood or tissue eosinophilia and may be considered in the differential diagnosis of eosinophilic lung disease. They are sometimes included in a category of eosinophilic lung disease with angiitis. A: Chest radio graph shows patchy consolidation with an upper lobe and peripheral predominance. Radiographically, chronic eosinophilic pneumonia is characterized by the presence of homogeneous peripheral air-space consolidation, "the photographic negative of pul monary edema'. This pattern can remain unchanged for weeks or months unless steroid therapy is given; chronic eosinophilic pneumonia responds promptly to the administration of steroids. The combination of blood eosinophilia, peripheral con solidation visible on radiographs, and rapid response to steroid therapy is often sufficiently characteristic to obviate the need for lung biopsy. The diagnosis may be difficult in patients with minimal blood eosinophilia or those in whom the peripheral distribution of infiltrates is not apparent. Simple pulmonary eosinophilia, however, is usually self-limited and associated with pulmonary infiltrates that are transient or fleeting. With simple pulmonary eosinophilia, areas of consolidation can appear and disappear within days; chronic eosinophilic pneumonia has a more protracted course, and areas of consolidation remain unchanged over weeks or months. The presence of peripheral air-space consolidation can be considered suggestive of chronic eosinophilic pneumonia in the appropriate clinical setting. This appearance mimics that of organizing pneumonia/bronchiolitis obliterans organizing pneumonia. The diagnosis is based on clinical findings of acute respiratory failure and the presence of markedly elevated numbers of eosinophils in bronchoalveolar lavage fluid. Response to steroids is prompt and the prognosis is good, with no residual disability. The earliest radiographic manifestation is reticular opacities, frequently with Kerley B lines. This progresses over a few hours or days to bilateral interstitial opacities and air-space consolidation involving mainly the lower lung zones. The main causes of morbidity and mortality are cardiac and central nervous system involvement. The radiographic manifestations are nonspecific and consist of transient hazy ground-glass opacity or areas of consolidation. Cardiac involvement eventually leads to car diomegaly, pulmonary edema, and pleural effusion. Churg-Strauss Syndrome Churg-Strauss syndrome (also known as Churg-Strauss granulomatosis or allergic granulomatosis and angiitis) is a multisystem disorder characterized by the presence of (1) necrotizing vasculitis, (2) extravascular granuloma forma tion, and (3) eosinophilic infiltration of various organs, par ticularly the lungs, skin, heart, nerves, gastrointestinal tract, and kidneys. Patients with this syndrome are usually middle-aged (average onset 40 to 50 years) and often have a history of allergic diseases, including asthma, nasal polyps, or sinusitis. Criteria for diagnosis include (1) asthma, (2) blood eosinophilia greater than 10%, (3) a history of allergy, (4) neuropathy, (5) migratory or transient pulmo nary opacities visible radiographically, (6) sinus abnor malities, and (7) extravascular eosinophilia on biopsy. The presence of four or more of these criteria is 85% sensi tive and nearly 100% specific for Churg-Strauss syndrome. Pneumomediastinum and right Pneumothorax are present and a right chest tube is in place. Lung abnormalities usually resemble simple pulmo nary eosinophilia or chronic eosinophilic pneumonia.
Dur ing the compensated phase of aortic regurgitation diabetes insipidus koira discount forxiga 5 mg free shipping, the effec tive stroke volume remains in the normal range. This suggests that this approach is useful for follow-up and monitoring response to therapy in patients with aortic regurgitation. Mag nitude (top) and phase (bottom) images in systole (left) and diastole (right). Note that on the ow ow phase images antegrade ow in systole is represented by bright voxels, whereas retrograde (aortic regurgitation) in diastole is represented by dark voxels in the ascending aorta. B: A versus time curve derived from image pairs at 16 phases of the cardiac cycle shows negative values (retrograde ow) in diastole. The area under the curve with negative values is the volume of aortic regurgitation. Chapter 32 Valvular Heart Disease 777 congenital valvular, subvalvular (parachute mitral valve), or supravalvular stenoses; left atrial myxoma; and exuberant mitral annular calcification. Mitral stenosis often is accom panied by a variable degree of mitral regurgitation. Mitral stenosis causes elevated left atrial pressure through out diastole, and pulmonary venous hypertension produces pulmonary arterial hypertension. In long-standing mitral stenosis, pulmonary arterial hypertension may be severe, and pulmonary regurgitation eventually ensues across a dilated pulmonary annulus. The right ventricle eventually dilates, causing tricuspid regurgitation from a dilated annulus. Associated mitral regurgitation appears as a signal void pro jected into the left atrium during systole. Likewise, signal voids may be recognized in right-sided cardiac chambers if there is any associated pulmonary or tricuspid regurgitation. Radiography the chest x-ray provides good insight into the severity of mitral stenosis by showing the relative severity of pulmo nary venous hypertension (see Table 30-8 in Chapter 30). In mild disease, there may be only equalization or reversal of the diameter of upper and lower lobe pulmonary vessels (cephalization). In more severe disease or with an imposed hypervolemic state, interstitial pulmonary edema or alveolar pulmonary edema becomes evident. Interlobular septal thick ening (Kerley B lines) usually is a sign of interstitial edema but may become permanent as a consequence of fibrosis or deposition ofhemosiderin after multiple episodes of pulmo nary edema. Rarely, high-density nodules (ossific nodules) in the lower lobes may be a consequence ofmultiple episodes of alveolar pulmonary edema and hemorrhage. In compensated mitral stenosis, only mild cardiomegaly or normal heart size is seen. The left atrium invariably is enlarged, causing a right retrocardiac double density. A con vexity on the upper left cardiac border in the frontal view indicates enlargement of the left atrial appendage. Enlargement of the pulmonary arterial segment and right heart indicates pulmonary arterial hypertension. Enlarge ment of the right heart in the absence of pulmonary arte rial enlargement usually indicates concomitant rheumatic tricuspid regurgitation. The ascending aorta and aortic arch are characteristically small in isolated mitral valve disease. Even slight prominence of the thoracic aorta should raise suspicion of associated rheumatic aortic valve disease. A: Phase (velocity) image acquired in a plane perpendicular to the direction of ow across a stenotic mitral valve. This area is interrogated for the peak velocity during diastole to estimate the pressure gradient using the modi ed Bernoulli equation (peak gradient slightly lower than the peak velocity measured by Doppler echocardiography. Prolapse is ballooning of the middle of the valve beyond the annulus during systole; the tips of the leaflets to which the chordae attach do not pass beyond the annulus. Flail is indicated by passage of the tips of the mitral leaflets beyond the annulus and into the left atrium during systole. The dys function may involve one or more of several components: leaflets, chordae, anterior and posterior papillary muscles, or annulus. Pulmonary venous hypertension or edema usually is less severe than with mitral stenosis. Pulmonary arterial hypertension is less common and less severe than with stenosis. Acute onset of mitral regurgitation such as might occur with chordal or papillary muscle rupture imposes sudden onset of pulmonary venous hypertension with no time for compensating mechanisms to become operative. It has been noted that rupture of the posterior papillary muscle or chordae supported by it may cause pulmonary edema confined to or more severe in the right upper lobe. In the absence of myocardial failure, the degree of cardiomegaly bears a rough relation to the sever ity of regurgitation. Signs of pulmonary venous and arterial hypertension are less prominent than with mitral stenosis. Nonrheumatic causes of mitral regurgitation usually do not cause radiographically discernible enlargement of the left atrial appendage. Acute onset of mitral regurgitation is characterized by pulmonary edema with a normal heart size. Rupture of the posterior papillary muscle or associated chordae may cause focal or more severe pulmonary edema of the right upper lobe. Mitra/ Valve Prolapse Mitral valve prolapse is observed on about 5% of left ventriculograms. Pathologically, it is caused by myxoma tous degeneration of the mitral valve leaflets and chordae tendineae. However, one complication that may occur-rupture of a chordae tendineae-can induce severe regurgitation.
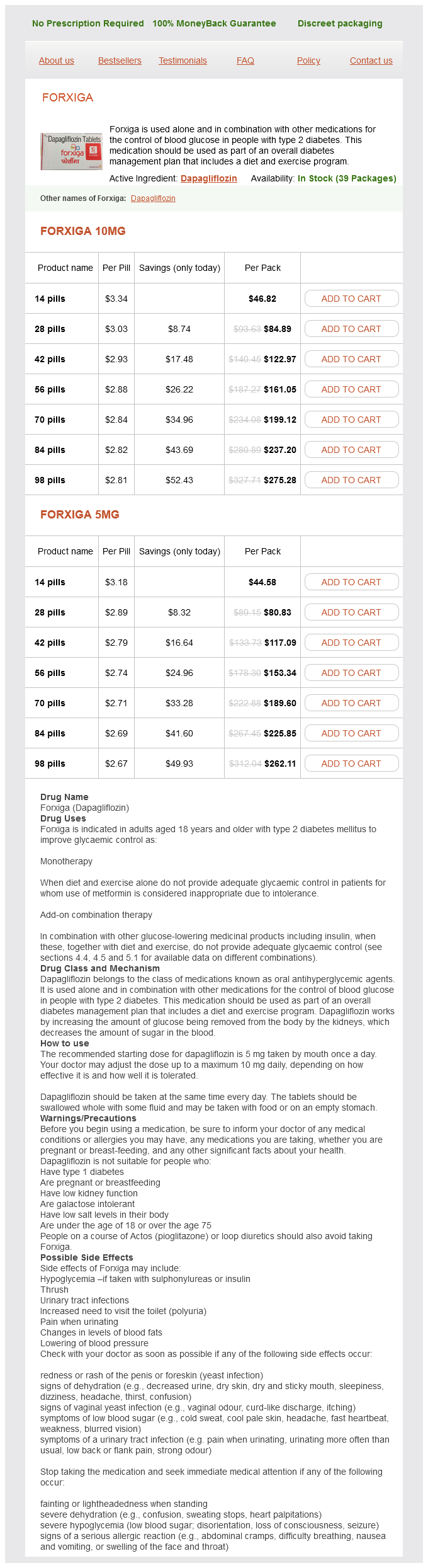
Forxiga Dosage and Price
Forxiga 10mg
- 14 pills - $46.82
- 28 pills - $84.89
- 42 pills - $122.97
- 56 pills - $161.05
- 70 pills - $199.12
- 84 pills - $237.20
- 98 pills - $275.28
Forxiga 5mg
- 14 pills - $44.58
- 28 pills - $80.83
- 42 pills - $117.09
- 56 pills - $153.34
- 70 pills - $189.60
- 84 pills - $225.85
- 98 pills - $262.11
The tube tip position relative to the carina is not critical diabetes signs baby discount forxiga 5 mg with mastercard, because this is determined by the location of the tracheostomy stoma. Tracheostomy tubes that are angled relative to the tracheal lumen may cause erosion of the tracheal wall, with perforation or subsequent tracheal stenosis, or may occasionally fall out. A: Chest radiograph shows an endotracheal tube with its tip (white arrow) about 3 cm above the carina. B: On a subsequent radiograph, the chin is visible overlying the lower cervical spine, indicating the neck is in a neutral position or slightly flexed. The endotracheal tube tip (white arrow) has migrated downward, and is a few mm above the carina. The endotracheal tube (black arrows) extends into the proximal left main bronchus. Complications of venous puncture include laceration of the subclavian or carotid artery. The tube balloon (small arrows) is overinflated and at the level of the piriform sinuses. C = tube (large white arrow) does not overlie the shadow of the trachea (small white arrows). Below the level of the tube tip, the esophagus (black arrows) is dilated and air-filled. Because many catheters have two or three lumens, each with a different orifice, the catheter tip should be as near to the azygos arch as possible. This position allows each orifice, which may be as much as 5 cm proximal to the tip, to be dis tal to the last venous valve. It usually is not desirable to place a catheter in the right atrium; this may result in dysrhythmia or injection of undi luted toxic drugs into the heart. Chest radiograph following attempted bilat eral subclavian and internal jugular vein catheter place ment. A large mass at the right apex represents an extrapleural hematoma due to laceration of the right carotid artery. Bilateral pneumothoraces (white arrows) also are pres ent, with mediastinal shift to the left. This occurs most often with catheters placed via the left subdavian vein or left internal jugular vein. Catheters may inadvertently extend into smaller veins, increasing the risk of inaccurate pressure measurements, thrombosis, or perforation. Because the artery is superior to the vein, it may be seen above the clavicle or overlying the aortic arch. A catheter taking an unusual course may be free within the mediastinum or pleural space rather than within a vein, and fluids should be administered with care. Improperly placed catheters sometimes can be sheared off at the needle tip and embolize to the heart or pulmonary arteries. Improper technique may lead to air embolism, with air visible in the pulmonary artery. A right internal jugular catheter Swan-Ganz catheters are double-lumen, balloon-tipped (black arrow) follows an unusual course and is directed laterally (white arrows) at catheters allowing measurement of pulmonary arterial and wedge pressures when the balloon is inflated. Normally the tube tip should lie within a large central pulmonary artery; with inflation of the balloon, the tube tip migrates distally to a wedged position. A catheter positioned in a main or (text continues on page 372) a level above the clavicle (and the subclavian vein). B: the veins shown in the internal jugular and subclavian veins (A) are localized relative to important landmarks visible on chest radiographs. The last valves in (white arrows) are located near the inner aspects of the first ribs (outlined in white). The cavoatrial junction is near the point the vena cava crosses the bronchus intermedius. A: A dialysis catheter (arrows) enters the azygos arch with it distal tips directed medially and upward. B: On a lateral view, the distal cath eter tips are directed posteriorly into the azygos arch (arrows). B: Typical course of the left superior intercostal vein (arrows) relative to other mediastinal veins. A: A left internal jugular venous catheter (white arrows) descends along the left mediastinum. However, this catheter position also may be e:xtravascular or in a small mediastinal vein. A peripherally placed right venous catheter (small arrows) is visible in the typi cal location of the subclavian vein, beneath and overlying the clavicle. A venous catheter (arrows) was sheared off during insertion and has embo lized to the left pulmonary artery. Coiling can result in knotting or sudden peripheral migration of the catheter with wedging. If the catheter lies in a small (lobar or segmental) artery, it may remain wedged with the balloon uninflated, and thrombosis and pul monary infarction or pulmonary artery aneurysm can result. Care also must be taken that the balloon does not Transvenous pacemaker and implanted defibrillator leads vary in number and location in different patients. Placement of the tip into the coronary sinus usually results in a superior and posterior deviation of the pacemaker lead. A: A patient with cardio megaly shows a peripherally located (segmental or subsegmental) Swan-Ganz catheter (arrow). B: Following withdrawal of the catheter 1 day later, a focal opacity representing a lung infarction is visible in the right lung (arrow).
© 2025 Adrive Pharma, All Rights Reserved..