General Information about Finast
So, how precisely does finasteride work? In order to understand its mechanism of action, it is important to understand the position of DHT in hair loss. DHT is a byproduct of testosterone, the male hormone responsible for masculine traits and bodily functions such as intercourse drive and sperm production. While DHT is important for the event of male traits during puberty, it can also bind to hair follicles on the scalp and trigger them to shrink, resulting in hair thinning and eventual hair loss.
One of the principle benefits of finasteride is its ability to stop further hair loss and even stimulate new hair development in areas the place thinning has occurred. Clinical research have shown that finasteride can considerably increase the number of hairs in a given space of the scalp and improve hair density in males with male sample baldness. This makes it an attractive remedy possibility for these who wish to not solely stop hair loss but also regrow their hair.
Finasteride is usually taken in tablet kind, with a really helpful daily dose of 1mg. It is necessary to note that this medication is only suitable for males and isn't really helpful for use by ladies or children. It is also essential to consult a health care provider before starting finasteride, as it might interact with certain drugs or have side effects similar to decreased libido and erectile dysfunction in some individuals.
This is the place finasteride is obtainable in. By inhibiting the manufacturing of DHT, finasteride successfully slows down the progressive miniaturization of hair follicles and promotes hair progress. It does this by blocking the motion of an enzyme called 5-alpha reductase, which converts testosterone to DHT in hair follicles. As a outcome, finasteride reduces the levels of DHT in the scalp by as a lot as 60%, permitting hair follicles to get well and resume their normal progress cycle.
In conclusion, finasteride is a extensively used and efficient medication for treating hair loss in males. It works by inhibiting the manufacturing of DHT, a hormone that performs a key role in male pattern baldness. By decreasing DHT levels in the scalp, finasteride prevents further hair loss and can even stimulate new hair growth. However, you will want to consult a well being care provider before beginning finasteride and to understand that it isn't a remedy for baldness. With its confirmed observe report and minimal unwanted effects, finasteride remains a preferred and trusted choice for those battling hair loss.
Additionally, finasteride is a safe and well-tolerated treatment, with few reported unwanted effects. Its success rate in treating male sample baldness has been persistently high, with many males reporting vital enhancements in hair progress after taking finasteride for a number of months. However, it could be very important note that results might vary from person to person, and it might take up to 6 months to see seen changes in hair development.
Finast, quick for finasteride, is a extremely effective treatment used to treat hair loss in men. It belongs to a class of drugs known as 5-alpha reductase inhibitors, which work by blocking the conversion of testosterone to dihydrotestosterone (DHT) within the body. DHT is a hormone that plays a key position in male pattern baldness, making finasteride a popular and successful treatment possibility for these struggling with hair loss.
The complexity of the injury has implications for subsequent facial reconstruction (Video 30 hair loss in men 91 buy finast 5 mg line. The mobile segment consists of the palate, the alveolar process and the lower thirds of the pterygoid plates. From the nasal bridge, the fracture enters the medial wall of the orbit to involve the lacrimal bone and then crosses the inferior orbital rim, usually at the junction of the medial third and lateral twothirds, and often involves the infraorbital foramen. The fracture line then runs beneath the zygo maticomaxillary suture, traversing the lateral wall of the maxillary sinus to extend posteriorly and horizontally across the pterygoid plates. The orbit may also be involved in fractures of the frontal bone and extensive nasal complex injuries. This protective mechanism of injury helps to maintain the integrity of the globe itself in preference to the orbital walls. Fortunately, the optic foramen, which is situated within the lesser wing of the sphenoid bone, is surrounded by dense bone and is only rarely involved in fractures. The fracture extends through the nasal base and continues pos teriorly across the ethmoid bone. The fracture then crosses the lesser wing of the sphenoid and, on occasion, involves the optic foramen. Usually, however, it slopes down medially, passing below the optic foramen to reach the pterygomaxillary fissure and pterygopalatine fossa. From the base of the inferior orbital fissure, the fracture runs later ally and upwards, separating the greater wing of the sphenoid from the zygomatic bone, to reach the frontozygomatic suture. It also extends Lower third of face (mandible) the mandible is essentially a tubular bone bent into a blunt V shape (Ch. This basic configuration is modified by sites of muscle attach ment, principally masseter and medial pterygoid at the angle, and temporalis at the coronoid process. The presence of teeth, particularly those with long roots such as the canines, or of unerupted teeth pro duces lines of weakness in the mandible. When the teeth are lost or fail to develop, the subsequent progressive resorption of the alveolar bone means that the mandible reverts to its underlying tubular structure. This injury demonstrates several complicated levels of Le Fort type maxillary fracture. There are also bilateral condylar neck fractures and a mandibular symphysial fracture (light blue arrows). Note the avulsed lower left premolar and dental fracture of the right incisor (yellow arrows). The aim of surgery is to reconstruct anatomy in order to provide a scaffold on which to overlay the soft tissues. In this case, navigation planning takes the normal green right side and mirrors to the left. There is obvious herniation of orbital contents and disruption of the soft tissue contents of the orbit. Again, like all tubular bones, the mandible has great resistance to compressive forces, but fractures at sites of tensile strain. It is liable to particular patterns of distribution of tensile strain when forces are applied to it. Anterior forces applied to the mental symphysis, or over the body of the man dible, lead to strain at the condylar necks and also along the lingual cortical plates on the contralateral side in the molar region. The man dible therefore often fractures at two sites and isolated fractures are relatively unusual. In order of frequency, fractures occur most com monly at the neck of the condyle, the angle, the parasymphysial region and the body of the mandible. Alternatively, if this membrane remains intact, it may be seen as blue and bulging (haemotympanum). The surgical disarticulation of the craniofacial skeleton has been used to gain access to otherwise inaccessible sites in order to allow the surgeon to attend to pathology in the skull base, cervical spine and anterior and posterior cranial fossae. The aim is to provide increased and more direct exposure of both the pathology and the adjacent vital structures without the need to resect uninvolved structures. The craniofacial skeleton can be divided into a series of modular osteotomies, which permit both independent and conjoined mobilization. The zygomatic and nasal bones and the maxilla may be exposed and mobilized, and pedicled on the overlying soft tissues either unilaterally or bilaterally. These approaches improve access to the nasal cavity, maxillary, ethmoidal and sphenoidal sinuses, the soft palate and nasopharynx, and the infratemporal fossa and pharyngeal space. The exposures may be extended to gain access to the anterior and middle cranial fossae, cavernous sinus, clivus, craniocervical junction and upper cervical vertebrae. A variety of different access osteotomies have been described and found to be useful in specific clinical situations. Most of the osteot omies described follow the conventional patterns of facial fractures described above. The osteotomy is completed by dividing the upper alveolus and palate just to the side of the nasal septum and perpendicular plate of the vomer. The maxilla may be mobilized at the Le Fort I level and downfractured, pedicled on the palatoglossal muscles and soft tissue attachments. This gives good access to the nasopharynx, clivus and upper cervical spine, par ticularly if the palate is divided in the midline. Lateral zygomatic osteotomies may be performed to gain access to the orbital apex and infratemporal fossa.
Trauma hair loss testosterone finast 5 mg purchase overnight delivery, such as persistent lip biting, results in scarring of the overlying oral mucosa and obstruction of the small drainage duct. When trauma occurs in the floor of the mouth and obstructs the drainage duct/s of the sublingual gland, the resulting retention cyst is known as a ranula. The palatoglossal glands are mucous glands and are located around the pharyngeal isthmus. The anterior glands are embedded within muscle near the ventral surface of the tongue and open by means of four or five ducts near the lingual frenulum, and the posterior glands are located in the root of the tongue. Serous glands (of von Ebner) occur around the circumvallate papillae; their secretion is watery, and they probably assist in gustation by spread ing taste stimuli over the taste buds and then washing them away. Ducts Intercalated, striated (both intralobular) and extralobular collecting ducts lead consecutively from the secretory endpieces. The lining cells of intercalated ducts are flat nearest the secretory endpiece but become cuboidal. Intercalated ducts function primarily as a conduit for saliva but, together with the striated ducts, may also modify its content of electrolytes and secrete IgA. Striated ducts are lined by a low columnar epithelium and are so called because their lining cells have characteristic basal striations. The latter are regions of highly infolded basal plasma membrane, between which lie columns of vertically aligned mitochon dria. Infolding of the basal plasma membrane and local abun dance of mitochondria are typical features of epithelial cells that actively transport electrolytes. Here, the cells transport potassium and bicarbo nate into saliva; they produce a hypotonic saliva by reabsorbing sodium and chloride ions in excess of water. Striated ducts modify electrolyte composition and secrete IgA, lysozyme and kallikrein. IgA is produced by subepithelial plasma cells and transported transcytotically across the epithelial barrier to be secreted, once it has been dimerized by epithelial secretory component, into the saliva (Garrett et al 1998). This is also a function of serous acinar cells and other secretory epithelia, notably the lactating breast. The intralobular ductal system of the sublingual gland is less well developed than that of the parotid and submandibular glands. Collecting ducts are metabolically relatively inert conduits that run within interlobular connective tissue septa in the glands. They transport saliva to the main duct, which opens on to the mucosal surface of the buccal cavity. It may be pseudostratified columnar, stratified cuboidal or columnar in the larger ducts, and has a distinct basal layer. Solid black arrows indicate the direction of transport of salivary components, and the open white arrow the direction of salivary flow. They extend numerous cytoplasmic processes around serous acini and are often termed basket cells. Myoepithelial cells associated with ducts are more fusiform in shape and are aligned along the length of the duct. Their cytoplasm contains abundant actin microfilaments, which mediate contraction. Although stimulated by the autonomic nervous system, the precise functional role of myoepithelial cells in salivary secretion awaits clari fication (Garrett 1998). Functional studies clearly indicate that myoepi thelial activity can accelerate the initial outflow of saliva, reduce luminal volume, contribute to the secretory pressure, support the underlying parenchyma, reduce backpermeation of fluid and help salivary flow to overcome increases in peripheral resistance (although, if this is exces sive, it may lead to sialectatic damage of striated ducts, thereby increas ing overall permeability). Secretion may be continuous but at a low resting level, and may also occur spontaneously. The controlled variation in the activity of the many types of salivary effector cells (serous, sero mucous and mucous secretory cells, myoepithelial cells, epithelial cells of all the ductal elements and the smooth muscle of local blood vessels) affects the quantity and quality of saliva. There is no clear evidence that circulating hormones evoke secretion directly at physiological levels but they may alter the response of glandular cells to neural stimuli. The afferent inputs to the reflex arc pass to brainstem salivatory centres, especially from taste and mechanoreceptors in the mouth. A variety of other sensory modalities in and around the mouth are also involved. The afferent input is integrated centrally by the salivatory centres, which are themselves influenced by higher centres. The latter may provide facilitatory or inhibitory influences, which presumably explains why the mouth becomes dry under stress. The efferent drive to the glands passes via parasympathetic and sympathetic outputs from the centres. Rela tively little is known about the connections of the preganglionic para sympathetic neurones in the salivatory centres, and virtually nothing is known about either the central location of the sympathetic pregangli onic neurones, or the output pathways. Cholinergic nerves often accompany ducts and arborize freely around secretory endpieces, but adrenergic nerves usually enter glands along arteries and ramify with them. The main secretomotor nerves are predominantly unmyelinated axons; the few myelinated axons that have been seen are presumably either preganglionic efferent or visceral afferent. Within the glands, the nerve fibres intermingle, such that cholinergic and adrenergic axons Basal cells A population of basal cells is present in the striated and collecting ducts (Riva et al 1992). They are sparsely distributed in the striated ducts and more densely distributed in the collecting ducts, in which they form a continuous layer as the ducts pass further towards the hilum. A small population of basal cells is found on the abluminal surface of ductal cells associated with both striated and collecting ducts.
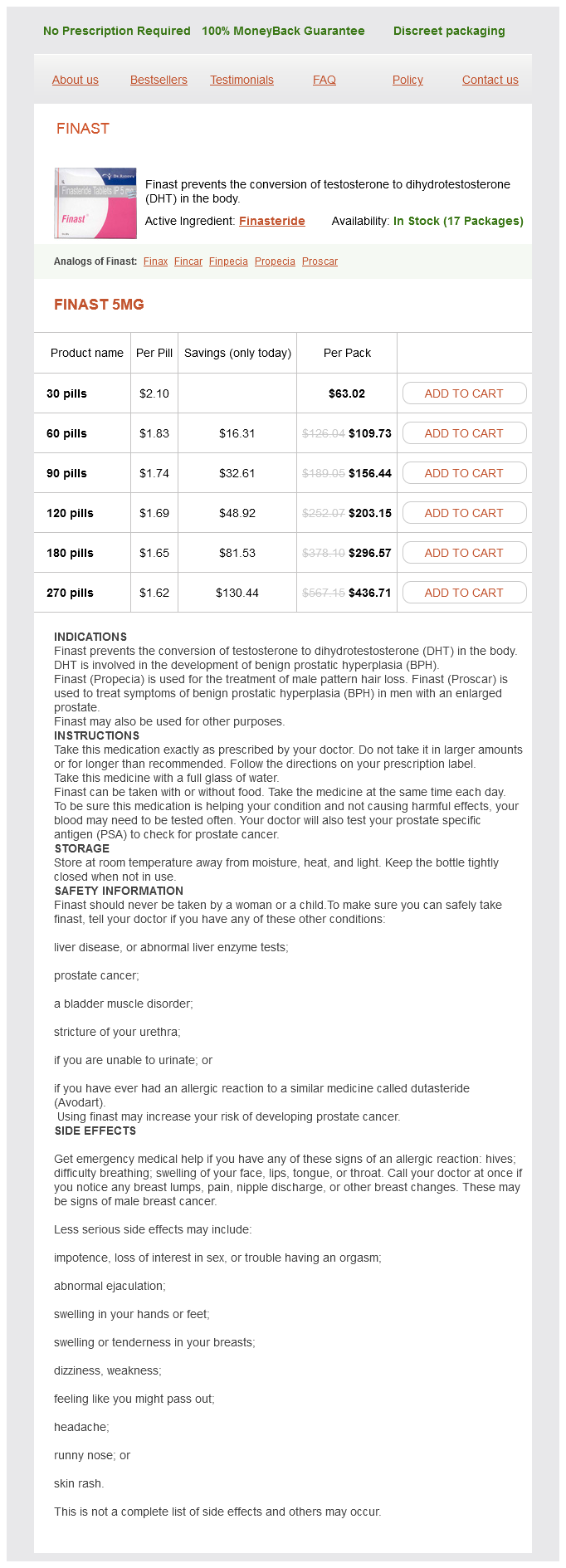
Finast Dosage and Price
Finast 5mg
- 30 pills - $63.02
- 60 pills - $109.73
- 90 pills - $156.44
- 120 pills - $203.15
- 180 pills - $296.57
- 270 pills - $436.71
Vascular supply Levator labii superioris alaeque nasi is supplied by the facial artery and the infraorbital branch of the maxillary artery hair loss cure israel finast 5 mg buy low price. Innervation Levator labii superioris alaeque nasi is innervated by zygomatic and superior buccal branches of the facial nerve. Actions the lateral slip raises and everts the upper lip and raises, deepens and increases the curvature of the top of the nasolabial furrow. The medial slip pulls the lateral crus superiorly, displaces the circumalar furrow laterally, and modifies its curvature; it is a dilator of the naris. Depressor septi and the medial slip of levator labii superioris alaeque nasi are sometimes described as secondary nasal dilators; there is little evidence that either of these muscles has any direct influence on the nasal valve. It is wider below than above, and widest and vertically deepest in its central region, where it is divided by a vertical, midline, osseocartilaginous septum. The nasal cavity communicates with the paranasal sinuses and opens into the nasopharynx through a pair of oval openings, the posterior nasal apertures or choanae. The parameters of the intranasal spaces depend on age and gender: growth is usually completed by the age of 16 (Samoliski et al 2007). Each half of the nasal cavity has a vestibule, roof, floor, medial (septal) and lateral walls. They include anomalous nasi, attached to the frontal process of the maxilla, procerus, transverse part of nasalis and the upper lateral cartilage. It is limited above and behind by a curved ridge, the limen nasi, raised where the greater ala of the lateral cartilaginous crus overlaps the lower edge of the lateral nasal cartilage on each side. On the septal side of the nasal cavity, the superior edge of the medial crus of the major alar cartilage (the medial intumescence) marks the boundary between the nasal vestibule and the nasal cavity. The medial wall of the vestibule is formed by a mobile septum consisting of the columella (which does not contain cartilage) and the underlying medial crura of the alar cartilages. The alae and lower part of the nasal septum are supplied by lateral nasal and septal branches of the facial artery, and the lateral aspects and dorsum of the nose are supplied by the dorsal nasal branch of the ophthalmic artery and the infraorbital branch of the maxillary artery. The venous networks draining the external nose do not run parallel to the arteries but correspond to arteriovenous territories of the face. The frontomedian region of the face, including the nose, drains to the facial vein, and the orbitopalpebral area of the face, including the root of the nose, drains to the ophthalmic veins. Lymph drainage is primarily to the submandibular group of nodes, although lymph draining from the root of the nose drains to superficial parotid nodes. The anterior slope is formed by the nasal spine of the frontal bones and by the nasal bones. The central region is formed by the cribriform plate of the ethmoid bone, which separates the nasal cavity from the floor of the anterior cranial fossa. It contains numerous small perforations that transmit the olfactory nerves and their ensheathing meningeal layers, and a separate anterior foramen that transmits the anterior ethmoidal nerve and vessels. The medial slip blends into the perichondrium of the lateral crus of the major alar cartilage of the nose and the skin over it. The lateral slip is prolonged into the lateral part of the upper lip, where it blends with levator labii superioris and orbicularis oris. Superficial fibres of the lateral slip curve laterally across the front of levator labii superioris and attach along the floor of the dermis at the upper part of the nasolabial furrow and ridge. Thus, the superficial muscular aponeurotic system is continuous from the nasofrontal process to the nasal tip, splitting at the caudal end of the lateral cartilage into superficial and deep layers, each with medial and lateral components (Oneal et al 1999). Dissection in rhinoplasty is usually performed in a sub-superficial muscular aponeurotic system plane. Posteriorly, the roof of the nasal cavity is formed by the anterior aspect of the body of the sphenoid, interrupted on each side by an opening of a sphenoidal sinus, and the sphenoidal conchae or superior conchae. Anteriorly, near the septum, a small infundibular opening in the bone of the nasal floor leads into the incisive canals that descend to the incisive fossa; this opening is marked by a slight depression in the overlying mucosa. The floor of the nose may be deficient as a result of congenital clefting of the hard and/or soft palate. Other bones that make minor contributions to the septum at the upper and lower limits of the medial wall are the nasal bones and the nasal spine of the frontal bones (anterosuperior), the rostrum and crest of the sphenoid (posterosuperior), and the nasal crests of the maxilla and palatine bones (inferior). The conchae have been removed to show the positions of the ostia of the paranasal sinuses and the nasolacrimal duct. Its anterosuperior margin is connected above to the posterior border of the internasal suture, and the distal end of its superior portion is continuous with the upper lateral cartilages. The anteroinferior border is connected by fibrous tissue on each side to the medial crurae of the major alar cartilage. Anteroinferiorly, the cartilaginous septum is attached to the anterior nasal spine, which is formed by anterior projections of each maxillary crest, and it has a strong, tongue-in-groove attachment with the premaxilla and vomer. The cartilaginous septum anterior to the spine is essential in tip support and should not be excised during septal surgery in order to prevent columellar retraction or loss of tip support. The posterosuperior border joins the perpendicular plate of the ethmoid, while the posteroinferior border is attached to the vomer and, anterior to that, to the nasal crest and anterior nasal spine of the maxilla. The anteroinferior part of the nasal septum between the nares is devoid of cartilage and is therefore called the membranous septum; it is continuous with the columella anteriorly. Above the incisive canals, at the lower edge of the septal cartilage, a depression pointing downwards and forwards is all that remains of the nasopalatine canal, which connected the nasal and buccal cavities in early fetal life. Near this recess, a minute orifice leads back into a blind tubule, 26 mm long, which lies on each side of the septum and houses remnants of the vomeronasal organ (see below). It contains three projections of variable size: the inferior, middle and superior nasal conchae or turbinates. The conchae curve inferomedially in general, each roofing a groove, or meatus, which is open to the nasal cavity.
© 2025 Adrive Pharma, All Rights Reserved..