General Information about Fertomid
Fertility has all the time been a subject of great significance and curiosity, especially for couples who're attempting to start a family. For some, fertility could come naturally, however for others, it might require a little additional assist. This is the place medications like Fertomid come into play. Fertomid is a fertility agent that is used to stimulate ovulation in women who are having problem getting pregnant.
Fertomid, also referred to as clomiphene citrate, is a nonsteroidal fertility medicine that belongs to a category of medicine called selective estrogen receptor modulators (SERMs). It works by blocking estrogen receptors in the mind, which then signals the body to provide extra follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones are essential in the strategy of ovulation, the place the ovaries launch an egg every month.
Fertomid is usually prescribed to ladies who are experiencing ovulation issues, which is amongst the most common causes of infertility. This could probably be because of situations like polycystic ovary syndrome (PCOS) or premature ovarian failure. Fertomid can additionally be used for girls who've irregular menstrual cycles or those who are undergoing fertility remedies like in vitro fertilization (IVF).
One of the significant benefits of Fertomid is that it's comparatively affordable in comparability with different fertility remedies. It additionally has a high success price, with studies exhibiting that about 70% of girls who take Fertomid will ovulate, and around 35% will turn into pregnant inside six cycles of use. However, it's essential to note that the success of fertility remedies varies from individual to individual and is decided by many factors, together with age, total health, and underlying causes of infertility.
In some instances, Fertomid is probably not the most effective option for treating infertility. If a lady has blocked fallopian tubes or if her male associate has fertility issues, other remedies like IVF may be beneficial as an alternative. It is at all times important to consult with a fertility specialist to discover out one of the best plan of action for every particular person's distinctive scenario.
In conclusion, Fertomid is a well-liked fertility agent that has helped many women efficiently conceive and begin a household. It is a relatively secure and reasonably priced remedy that stimulates ovulation in ladies with ovulation problems. However, it is important to understand the potential dangers and considerations related to Fertomid and to seek the assistance of with a healthcare skilled for an individualized remedy plan. With the proper steering and support, fertility treatments like Fertomid can convey a glimmer of hope for couples who dream of changing into parents.
The dosage of Fertomid varies relying on the person's condition, but it is sometimes taken orally for 5 days of the menstrual cycle. It is important to follow the prescribed dosage and instructions to ensure most effectiveness and avoid any potential unwanted side effects. Some widespread side effects of Fertomid embrace hot flashes, mood swings, complications, and breast tenderness. These side effects are normally delicate and go away on their very own.
Like any medication, Fertomid does include some potential risks and concerns. Women with a historical past of liver disease, ovarian cysts, or uterine fibroids ought to inform their physician before beginning Fertomid. Additionally, Fertomid might increase the danger of a quantity of pregnancies (twins/triplets), which might lead to potential issues throughout pregnancy and delivery.
Antibodies produced by the adaptive immune system are designed to react with and eliminate a particular antigen womens health kate beckinsale effective 50 mg fertomid. Different types of infectious agents stimulate distinct patterns of immune response that typically are host protective and result in adaptive and specific immunity to the infectious agent. The principal protective immune response against extracellular bacteria (those invading extracellular spaces) and bacteria in the circulation is specific antibody that opsonizes bacteria for phagocytosis by macrophages and polymorphonuclear leukocytes. During the process of opsonization, a pathogen is marked by complement proteins for phagocytic ingestion and destruction. Defend against intracellular pathogens and cancer by binding to and lysing infected cells or cancer cells. Complement comprises over 20 different serum proteins, some of which can bind to antibodies or to membrane components of cells. Intracellular bacteria survive and replicate within host cells, including phagocytes, because these microorganisms have developed mechanisms for resisting intracellular degradation. Immunity against these bacteria is principally cell-mediated and consists of T-helper lymphocytes that activate macrophages by the production of cytokines. Adaptive immunity against viruses consists of specific cytotoxic T lymphocytes that lyse virally infected cells and may contribute to tissue injury even when the infectious virus is not cytopathic by itself. Adaptive immunity against viruses also consists of specific antibodies and T-helper lymphocytes that provide cytokines for the growth and differentiation of effector T and B lymphocytes. Describe the difference between the innate immune system and the adaptive immune system. Cells such as macrophages are resident in almost all tissues and are found in particularly large numbers at mucosal sites, which are in contact with the external environment. Polymorphonuclear leukocytes are present in the blood in very large numbers, and they can be rapidly recruited to any site where complement has been activated. During the early phase of adaptive host defense, antigen-presenting cells called dendritic cells66 engulf or phagocytose microbial antigen, such as viral antigen, and degrade the antigen into small peptides. The antigen (peptide) activation of T lymphocytes leads to the clonal proliferation of these antigen-specific lymphocytes, resulting in the production of effector T lymphocytes, such as T-helper lymphocytes that produce cytokines that drive the proliferation and differentiation of cytotoxic T lymphocytes. The presence of IgM (characteristic of the primary response) begins to be detectable in the circulation 34 days after antigen entry and peaks between 2 and 3 weeks. The IgG response (characteristic of the secondary response) is delayed 57 days and persists much longer. Adaptive immune response to antigen is characterized during the primary response by a long lag period before the appearance of antibody in the circulation as well as a predominant IgM response. The secondary response to the same antigen is characterized by a shorter lag period before appearance of antibody in the circulation and by a predominant IgG response that is of a much greater magnitude than that during the primary immune response. Subsequent encounters with the same infectious agent will also be vigorously mounted. This secondary or adaptive immune response, which is mediated by longlived memory T lymphocytes and memory B lymphocytes, is the basis for subsequent protective immunity, which is the basis of vaccination. The protective components of the host response to bacteria are summarized in Table 13. In addition, for diseases caused by exotoxigenic organisms (microorganisms that secrete toxins, such as C. This neutralization occurs as the result of specific antibody blocking the interaction of the toxin with its mammalian cell surface target. In the case of tetanus toxin, the antibody blocks the toxin from binding to neurons. Other protective mechanisms that are employed in the host defense against viruses are listed in Table 13. Fungi Phagocytic cells primarily handle these microorganisms, particularly cytokine-activated phagocytes. An excellent example of a fungus that is handled by the immune system in this way is C. Parasites Large, multicellular parasites present a special problem to the immune system and indeed are rather poorly eliminated. The mechanisms that are deployed include antibody-directed complement-mediated destruction and antibody-dependent cellular cytotoxicity (antibodies specific for the parasite are bound to receptors on the effector cells) mediated by eosinophils derived from the peripheral blood. The parasites employ many evasion strategies, including complement inhibitors, release of large quantities of soluble antigen, and acquisition of host proteins. Different arms of the immune system are needed for protection from these differing microorganisms. In addition, many pathogenic microorganisms have evolved specific countermeasures, which limit or inhibit the effectiveness of the immune response. The general types of microbial pathogens are classified as either extracellular or intracellular microorganisms. Resistance to Intracellular Microorganisms Bacteria and Protozoa Many microorganisms have evolved resistance to the constitutive killing mechanisms used by phagocytes. These pathogens actively replicate inside mammalian cells, either in the phagosome or in the cytoplasm. T-cell activation is required, and a T-helper lymphocyte response, which results in the production of cytokines that activate phagocytes (in this case, alveolar macrophages), is necessary for clearance of the microorganism. What is effective is the development of a delayed type hypersensitivity reaction to proteins derived from mycobacteria. This reaction demonstrates the importance of cytokine producing T-helper lymphocytes that are responsive to the mycobacteria, and such a reaction correlates with exposure to the antigen and probable protective immunity.
Examples Epilepsy Parkinson disease Stroke Plantar fasciitis Tension headache Myofascial Neuropathic Carpal tunnel syndrome Diabetic neuropathy Postherpetic neuralgia Trigeminal neuralgia Phantom limb pain women's health clinic st louis buy 50 mg fertomid fast delivery. Stress-induced headache Facial or lower back pain following an emotional situation. Cervical radicular pain Lumbar radiculopathy Burns Arthritis Fracture Chest pain as with angina pectoris or myocardial infarction Lower extremity pain associated with peripheral artery disease Migraine headache Appendicitis Gallbladder disease Kidney stones Phantom Pain associated with a missing body part or a surgically removed limb. Believed to result from damaged or dysfunctional nerve pathways at the site of injury. Physical pain with psychologic causes such as stress or anxiety Pain caused by inflammation or compression of a spinal nerve root. Some C fibers are heat and chemical sensitive only but can develop mechanical sensitivity in the presence of tissue injury. C fibers are responsible for conducting the "second" or "slow" pain, a throbbing, burning, aching sensation that is poorly localized and not specifically related to a stimulus. Nociceptors show no adaptation and depolarize in proportion to the intensity and frequency of the stimulus; the greater the stimulus, the greater is the transduction of the stimulus into a nerve impulse. Activation of voltagegated sodium and potassium channels on the Ad and C fibers is necessary for the generation and conduction of the action potential. Responsible for the transmission of touch and pressure from the periphery of the body or internal viscera to the dorsal horn of the spinal cord. Responsible for transmission of "first" or "fast" pain to the dorsal horn of the spinal cord Responsible for transmission of parasympathetic and sympathetic impulses from the brain and spinal cord to the postganglionic fibers. Responsible for sympathetic stimulation of the heart blood vessel, smooth muscle, viscera, and glands. A-beta (Ab) 512 Myelinated 3070 A-delta (Ad) B 25 63 Myelinated Lightly myelinated 1530 315 C Sympathetic 0. Peripheral sensitization can result from inflammation- or trauma-triggered changes in the chemical environment of the free endings of the nociceptor. The resulting "inflammatory soup" increases the excitability and sensitivity of the nociceptors. Damage to peripheral nociceptors can result in spontaneous depolarization or altered conduction. Unlike other neurons that have an axonal branch and a dendritic branch, Ad and C afferents have both a peripheral branch and a central axonal branch that innervate their peripheral target and the spinal cord, respectively. The dorsal horn of the spinal cord is the relay center for nociceptive and sensory input. Activation of the dorsal horn depends on the intensity of the noxious stimulus, the release of excitatory or inhibitory neurotransmitters, and activation of descending and segmental inhibitory neurons. In response to tissue injury, endogenous inflammatory chemical mediators are released from mast cells, macrophages, platelets, neutrophils, endothelial cells, and fibroblasts. The predominant excitatory neurotransmitter is glutamate, which initially binds to the a@amino@3 @hydroxy@5 @methyl@4 @isoxazolepropionic acid receptor, which mediates fast synaptic transmission between first-order and second-order neurons. Third-order neurons transmit noxious impulses from the thalamus to the primary somatosensory areas for perception of pain. The third-order neurons project from the thalamus and midbrain to the somatosensory cortex for perception and localization of the pain; they also project to the limbic system, which is associated with the behavior, emotion, and memory of pain. On the way, they synapse in the periaqueductal gray matter, nucleus raphe magna, and medullary reticular formation. The primary neurotransmitters of the descending tracts are norepinephrine and serotonin. The descending tracts also stimulate the release of supraspinal and spinal endogenous opioids (endorphins, dynorphins, and enkephalins). In the periphery, injured tissues release substance P and glutamate, which directly activates nociceptors. Potassium, hydrogen ions, lactic acid, acetylcholine, serotonin, bradykinin, histamine, prostaglandins released from injured cells, local mast cells, plasma, and platelets sensitize and excite nociceptors and mediate inflammation. This peripheral sensitization results in primary hyperalgesia, in which a reduced stimulus intensity can activate nociceptors. Primary hyperalgesia decreases as healing reduces the amount of the sensitizing substances. When a peripheral nerve is injured, glial cells accumulate in the dorsal horn in the terminal lamina of the injured nerve. They release proinflammatory cytokines (tumor necrosis factor, interleukin 1, and interleukin 6), glutamate, and nitric oxide, which directly activate first-order and secondorder neurons in the dorsal horn and favor the development of persistent central pain (regional pain that is caused by a primary lesion or dysfunction of the central nervous system and persists after resolution of the initial inflammation or trauma). Peripheral nerve injury also activates glial cells in the brainstem that decrease the effectiveness of the inhibitory function of the descending tracts. Central sensitization is a result of increased excitability of the dorsal horn that results in an amplification of the noxious stimulus. Excessive or continued activation of the dorsal horn results in an abnormal response to sensory input and secondary hyperalgesia, an increased peripheral sensitivity beyond the site of the injury. The perception of pain is influenced by emotional or psychologic stress, cultural and religious beliefs, and prior experience with pain. While the intensity of the stimulus is an external event, the threshold is the perception of the patient. Sensitization, an increased excitability of neurons, occurs when the pain threshold is lowered and there is increased responsiveness of the neuron. Peripheral sensitization is a result of a decreased threshold and increased responsiveness of the peripheral nociceptors. Central sensitization is usually triggered by increased activity of peripheral nociceptors in response to trauma or inflammation that alters the synaptic connections between the first- and second-order neurons in the dorsal horn. With sensitization, low-threshold sensory fibers responsive to light touch can activate neurons in the dorsal horn that normally respond only to noxious stimuli.
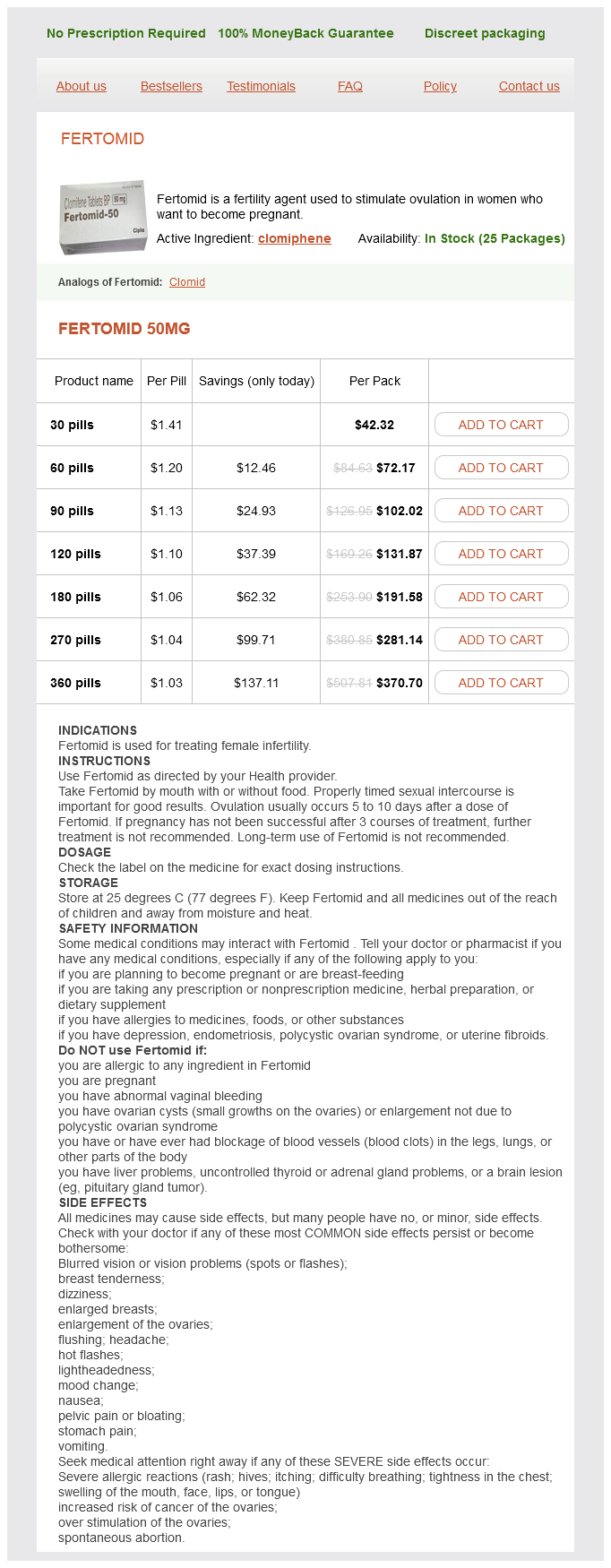
Fertomid Dosage and Price
Fertomid 50mg
- 30 pills - $42.32
- 60 pills - $72.17
- 90 pills - $102.02
- 120 pills - $131.87
- 180 pills - $191.58
- 270 pills - $281.14
- 360 pills - $370.70
Frozen shoulder has also been seen in individuals who have experienced an acute shoulder injury or who are recovering from surgical repair of another shoulder problem womens health nurse practitioner buy 50 mg fertomid. Because movement exacerbates the pain, the person begins to limit arm and shoulder movements. This self-imposed immobility of the shoulder leads to stiffness, more pain, and continued loss of motion. Eventually, the patient is unable to move the arm above the head or behind the back. Linking Pathophysiology to Diagnosis and Treatment the diagnosis of impingement syndrome is made when pain is immediately relieved after an anesthetic is injected into the space below the acromion. Additional diagnostic testing may include x-rays to assess for arthritis, bone spurs, or a rotator cuff tear. Then progressive exercising is used to strengthen the muscles and maintain joint flexibility. Shoulder pain that continues after conservative treatment may be treated with arthroscopic surgery to widen the subacromial space. Postoperative care after surgery includes pain management and progressive physical therapy to ensure shoulder muscle strength and joint mobility. If left untreated, frozen shoulder can resolve within 2 years with minimal loss of shoulder function. At times, arthroscopic surgery may be performed to cut the ligament in an attempt to get shoulder joint function to return. Even with surgery and physical therapy, a patient may continue to experience shoulder pain and stiffness. This section focuses on osteomyelitis (bone infection), osteonecrosis, and bone tumors. Bone tumors can be benign or malignant or can develop as a result of metastatic bone disease. These infections are also seen after joint replacement and internal fixation surgeries. Although osteomyelitis can occur at any age, it is seen most frequently in people over the age of 50. Osteonecrosis When the blood supply to the bone is altered, the area is prone to developing necrosis. Other names for osteonecrosis are avascular necrosis, aseptic necrosis, or ischemic necrosis. It most often affects the bones of the lower extremities but can also occur in the shoulders. Etiology and Pathogenesis In osteomyelitis, an offending microorganism, such as bacteria, fungi, parasites, or viruses, lodge and multiply in the bone. The microorganism causes inflammation and an immune response with the formation of pus, edema, and vascular congestion. Canals within the bone permit the infection to move to other bone areas, which could potentially disrupt blood supply to the bone tissue. Osteomyelitis can also occur if an infection from another body area is carried to a bone through the blood supply. This is often seen in older patients, patients with sickle cell disease, and patients who engage in intravenous substance abuse. Individuals with a chronic health problems such as diabetes are prone to developing osteomyelitis from an infected foot wound. A postoperative joint replacement that becomes infected can also cause osteomyelitis and is considered the most common cause of the bone infection in adults. But if blood flow to a joint is reduced, bone breakdown occurs faster than replacement bone is made. Over time, the bone in the joints breaks down, leading to pain and alterations in joint mobility. Although this health problem can occur in anyone at any age, it is most commonly seen in people between the ages of 30 and 50 years. Risk factors for the development of osteonecrosis include long-term use of steroids, heavy alcohol intake, and direct injury to the bone or joint. The people who are most prone to developing this health problem are those who are undergoing chemotherapy or radiation or who have had an organ transplantation. However, some individuals with no known health problem or risk factor can develop the disorder. In time the patient may begin to experience pain when pressure or weight is applied to the affected joint. The onset of the disease process to complete loss of limb function may take months to over a year. Local indications of a bone infection include bone pain, drainage and ulceration at the site, swelling, redness, warmth, and localized tenderness. Lymph node swelling, fever with chills, general malaise, tachycardia, nausea, vomiting, and anorexia are manifestations of a systemic bone infection. Linking Pathophysiology to Diagnosis and Treatment the diagnosis of osteonecrosis will be made after a physical examination and diagnostic tests confirm necrosis of a joint. Treatment of osteonecrosis is focused on interventions to prevent joint breakdown.
© 2025 Adrive Pharma, All Rights Reserved..