General Information about Fenofibrate
High cholesterol and triglyceride ranges are main threat factors for creating coronary heart disease, stroke, and other cardiovascular conditions. They are additionally related to quite lots of lifestyle components similar to unhealthy diets, lack of physical exercise, weight problems, and smoking. In most circumstances, life-style modifications such as adopting a nutritious diet, common exercise, and smoking cessation are beneficial as first-line treatments for top ldl cholesterol and triglyceride levels. However, in some circumstances, medicine may also be prescribed to effectively lower these ranges and reduce the danger of cardiovascular disease.
Like most drugs, Tricor may trigger some side effects, although not everyone experiences them. Some of the widespread unwanted effects associated with Fenofibrate use embody abdomen upset, gas, diarrhea, and headache. In uncommon cases, it could additionally cause extra extreme unwanted effects similar to liver issues and muscle ache. It is essential to inform your healthcare supplier immediately when you expertise any uncommon signs whereas taking this medicine.
Clinical trials have proven that Fenofibrate, when used as prescribed, can considerably cut back the degrees of triglycerides within the blood by up to 50% and enhance HDL levels of cholesterol by up to 15%. This discount in lipid ranges can lead to a 30% lower in the risk of developing cardiovascular issues. Additionally, Fenofibrate has also been discovered to have further advantages similar to lowering irritation and improving blood vessel perform.
Fenofibrate, generally known as Tricor, is a drugs used to deal with sufferers with high ldl cholesterol and really high levels of triglycerides in the blood. It belongs to the class of medications known as fibric acid derivatives and is often prescribed alongside a nutritious diet and exercise to successfully handle lipid levels in the body.
In conclusion, Fenofibrate, or Tricor, is a drugs that has been proven to be effective in managing high ldl cholesterol and very excessive ranges of triglycerides in the blood. It works by lowering triglyceride ranges, growing HDL ldl cholesterol, and offering additional advantages corresponding to lowering inflammation and improving blood vessel perform. When used as prescribed, it may possibly significantly cut back the danger of creating cardiovascular disease. As with any medication, it is important to observe your doctor’s directions and make lifestyle modifications to take care of general well being and wellbeing.
In addition to medicine, it is important to make lifestyle modifications that may help handle excessive ldl cholesterol and triglyceride ranges. This contains maintaining a healthy weight, following a balanced diet, regular train, limiting alcohol consumption, and quitting smoking. Fenofibrate works best when utilized in mixture with these way of life changes and can result in important improvements in general health and wellbeing.
Fenofibrate has been permitted by the FDA and has been used for over 20 years to treat sufferers with high ldl cholesterol and triglyceride ranges. However, as with all treatment, you will want to observe your doctor’s directions and use it as prescribed. Tricor may work together with other medicines, such as blood thinners and cholesterol-lowering medication, so it is very important inform your doctor of all of the medications you take earlier than beginning remedy.
Tricor works by reducing the production of triglycerides in the liver and growing the breakdown of fats in the blood. It also has the power to extend the levels of fine ldl cholesterol, also referred to as HDL, within the blood. Tricor is available in various types corresponding to tablets, capsules, and extended-release tablets, and is typically taken a couple of times a day, depending on the severity of the condition.
Keratosis follicularis spinulosa decalvans is probably the least common keratosis pilaris variant cholesterol values normal cheap fenofibrate american express. It is manifested by areas of skin thickening and follicular plugging Ulerythema ophryogenes showing loss of the lateral eyebrows Keratosis pilaris of upper thighs. Small 1- to 2-mm hyperkeratotic red papules Keratosis Pilaris Variants Keratosis pilaris rubra Ulerythema ophryogenes (keratosis pilaris atrophicans faciei) Atrophoderma vermiculata (folliculitis ulerythematosa reticulata) Erythromelanosis follicularis faciei et colli Keratosis follicularis spinulosa decalvans Keratosis pilaris atrophicans faciei. It is believed to be caused by an abnormality in follicular keratinization of the infundibulum. The plug is typically 1 to 2 mm in diameter and may lie on top of a meager lymphocytic infiltrate. After discontinuation, however, the rash of keratosis pilaris returns over a period of a few weeks to months. The cream is applied daily and has been successful in removing the redness and hyperkeratosis. Historically, the disease was categorized based on the grouping of symptoms and organs affected, with names such as Letterer-Siwe disease and HandSchüller-Christian disease. These histiocytoses are a heterogeneous group of diseases that may affect both the skin and various internal organs. The main pathological finding is the accumulation of pathological Langerhans cells within the affected tissue. The diagnosis is made on clinical, histological, laboratory, and radiographic findings. Prognosis and therapy depend on the organ systems involved and the number of systems implicated. Usually, the condition is first noticed in childhood, but adult-onset disease does occur. In infants, the typical presenting skin findings are those of a persistent papulosquamous eruption on the scalp that resembles cradle cap. The other common presentation in children is that of persistent diaper dermatitis. The rash has a unique predisposition to affect the groin folds and can be quite inflammatory and resistant to typical therapy for irritant contact dermatitis or diaper rash. The groin rash appears as red to yellowish-orange papules that coalesce in to plaques. Other skin findings that can be observed by the astute clinician are adenopathy, ear inflammation and drainage from the external ear, and soft tissue swelling. The soft tissue swelling is seen only in those patients with underlying bony disorders. Infants may also have premature eruption of their teeth, which is most commonly noticed by the still breast-feeding mother. The diaper area is one of the more common areas of involvement with Langerhans cell histiocytosis. This disease should be in the differential diagnosis of diaper rash that does not respond to therapy for dermatitis, especially if petechiae are present. Sheets of Langerhans cell histiocytes with abundant pink cytoplasm and folded nuclei with prominent nuclear grooves Disseminated Langerhans cell histiocytosis lesions in axilla and on neck and trunk systemic complaints. Children present with a painless to slightly tender soft tissue swelling overlying the bony area of involvement, most commonly the calvarium. Palpation of the swelling reveals the fluctuant nature of the soft tissue distention, and in some cases the defect in the underlying bone can be felt. If one area of bony involvement is found, a skeletal survey should be performed to evaluate for other silent bony lesions, which can occur in up to 15% of cases. The involved bone has a radiolucent appearance that is sharply demarcated from the surrounding bone. The term "floating teeth" has been used to describe the finding of radiolucent aspects of the mandible that give the appearance that the teeth are floating without the support of the underlying bone. Biopsies of lymph nodes can show involvement with Langerhans cells or dermatopathic changes. Radiographs may be normal or may show cystic spaces or a nonspecific interstitial infiltrate. Pulmonary function testing may reveal a decrease in diffusion capacity and a decrease in forced expiratory volume. The lack of antidiuretic hormone causes the excretion of large amounts of dilute urine and increased thirst. Letterer-Siwe disease is the name given to the constellation of symptoms that include severe skin involvement, hepatosplenomegaly, anemia, and leukopenia. These patients have early onset of disease in infancy and have a poor prognosis because of the aggressiveness and extent of the disease load. Treatment likewise depends on these factors, and a multidisciplinary approach should be taken. Pathogenesis: the exact etiology is unknown, and there is considerable ongoing research to determine whether this is a clonal malignant process or a reactive process. The Langerhans cells that are present within the areas of involvement have a different morphology from their normal counterparts. The affected Langerhans cells are round, without dendritic processes, and have been found to express different cell surface markers. Histology: Histological findings from the skin and other involved tissues are only slightly different. The main pathology is found within the sheets of abnormalappearing Langerhans cells. On microscopic evaluation, the cells have kidney beanshaped nucleus and show varying amounts of epidermotropism. On electron microscopy, the characteristic tennis racketshaped Birbeck granules are seen.
Less often cholesterol lowering foods list discount fenofibrate 160 mg with mastercard, duplication may also occur in the lower gastrointestinal tract or spine. It is possible that complete duplication of the bladder and adjacent organ systems reflects partial twinning of the embryonic tail early in gestation. In contrast, isolated defects of the bladder may reflect abnormalities during cloacal septation (see Plate 2-4). The left half does not communicate with the urethra and is thus obstructed, with associated renal abnormalities. The right-sided ureter exhibits vesicoureteral reflux, with associated hydroureteronephrosis. Partial septation of bladder the timing of diagnosis depends on the nature and extent of the malformation. If there is external evidence of duplication-such as in the genitals or spine-the patient is likely to undergo comprehensive evaluation early in life, during which the bladder abnormality will be discovered. Once the diagnosis has been established, further evaluation should include a renal scan to assess kidney function, as well as video-urodynamic studies to examine voiding from each bladder compartment and to determine if vesicoureteral reflux is present. If an obstruction is present, it should be excised as soon as possible so as to reduce the risk of further infection and preserve renal function. If incontinence, vesicoureteral reflux, external duplication, and/or other anomalies are present, a more complex intervention will be required, the specifics of which must be tailored to each individual patient. The urogenital sinus, which gives rise to the bladder, is initially continuous with the allantois, a tube that extends in to the connecting stalk (see Plate 2-4 for an illustration). As the bladder matures and descends in to the pelvis, however, the allantois narrows to form a thick, epithelial-lined tube known as the urachus. Normally the urachus regresses in to a fibrous cord, known as the median umbilical ligament. For uncertain reasons, however, this normal regression process sometimes fails, resulting in a persistent urachus that is either partially or completely patent. Because many urachal anomalies are undiagnosed, their overall incidence is unknown. It typically presents during the neonatal period as dribbling of fluid from the umbilicus. The fluid leakage may increase in response to bladder contraction during either purposeful voiding or other increases in intraabdominal pressure, such as during crying or straining. A patent area at the distal end of the urachus, which communicates with the umbilicus, is known as a superior urachal sinus (or umbilical-urachal sinus) and accounts for 15% of urachal anomalies. Like a patent urachus, a superior sinus causes umbilical discharge during the neonatal period, although the fluid is not as copious. A patent area in the middle of the urachus, which communicates with neither the umbilicus nor bladder, is known as a urachal cyst and accounts for about 30% of urachal anomalies. It may be noted as an incidental finding during laparotomy; as a palpable midline mass; or as a site of infection, usually with Staphylococcus aureus, with associated pain and erythema. Finally, a patency in the proximal end of the urachus, which communicates with the apex of the bladder, is known as an inferior sinus (or vesicourachal diverticulum) and accounts for 5% of urachal anomalies. It usually does not cause symptoms because it is has a large opening in to the bladder lumen and does not communicate with other structures. In rare instances, Inferior urachal sinus (vesicourachal diverticulum) Urachal cyst Urachal adenocarcinoma: computed tomography (contrast enhanced) Rectus abdominis muscles Urachal adenocarcinoma Bladder however, it may act as a site of calculus formation or lower urinary tract infection. It is essential to remove all abnormal urachal tissue because there is a small risk of later malignant transformation. Thus, in addition to the urachus, a cuff of surrounding bladder tissue should be removed as well. An asymptomatic urachal cyst or inferior sinus can be managed with careful observation since spontaneous resolution is possible. If resolution does not occur, however, or if symptoms emerge, all urachal tissue should be carefully excised. They are the most common cause of congenital urinary tract obstruction, occurring in 1 in 8000 to 1 in 25,000 live births, and are seen only in males. The traditional classification system describes two major types of valves, which vary both in morphology and relative frequency. Type I valves, said to account for more than 95% of cases, begin as a mucosal ridge from the seminal colliculus, which extends distally and divides in to two flaps that fuse with the walls of the membranous urethra. There is typically incomplete fusion of the flaps with the anterior wall of the urethra, and there is a small opening in the membrane near the posterior wall of the urethra, adjacent to the seminal colliculus. The segments include the prostatic urethra, which extends from the bladder neck to the urogenital diaphragm; the membranous urethra, which traverses the diaphragm; the bulbous urethra, which extends from the urogenital diaphragm to the penoscrotal junction; and the spongy (penile) urethra, which continues through the penile shaft until the urethral meatus. Between the fourth and sixth weeks of fetal development, the cloaca is divided in to the primitive urogenital sinus and the rectum, and the cloacal membrane is likewise divided in to the urogenital membrane and rectal membrane. The primitive urogenital sinus has several distinct regions that give rise to the different segments of the lower urinary tract. The dilated cranial region becomes the urinary bladder; the neck just caudal to this region becomes the prostatic and membranous urethra; and the most caudal region, known as the definitive urogenital sinus, becomes the bulbous and spongy urethra. As the urinary tract develops, swellings known as the cloacal folds appear lateral to the cloacal membrane. After the urogenital membrane dissolves, the urethral folds fuse in the midline, encasing the future bulbous and penile urethra. The dilated prostatic urethra can be seen caudal to the dilated bladder, a phenomenon known as the "keyhole" sign.
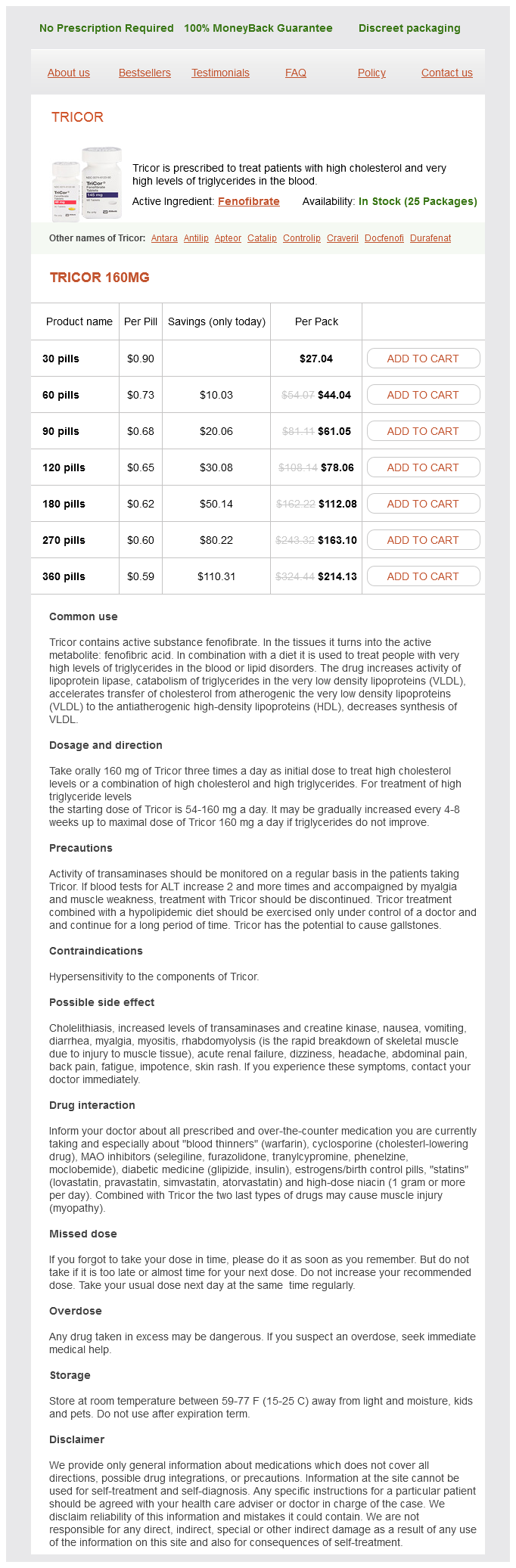
Fenofibrate Dosage and Price
Tricor 160mg
- 30 pills - $27.04
- 60 pills - $44.04
- 90 pills - $61.05
- 120 pills - $78.06
- 180 pills - $112.08
- 270 pills - $163.10
- 360 pills - $214.13
Systemic involvement is significant cholesterol lowering foods red wine buy generic fenofibrate online, with recurrent bouts of pancreatitis and hepatosplenomegaly. These patients have extremely elevated triglyceride and chylomicron levels but normal cholesterol levels. The blood vessels within the eye have a creamy white color because of the excess lipid in the bloodstream. The arteries and veins are equally affected, and the only way to differentiate the two is by comparing the caliber of the vessel. Lipoprotein lipase enzyme activity can be measured, and this test is used to help diagnosis type I hyperlipoproteinemia. This protein is particularly important in clearing chylomicrons and intermediatedensity lipoproteins. Multiple medications have been implicated in the production of hypertriglyceridemia. They include isotretinoin, glucocorticoids, olanzapine, protease inhibitors (especially ritonavir), and indomethacin. Patients presenting with eruptive xanthomas who are taking any of these medications should have the medication discontinued or another substituted and should be reevaluated after treatment. Diabetes is the most common cause of hypertriglyceridemia, and it probably is also the most common cause of eruptive xanthomas. Diabetic patients who are deficient in insulin have lower activity levels of lipoprotein lipase and increased levels of chylomicrons and triglycerides as a result. If a sample of blood is centrifuged for a few minutes, the white to creamycolored triglycerides will become evident and will take up a considerable amount of the specimen. On occasion, there are so many triglycerides present that the blood sample is a light creamy color even before centrifugation. Histology: the histological findings from biopsies of early lesions of eruptive xanthomas can mimic those of granuloma annulare. The neutrophilic infiltrate lessens and disappears once the lesion has had time to establish itself. It is recommended that the biopsy specimen be taken from an established lesion (one that has been present for a day or two) so that more characteristic findings will be seen. The number of foam cells is not as prominent as in tuberous or tendinous xanthomas. One unique finding is the presence of extracellular lipid, which is seen between bundles of collagen. The final common pathway in the pathogenesis of eruptive xanthomas is the presence of significantly elevated triglyceride levels. Treatment: the main goal of therapy is to return the triglyceride level back to a normal range. Underlying diabetes needs to be treated aggressively to get better control of glucose metabolism and insulin requirements. Those patients with familial causes need to institute dietary changes ( to avoid medium-chain triglycerides), increase their activity level, and take triglyceride-lowering medications. The medications most commonly used to lower triglyceride levels are fenofibrate and gemfibrozil. For unknown reasons, not all persons exposed to heat sources develop the rash of erythema ab igne. Reported causes have included hot water bottles, heating blankets, heaters, and computer laptops. Erythema ab igne has also been called the "roasted skin" or "toasted skin" syndrome. The exact temperature needed for the reaction to occur is unknown, and for some reason it does not occur from hot tub use, most likely because the causes of erythema ab igne are dry heat or temperatures higher than those of most hot tubs. Clinical Findings: this condition can be seen in individuals of any race and gender. Occasionally, no inflammatory phase is noticed, only a reticulated hyperpigmentation of the skin. Some patients do not realize that the rash is located on skin in direct approximation to a heat source. The lower back is a commonly affected area, secondary to the use of heating blankets or bottles to help treat chronic lower back pain. There have been many reports of erythema ab igne from exposures to all sorts of heat sources. Laptop computers can release a large amount of energy as infrared radiation; if someone is chronically using a laptop computer in direct approximation to their skin. The diagnosis is typically made by clinical examination and historical information. Patients often need to be asked whether they have been using a heating device or consistently using a laptop computer, because the correlation is not evident to them. The development of actinic keratosis or squamous cell carcinoma within the areas of erythema ab igne has rarely been reported. Pathogenesis: Erythema ab igne is caused by the direct effects of heat on the skin. The temperature required has not been precisely defined, but the range of 43°C to 47°C seems to be most likely. In any case, there must be repeated exposure to subthermal burning Also known as "toasted skin syndrome," erythema ab igne is caused by excessive heat transfer to the underlying skin. Common Etiologies of Erythema Ab Igne Heating blanket/pad Hot water bottles Localized heaters/radiators Laptop computers temperatures. More frequent exposures and longer exposures seem to increase the risk of development of erythema ab igne.
© 2025 Adrive Pharma, All Rights Reserved..