General Information about Feldene
When taken orally, Feldene is normally prescribed at a low dose to be taken as soon as a day. It is recommended to be taken with meals to reduce gastrointestinal side effects, as this treatment could cause stomach upset. The dose could also be increased progressively if the initial dose just isn't efficient, however the maximum beneficial every day dose shouldn't exceed 20 mg. Doctors may also prescribe Feldene together with other medicines, corresponding to disease-modifying antirheumatic medicine (DMARDs), to realize better management of the disease.
However, like all medicines, Feldene also has unwanted side effects, the most typical being stomach upset similar to nausea, abdominal pain, and heartburn. In uncommon circumstances, it may additionally cause critical side effects, such as an increased risk of coronary heart attack, stroke, and abdomen bleeding. Therefore, it's important to take Feldene as prescribed by the doctor and not to exceed the really helpful dose.
One of some great benefits of Feldene over other NSAIDs is its lengthy half-life. This implies that the drug stays within the body for a extra prolonged period, allowing sufferers to take it as quickly as a day instead of multiple occasions a day. This can improve patient compliance and decrease the chance of adverse side effects.
In conclusion, Feldene is a broadly used and effective drug for the treatment of persistent inflammatory conditions like rheumatoid arthritis and osteoarthritis. Its anti-inflammatory and pain-relieving properties assist enhance the quality of life for patients, lowering their reliance on different pain drugs. However, like all treatment, it should be taken with caution and underneath the supervision of a healthcare professional to keep away from potential unwanted facet effects. With correct use and monitoring, Feldene can present much-needed aid for those living with these debilitating situations.
Feldene helps in the management of RA and OA by lowering the irritation and ache related to these circumstances. It is available in varied forms, including capsules, injection, and gel. The alternative of administration is determined by the severity of the situation and the patient’s response to therapy.
Feldene is also not suitable for everybody. Patients with a historical past of abdomen ulcers, asthma, heart or liver illness, or those that are pregnant or breastfeeding mustn't take this medication. It is all the time essential to debate with a doctor or pharmacist before beginning any new medication.
Feldene, additionally identified by its generic name piroxicam, is a non-steroidal anti-inflammatory drug (NSAID) used to deal with continual inflammatory circumstances corresponding to rheumatoid arthritis and osteoarthritis. It belongs to the category of medication referred to as oxicams and works by reducing the body’s manufacturing of prostaglandins, that are answerable for causing inflammation, pain, and fever in the body. Feldene can help relieve pain, stiffness, and swelling associated with these circumstances, permitting sufferers to have a better quality of life.
Rheumatoid arthritis (RA) is an autoimmune disorder that impacts the joints, causing ache, stiffness, and swelling. It is a continual condition that may find yourself in joint harm and disability if left untreated. Osteoarthritis (OA), then again, is a degenerative joint disease attributable to put on and tear of the joints over time. It principally affects older adults and may result in joint pain, stiffness, and decreased mobility. Both conditions can significantly influence a person’s daily activities and total well-being.
Sentinel node biopsy for nonpalpable breast tumors requires a preoperative diagnosis of invasive breast cancer arthritis neck surgery cost of feldene. Core biopsy diagnosis of ductal carcinoma in situ: an indication for sentinel lymph node biopsy. An update of sentinel lymph node mapping in patients with ductal carcinoma in situ. Role of axillary sentinel lymph node biopsy in patients with pure ductal carcinoma in situ of the breast. Is it possible to refine the indication for sentinel node biopsy in highrisk ductal carcinoma in situ What is the value of axillary dissection or sentinel node biopsy in patients with ductal carcinoma in situ Tumor size as predictor of microinvasion, invasion, and axillary metastasis in ductal carcinoma in situ. Combined radioguided nonpalpable lesion localization and sentinel lymph node biopsy for early breast carcinoma. Cost/accuracy ratio analysis in breast cancer patients undergoing ultrasound-guided fine-needle aspiration cytology, sentinel node biopsy, and frozen section of node. Outcomes for women with ductal carcinoma-in-situ and a positive sentinel node: a multi-institutional audit. Sentinel lymph node metastasis from mammary ductal carcinoma in situ with microinvasion. Sentinel node biopsy is not a standard procedure in ductal carcinoma in situ of the breast: the experience of the European institute of oncology on 854 patients in 10 years. Do sentinel node micrometastases predict recurrence risk in ductal carcinoma in situ and ductal carcinoma in situ with microinvasion Role of primary tumor characteristics in predicting positive sentinel lymph nodes in patients with ductal carcinoma in situ or microinvasive breast cancer. The sentinel lymph node procedure for patients with preoperative diagnosis of ductal carcinoma in situ: risk factors for unsuspected invasive disease and for metastatic sentinel lymph nodes. Microinvasive breast cancer and the role of sentinel node biopsy: an institutional experience and review of the literature. Importance of Sentinel Lymph Node Biopsy in Surgical Therapy of in situ Breast Cancer. The effect of prior breast biopsy method and concurrent definitive breast procedure on success and accuracy of sentinel lymph node biopsy. Biopsy method and excision volume do not affect success rate of subsequent sentinel lymph node dissection in breast cancer. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: a population-based study. Salvage treatment for local recurrence following breastconserving surgery and definitive irradiation for ductal carcinoma in situ (intraductal carcinoma) of the breast. Fifteen-year results of breast-conserving surgery and definitive breast irradiation for the treatment of ductal carcinoma in situ of the breast. Factors associated with local recurrence and cause-specific survival in patients with ductal carcinoma in situ of the breast treated with breast-conserving therapy or mastectomy. Treatment for ductal carcinoma in situ in an Asian population: outcome and prognostic factors. Clinical outcome after selective treatment of patients diagnosed with ductal carcinoma in situ of the breast. Boost radiotherapy in young women with ductal carcinoma in situ: a multicentre, retrospective study of the Rare Cancer Network. Ductal carcinoma in situ of the breast results of conservative and radical treatments in 716 patients. Value of the Van Nuys Prognostic Index in prediction of recurrence of ductal carcinoma in situ after breastconserving surgery. Relationship between excision volume, margin status, and tumor size with the development of local recurrence in patients with ductal carcinoma-in-situ treated with breast-conserving therapy. Significance of multifocality in ductal carcinoma in situ: outcomes of women treated with breast-conserving therapy. Prevention of invasive breast cancer in women with ductal carcinoma in situ: an update of the national surgical adjuvant breast and bowel project experience. Ductal carcinoma in situ (intraductal carcinoma) of the breast treated with breast-conserving surgery and definitive irradiation. Breastconserving therapy for ductal carcinoma in situ: a 20year experience with excision plus radiation therapy. The prognostic significance of multiple morphologic features and biologic markers in ductal carcinoma in situ of the breast: a study of a large cohort of patients treated with surgery alone. The value of the Van Nuys Prognostic Index in ductal carcinoma in situ of the breast: a retrospective analysis. The significance of the Van Nuys prognostic index in the management of ductal carcinoma in situ. Are cellular polarisation and mitotic frequency prognostic factors for local recurrence in patients with ductal carcinoma in situ of the breast The importance of complete excision in the prevention of local recurrence of ductal carcinoma in situ. Rationalization and regionalization of treatment for ductal carcinoma in situ of the breast. An attempt to independently verify the utility of the Van Nuys Prognostic Index for ductal carcinoma in situ. Quality aspects of the tissue microarray technique in a population-based cohort with ductal carcinoma in situ of the breast. Factors associated with local recurrence of mammographically detected ductal carcinoma in situ in patients given breast-conserving therapy. Concurrent lobular neoplasia increases the risk of ipsilateral breast cancer recurrence in patients with ductal carcinoma in situ treated with breast-conserving therapy. Ductal carcinoma in situ: trends in geographic, temporal, and demographic patterns of care and survival. Local recurrences after conservative treatment of ductal carcinoma-in-situ of the breast without radiotherapy: the effect of age.
Despite these limitations arthritis in fingers young discount feldene 20 mg with mastercard, fibrin sealants have been shown to effectively reduce bleeding from tissue surfaces and anastomoses [20], and these adhesives have been used safely during acute aortic dissection repairs [6,21]. Nakajima and colleagues [22] recently described a technique in which a sheet of knitted polyester fabric is soaked in the fibrinogen solution and inserted between the dissected layers of the aorta, the thrombin solution is added on each side, and the layers are compressed, effectively obliterating the false lumen. Balancing risks and benefits Although surgical adhesives offer the opportunity to improve patient outcomes, these agents can cause early and long-term complications; therefore, improving their safety by carefully defining and addressing potential problems is essential. The critical balance between maximizing benefit and minimizing risk should be evaluated for each individual patient. Many groups have reported subjective benefits of using adhesives to facilitate aortic repairs. Adhesives appear to improve hemostasis, strengthen weak tissues, provide anastomotic support, and enhance the durability of repair [23-25]; these benefits are especially pronounced in patients with marked tissue fragility, including those with acute dissection or connective tissue disorders. Additional purported early benefits of adhesive use include reduced bleeding, decreased transfusion requirements, shortened operative and circulatory arrest times, and shortened lengths of hospital stay [21,23,26]. Additionally, the reduction in intra-operative bleeding could, theoretically, minimize the risk of coagulopathy and the need for early reoperation [17]. Whether adhesives provide longterm benefits, such as a reduced incidence of false lumen patency and a decreased incidence of late reoperation, remains controversial [9,27-29]. Although surgical adhesives may offer benefits, they pose several potential risks that warrant attention. Allergic reactions and infectious disease transmission remain concerns when one is using products of bovine or human origin. Additionally, the aldehyde components of adhesives have been reported to be directly toxic to nerves [30-33]; thus, when using aldehyde-based adhesives during arch repair, surgeons should take extra care to avoid the nearby phrenic and recurrent laryngeal nerves. The concerns about tissue toxicity in nerves also apply to cardiac conduction tissue [32,34]. Fibrin sealants vary in their composition but generally include a fibrinogen solution (fibrinogen + fibrinolytic inhibitor) and a thrombin solution (thrombin + calcium chloride solution). When the two components are mixed at the site of use, the gel solidifies in a reaction mimicking the physiologic coagulation and tissue adhesion cascade. The biologic components can potentially transmit infectious diseases, although aggressive pathogen inactivation protocols are used to minimize this risk. Systems that prepare autologous fibrin sealant promise to improve biocompatibility and eliminate the risks of viral infection [18,19], but such systems are not widely used. Further, fibrin sealants do not bond as strongly as aldehyde-based adhesives and may be weakened through fibrinolysis. Reports after reoperations have described necrotic, fibrosed, and excessively thinned aortic tissue found at the site of adhesive application [27,35,37,39,41]. Because aldehydebased glues have been linked to the development of vascular strictures and impaired aortic growth, they are not recommended for use during cardiovascular reconstructions in pediatric patients [35,41]. Systemic embolization of adhesive fragments is another concern, especially given the proximity of the brachiocephalic vessels during aortic arch repair. Some authors have used adhesive in the brachiocephalic vessels when dissection is present [42]; this should be done with caution because of the potential for embolization. Several reports have raised concerns about adhesive leaking into the aortic lumen, resulting in valve dysfunction or embolization [43-47]. Cerebral and myocardial infarctions caused by polymerized glue emboli have been found on autopsy, and polymerized glue emboli have been extracted from patients with severe acute limb ischemia [45,47,49]. Carrell and associates [49] have suggested three mechanisms by which adhesives may cause embolization: direct spillage into the true lumen (despite precautions), escape through reentry sites into the true lumen, and leakage through suture-line needle holes. The first two mechanisms can result from technical error, so careful attention and proper training of the surgical team will minimize this risk. Fortunately, the number of reported cases involving adhesive embolization remains low; however, the incidence of adhesive embolization may be underestimated, because adhesive embolization is rarely suspected as a cause when ischemic complications arise and because post-mortem microscopy examinations are not routinely performed in patients that succumb to complications of cardiovascular repairs. Given the well-documented risks involved in using surgical adhesives during aortic repairs, we do not recommend doing this routinely; however, during certain complex operations - especially in cases of acute aortic dissection - the benefits of using these agents may truly outweigh the potential risks. Thus, the risk-benefit ratio for using glue should be carefully considered on a patientby-patient basis. Adhesives and sealants should be used only when medically necessary to secure hemostasis and reinforce weak tissues. When the use of surgical adhesive is warranted by the clinical situation, several technical considerations can be applied to make the use of these products as safe as possible. Technical aspects of using glue during aortic arch repair We primarily use BioGlue in patients with acute aortic dissection; we perform these procedures using profound hypothermic circulatory arrest and an open distal anastomosis [51]. BioGlue is used to obliterate the false lumen and reinforce the fragile suture lines. Because blood interferes with tissue bonding, all clotted and fresh blood is removed from the false lumen to create a dry field. It is also sometimes necessary to stop antegrade or retrograde cerebral perfusion briefly before glue is applied. The dissecting membrane is carefully tacked to the outer wall with a few interrupted 6-0 sutures to keep the walls aligned during glue application. To protect surrounding structures from the tissue and nerve damage that contact with the glue can cause, gauze sponges dampened with saline can be used to shield these tissues from unintentional adhesive run-off during glue application. A Foley catheter with a 30-cc balloon is inserted via the true lumen into the proximal descending thoracic aorta, immediately distal to the left subclavian artery, and inflated to prevent the adhesive from running down the false lumen into the descending thoracic and abdominal aorta.
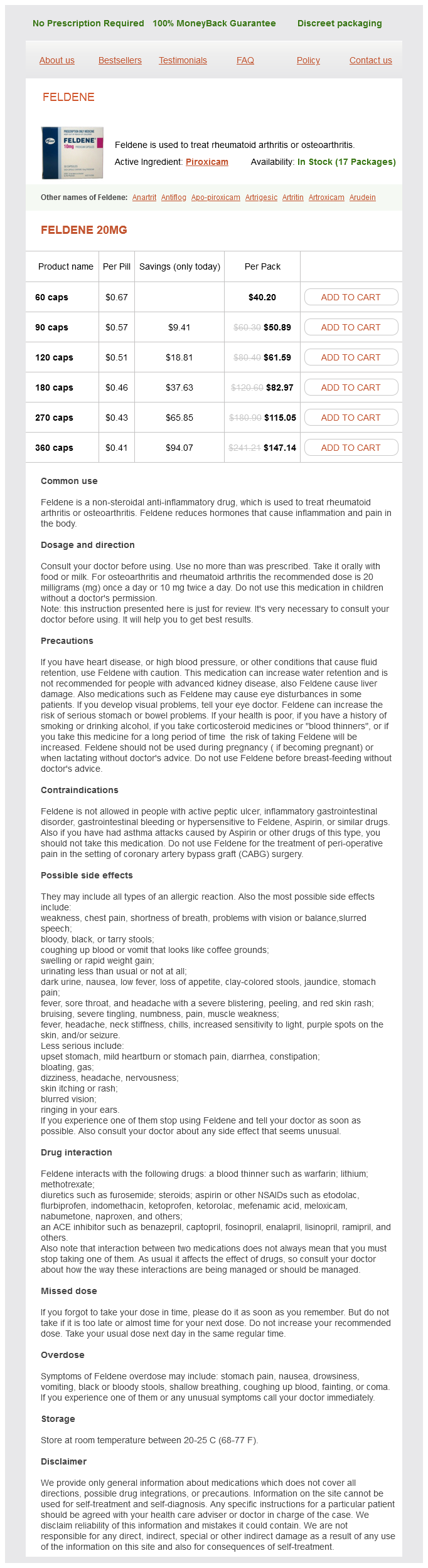
Feldene Dosage and Price
Feldene 20mg
- 60 caps - $40.20
- 90 caps - $50.89
- 120 caps - $61.59
- 180 caps - $82.97
- 270 caps - $115.05
- 360 caps - $147.14
If a bypass is performed arthritis laser treatments purchase feldene amex, a shunt can be inserted through the graft once the proximal anastomosis is done. In selected cases with focal distal disease, innominate reconstruction can also be performed through a cervical approach. In most patients, a vascular clamp can be safely placed on the distal innominate artery from a supraclavicular approach when the neck is extended. However, the cervical approach for innominate lesions is usually recommended for highrisk patients and for those who have had a previous sternotomy for coronary artery bypass grafting. Partial sternotomy is an excellent approach for patients who need distal innominate reconstruction [38]. A transverse 45 cm long supraclavicular incision is made one finger-breadth (2 cm) above the clavicle, starting over the medial head of the sternocleidomastoid muscle. The platysma and the lateral head of the sternocleidomastoid muscle are transected and the scalene fat pad is mobilized carefully, ligating all major lymphatic vessels before division to avoid lymph leak. The phrenic nerve is identified and carefully preserved as it courses from lateral to medial along the anterior surface of the anterior scalene muscle. The nerve is retracted and the anterior scalene is transected with electrocautery. The subclavian artery with its branches, including the thyrocervical trunk, the internal thoracic artery and the vertebral artery, is dissected and encircled with vessel loops. The third portion of the subclavian artery, lateral to the anterior scalene muscle, is usually the best location for the distal anastomosis. In patients with an internal thoracic artery coronary bypass graft, the subclavian artery distal to the internal thoracic artery should be used for the distal anastomosis to avoid myocardial ischemia. The skin incision can be either a low longitudinal, or a transverse supraclavicular incision. The longitudinal incision is made oblique along the anterior border of the sternocleidomastoid muscle, starting at the sternal notch. The dissection of the subclavian artery is best performed with the operating surgeon standing at the opposite side of the table and the patient positioned in a goiter operation position, with the neck extended (and rotated to the right) and the operating table in a reversed Trendelenburg position (C. Injury to the thoracic duct and sympathetic nerves should be avoided during dissection. We agree with Berguer that division of the internal 315 Carotid-subclavian or subclavian-carotid bypass After exposure of the arteries, as described above, the patient is heparinized. After placement of the clamps on the carotid artery, they are gently rotated medially 4560° in order to perform an easy anterior wall anastomosis, but have the graft lay lateral to the carotid artery once the clamps are removed. The graft is tunneled under the jugular vein, carefully avoiding injury to the thoracic duct on the left or the main lymphatic trunk on the right. The distal anastomosis between the graft and the subclavian artery is also performed in an end-to-side fashion, using running 5-0 or 6-0 monofilament suture. The graft can be tunneled retrosternally, in front of the neck under the platysma, protected half-way by the upper edge of the manubrium. Another, more direct path for a cross-over graft is the retropharyngeal space; the prosthesis is tunneled behind the esophagus, in front of the pre-vertebral lamina. The disadvantage of this technique is that both carotid arteries are cross-clamped at the same time; the use of a shunt in these patients is clearly warranted. Axillo-axillary bypass this operation was once quite popular for treating upper extremity ischemia or for providing inflow for a subclavian-based carotid reconstruction [54-60]. A later sternotomy in these patients obviously cannot be done without division of the graft first. Outcome of arch vessel reconstructions Published surgical results after cervical and extrathoracic reconstructions [38,40,43,47,52-66] have usually been excellent (Table 30. However, a comparison of published results between cervical and transthoracic reconstructions is frequently difficult since the operations are performed for different indications and in different types of patients. Most patients who undergo transthoracic repair are younger and have innominate artery or multivessel disease. On the other hand, most patients who have cervical reconstruction have either single vessel disease or multilevel disease with high risk for cardiac complications. Perioperative mortality was 2%, and 94% of the patients were relieved of symptoms. Early experience from our institution showed that when the type of procedure is carefully selected in patients with innominate artery disease, transthoracic endarterectomy provides results as good and durable as bypass grafting [9]. Still, more patients are candidates for aorticbased bypass procedures and this operation has become the favorite for arch vessel reconstruction. In a series of 58 patients, who underwent reconstruction of 92 arch vessels, our Mayo Clinic team reported a 3% early mortality and a 7% stroke rate [14]. Elevated serum creatinine and hypercoagulable states were predictors of adverse outcome. Primary and secondary graft patency rates at 5 years were 80% and 91%, respectively. Myocardial infarction and stroke are the two most frequent complications following innominate reconstructions, and both contribute to early mortality in these patients. Perioperative stroke rate can be decreased by careful technique to avoid cerebral embolization. Larger series report a decreased mortality and stroke rate in those patients who underwent reconstructions recently compared with those operated on earlier. In the experience of Berguer, mortality following 100 thoracic operations was 8%, and for 182 cervical operations it was 0. However, during a recent 10-year experience, the combined morbidity/mortality of each approach was only 3. In a group of 148 patients with atherosclerotic arch vessel disease, Kieffer et al.
© 2025 Adrive Pharma, All Rights Reserved..