General Information about Extra Super Cialis
Extra Super Cialis just isn't appropriate for everybody and should solely be used after consulting with a physician. Men with a historical past of heart illness, stroke, liver or kidney illness, or those taking medication for high blood pressure should exercise warning when utilizing this medication. It can be not suitable for men underneath the age of 18.
The beneficial dosage for Extra Super Cialis is one tablet taken orally 30 minutes before sexual activity. It is essential to note that this treatment shouldn't be taken more than as soon as each 24 hours. The effects of Extra Super Cialis can last for as much as 36 hours, giving males an extended window of alternative to have interaction in sexual exercise with out having to fret about erectile dysfunction.
Dapoxetine, however, is the part that addresses premature ejaculation. It is a selective serotonin reuptake inhibitor (SSRI) that helps to delay ejaculation by lowering the degrees of serotonin in the mind. This allows men to have better management over their ejaculation and prolong the sexual act, resulting in a extra satisfying sexual encounter for each partners.
As with any medication, Extra Super Cialis might have potential unwanted effects. The most commonly reported ones include headache, nausea, dizziness, and diarrhea. These side effects are normally delicate and subside with continued use of the medication. However, in the occasion that they persist or turn into bothersome, it is essential to consult a well being care provider.
Extra Super Cialis is a medication that combines Tadalafil and Dapoxetine to successfully deal with two widespread male sexual health issues - erectile dysfunction and premature ejaculation. It is a powerful and handy solution for males who wrestle with these conditions, offering relief and restoring confidence of their sexual skills.
It is also essential to mention that Extra Super Cialis shouldn't be taken with alcohol or grapefruit products as they will intervene with the effectiveness of the treatment. It is also not beneficial to take this medicine simultaneously with other erectile dysfunction drugs or any medication that contains nitrates.
Extra Super Cialis is out there in a tablet kind, with every tablet containing 40mg of Tadalafil and 60mg of Dapoxetine. This is a specially formulated mixture that provides the next dose of Tadalafil compared to different erectile dysfunction medicines, allowing for stronger and longer-lasting erections. Additionally, the inclusion of Dapoxetine ensures that men not only have a passable erection, but also have the ability to last more in bed.
In conclusion, Extra Super Cialis is a potent combination of Tadalafil and Dapoxetine that gives effective aid for both erectile dysfunction and premature ejaculation. It provides males a longer window of opportunity for sexual exercise, with out having to worry concerning the effectiveness of the medication. With correct utilization and warning, Extra Super Cialis can help males regain their sexual confidence and revel in a more fulfilling intercourse life.
Tadalafil is the active ingredient in Extra Super Cialis that's used to deal with erectile dysfunction. It works by rising blood circulate to the penis, permitting for a firmer and longer-lasting erection. This helps males to realize and maintain a satisfactory erection, a vital element in a satisfying sexual experience.
Cutaneous pseudolymphomas associated with infectious organisms (such as Borrelia burgdorferirelated lymphocytoma) commonly arise in regions with endemic infection for the responsible organisms erectile dysfunction hormone treatment buy extra super cialis with a mastercard. On the other hand, there has been a rise in the number of cases of Borrelia lymphocytoma in countries where Borrelia species are absent, in patients returning from travels in endemic regions. The lesions are often solitary or regionally clustered but may also be generalized in distribution, and even erythroderma may be observed. The lesions may persist for weeks, months, or even years; they may resolve spontaneously, and they may recur unpredictably. Histologic criteria for the diagnosis of cutaneous pseudolymphomas include two main features: (i) the architectural pattern of the infiltrates and (ii) the cellular composition of those infiltrates, which frequently show a mixed character. These histologic features need to be integrated carefully with the immunophenotypical data. Although, as a rule, malignant lymphomas reveal a monoclonal population of lymphocytes whereas pseudolymphomas show a polyclonal infiltrate, it must be underlined that demonstration of monoclonality may be lacking in true malignant lymphomas and that a distinct proportion of cutaneous pseudolymphomas harbor a monoclonal T or Bcell population. In addition, pseudoclonality represents a pitfall in cutaneous infiltrates, particularly when results are interpreted without knowledge of other data [1]. Although highthroughput sequencing may be more sensitive for analysis of clonal populations of T lymphocytes [24], data on reactive cutaneous conditions are still lacking; thus specificity has not yet been tested adequately. In this context, it must be clearly stated that differentiation of benign from malignant lymphoid infiltrates of the skin is possible only after careful synthesis and integration of the clinical, histopathologic, immunophenotypical, and molecular features. It is important not to overdiagnose cutaneous malignant lymphomas, and in some unclear cases a descriptive term such as "cutaneous atypical lymphoid proliferation" may be a useful working diagnosis for unclear cases (see Chapter 29). Cutaneous pseudolymphomas are traditionally divided into T and Bcell variants according to the histopathologic and immunophenotypical features, but in many conditions this distinction is artificial. In addition, in many instances, both T and B lymphocytes are present within the infiltrate of a given pseudolymphoma. Thus, in what follows cutaneous pseudolymphomas will be classified according to specific clinicopathologic entities (Table 28. In addition, the disease is one of the rarest among the pseudolymphomas; thus the diagnosis should be made only when compelling evidence is present and can be accepted only when confirmed by pathologic phototesting. Although "progression" into Tcell lymphoma has been reported, it seems more likely that these cases represented examples of undiagnosed mycosis fungoides or Sézary syndrome from the onset and that actinic reticuloid is not a potential precursor of cutaneous Tcell lymphomas [5]. Actinic reticuloid is a severe persistent photodermatitis that usually affects older men. A "leonine" face with deep furrowing of markedly thickened skin as well as diffuse alopecia can also be seen. When present, the features of lichen simplex chronicus superimposed upon an inflammatory process are helpful in distinguishing actinic reticuloid from mycosis fungoides and Sézary syndrome. The clinical differentiation of actinic reticuloid from mycosis fungoides and Sézary syndrome can be difficult because circulating cerebriform lymphocytes may be found in the peripheral blood of patients with actinic reticuloid [11]. Thelper lymphocytes are invariably predominating in Sézary syndrome, whereas Tcytotoxic cells are numerous in actinic reticuloid. Erythematous, scaly, lichenified lesions with scratching artifacts on the arm and back of hand. Suberythroderma causing complete involvement of the face by erythematous, scaly lesions. In patients with actinic reticuloid, the minimal erythema dose is lower than normal. Treatment of chronic actinic dermatitis is difficult and numerous therapeutic approaches have been proposed [13]. Any relevant associated contact or photocontact allergens have to be identified and avoided. These authors described four patients with persistent allergic contact dermatitis proved by patch tests. The clinical picture and histologic features in their patients were highly suggestive of mycosis fungoides. A unique case due to methylisothiazolinone and the mixture of methylchloroisothiazolinone/methylisothiazolinone revealed dermal infiltrates with predominance of B lymphocytes and formation of germinal centers [17]. However, monoclonality can be observed in the majority of patch test lesions in patients with conventional contact dermatitis, demonstrating that the finding of a clonal population of T lymphocytes in such patients does not have any diagnostic implications [18]. Patch tests for a variety of common antigens can give a positive reaction in lymphomatoid contact dermatitis, and the diagnosis should be reserved for patients in whom the lymphomatoid skin lesions are caused by a positively reacting antigen. For the management of patients, a thorough search for antigens is necessary in order to interrupt the process. When contact with the responsible allergens is avoided, the lesions heal in a relatively short time. Although lymphomatoid contact dermatitis has been reported to evolve into true malignant lymphoma, it is more likely that such patients had malignant lymphoma from the outset. The differentiation is determined mainly on the basis of changes within the epidermis, which shows variable acanthosis and spongiosis. In fact, to a certain extent follicular mucinosis may be regarded as a cutaneous histopathological pattern, akin to other nonspecific findings such as epidermolytic hyperkeratosis or acantholytic dyskeratosis, among many others. Isolated follicles with features of follicular mucinosis may be observed in unrelated inflammatory and neoplastic skin conditions such as squamous cell carcinoma, insect bite reactions, and acne vulgaris, among many others [19]. In some patients, dense perifollicular infiltrates with pilotropic lymphocytes but without deposition of mucin within the hair follicles represent also a mimic of pilotropic mycosis fungoides. As pilotropic mycosis fungoides in several cases does not show follicular deposition of mucin, these cases, too, represent a pitfall in the histopathological diagnosis. Recognition of the clinicopathological features of the background condition allows to properly classify these cases. As neoplastic cells of mycosis fungoides may colonize skin lesions of other conditions, the theoretical possibility of a specific manifestation of the disease at the site of an inflammatory dermatosis cannot be ruled out completely. For practical purposes, however, the finding of hair follicles showing follicular mucinosis in otherwise different diseases and without skin signs of mycosis fungoides should not be overdiagnosed as follicular mycosis fungoides and rather interpreted as a nonspecific histopathological pattern.
One potential pitfall may be represented by the presence of small oligoclonal populations of reactive T and B lymphocytes within the infiltrate impotence in the bible extra super cialis 100 mg on line. Complex karyotypes and chromosomal abnormalities involving chromosomes 5q, 6q, 12p, 13q, 15q, and 9 have been observed in blastic plasmacytoid dendritic cell neoplasm [3]. Gain of chromosomes 7q and 22 and loss of chromosomes 3p and 13q were demonstrated by comparative genome hybri dization in one study [49], while recurrent deletion of regions on chromosome 4 (4q34), chromosome 9 (9p13p11 and 9q12 q34), and chromosome 13 (13q12q31) was found in another study [12], and losses of 9/9p and 13q and gain of 7 in a third [50]. The least common denominator of these studies seems to be the presence of abnormalities involving chromosomes 9 and 13, confirmed by subsequent studies showing aberrations located at the 9p21. Wholeexome sequencing analysis of three cases of blastic plasmacytoid dendritic cell neoplasms confirmed the relation ship to the myeloid leukemias [59]. In my experience, this pattern is the exception rather than the rule, and negativity (b) is observed more frequently. Although systemic chemotherapy is usually followed by rapid, complete primary responses, remissions are short and recur rences are the rule [60]. Good response has been observed with lasparaginase in association with methotrexate and dexameth asone [61a], and asparaginase with high dose methotrexate is considered as a firstline treatment [61b]. Bortezomib has been used with good results in some patients [62], sometimes in association with lenalidomide and dexamethasone [63]. Response has been observed in some patients after the administration of pralatrexate and enasidenib [64]. The only curative option, however, seems to be allogeneic stem cell trans plantation [11, 6568]. Patients presenting with primary cuta neous disorder should be treated in the same aggressive manner as those with systemic involvement. On a mouse model, the epigenetic drugs 5azacytidine and decitabine were able to control disease progression in vivo [58]. Prognosis Blastic plasmacytoid dendritic cell neoplasm is a very aggressive disorder and the prognosis is very poor. Although presentation with solitary or localized skin lesions may be associated with a less aggressive course, at present, there is no evidence that longterm survival can be achieved with conventional treatments, even for these patients. As already mentioned, allogeneic bone marrow trans plantation yields better results and should be offered as the first therapeutic option whenever possible [11, 6668]. Young age (<40 years) and TdT expression in >50% of the neoplastic cells were independent prognostic variables associ ated with a better prognosis in one study [41], confirmed by the subsequent finding of better survival in pediatric cases [24]. Skin involvement seems to represent an unfavorable prognostic sign both in children and adult patients [24, 73]. As already mentioned, however, cutaneous manifestations are found in the vast majority of cases. Solitary, localized or generalized plaques and tumors, sometimes with a "bruise like" aspect. Usually monomorphous infiltrate of mediumsized cells within the entire dermis and subcutis. Complex karyotypes and chromosomal abnormalities involving chromosomes 5q, 6q, 12p, 13q, 15q, and 9. It is a rare entity, associated in most cases with chronic myelo monocytic leukemia or, more rarely, myelodysplasia and acute leukemias with monocytic differentiation. Their relationship to the underlying myeloid neoplasm has been demonstrated by the finding of identical clonal chromosomal abnormalities in the two cellular components. Although the exact nosology of this proliferation is yet unclear, it should not be considered to be a "pseudolymphoma," as its neoplastic nature is confirmed by the finding of genetic aberrations similar to those of the underlying leukemia. Apoptosis may be prominent, representing a further differential diagnostic clue from blastic plasmacytoid dendritic cell neoplasm. Treatment of the underlying myeloid neoplasm may result in the regression of the cutaneous plasmacytoid dendritic cell infiltrates, but prognosis is usually poor with a median survival of 11 months (related to the original leukemia rather than directly to the infiltrates of mature plasmacytoid dendritic cells) [44, 75]. Blastic natural killercell lymphoma of the skin associated with myelodysplastic syndrome of myelogenous leukaemia: a coincidence or more Cutaneous presentation of steroid responsive blastoid natural killer cell lymphoma. Plasmacytoid dendritic cells: a new cutaneous dendritic cell subset with distinct role in inflammatory skin diseases. Incidental diagnosis of blastic plas macytoid dendritic cell neoplasm in skin excision for basal cell car cinoma. Cutaneous manifestations of blastic plasmacytoid dendritic cell neoplasm morphologic and phenotypic variability in a series of 33 patients. Optimized immunohisto chemical panel to differentiate myeloid sarcoma from blastic plas macytoid dendritic cell neoplasm. Cytoplasmic nucleophos min is not detected in blastic plasmacytoid dendritic cell neoplasm. Genomic alterations in blastic natural killer/extranodal natural killerlike T cell lymphoma with cutaneous involvement. Twentyone cases of blastic plasmacytoid dendritic cell neoplasm: focus on biallelic locus 9p21. Blastic plasmacytoid dendritic cell neoplasm: genomics mark epigenetic dysregulation as a pri mary therapeutic target. Lasparaginase with meth otrexate and dexamethasone is an effective treatment combination in blastic plasmacytoid dendritic cell neoplasm. How should we diagnose and treat blastic plasmacytoid dendritic cell neoplasm patients Bortezomib as a new therapeutic approach for blastic plasmacytoid dendritic cell neo plasm. The lenalidomide/bort ezomib/dexamethasone regimen for the treatment of blastic plas macytoid dendritic cell neoplasm.
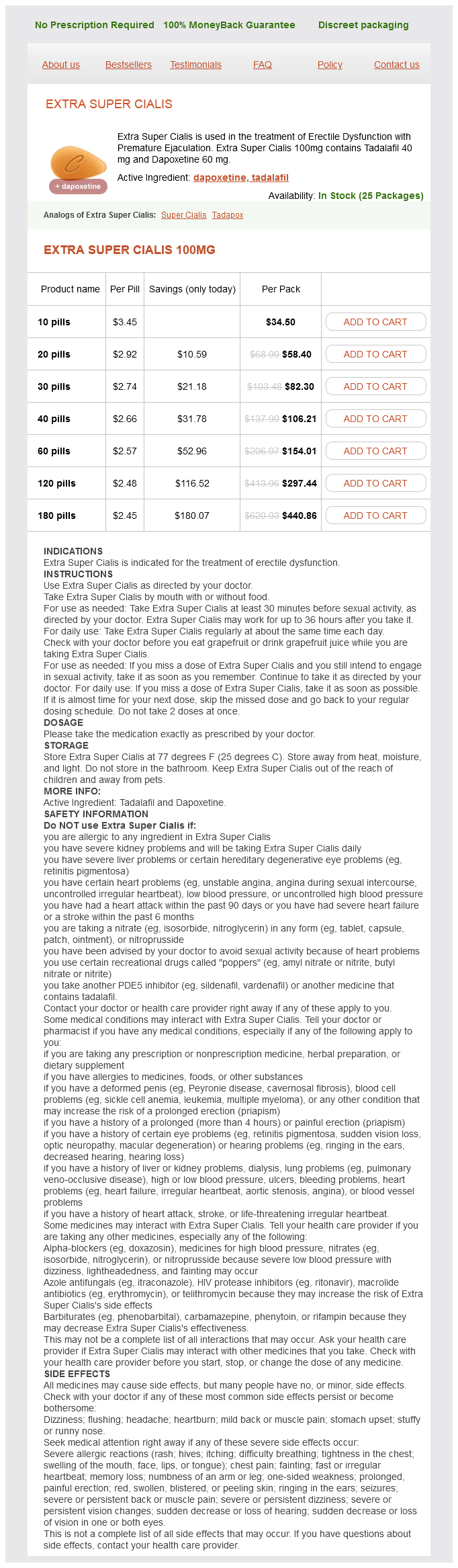
Extra Super Cialis Dosage and Price
Extra Super Cialis 100mg
- 10 pills - $34.50
- 20 pills - $58.40
- 30 pills - $82.30
- 40 pills - $106.21
- 60 pills - $154.01
- 120 pills - $297.44
- 180 pills - $440.86
The clinicopathologic and prognostic features are similar to those observed in adults impotence natural remedies extra super cialis 100 mg purchase amex. Considering primary and secondary cases together, cutaneous lymphoblastic lymphoma is not uncommon in pediatric patients and represents an important differential diagnosis of rapidly growing tumors, particularly on the head and neck area. Cutaneous Blymphoblastic lymphoma is much more common than cutaneous Tlymphoblastic lymphoma (both in adults and in children). Paediatric cutaneous lymphoma in Korea: a retrospective study at a single institution. Clonal rearrangement of the T cell receptor beta gene in the circulating lymphocytes of erythrodermic follicular mucinosis. Retrospective analysis of nonanaplastic peripheral Tcell lymphoma in pediatric patients in Japan. Angioimmunoblastische Lymphadenopathie mit kutanen Manifestationen bei einem 13jährigen Mädchen. Cutaneous lymphomas in adolescents and young adults: Clinical spectrum and physician-reported and patient-reported outcomes. Clinicopathological features and Tcell receptor gene rearrangement findings of mycosis fungoides in patients younger than age 20 years. Mycosis fungoides in Arab children and adolescents: a report of 36 patients from Kuwait. Mycosis fungoides in the pediatric population: report from an international childhood registry of cutaneous lymphoma. Clinical presentation, immunopathology, and treatment of juvenileonset mycosis fungoides: a case series of 34 patients. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. Pediatric follicular mucinosis: presentation, histopathology, molecular genetics, treatment, and outcomes over an 11year period at the Mayo Clinic. Pediatric primary follicular mucinosis: further evidence of its relationship with mycosis fungoides. Pagetoid reticulosis (WoringerKolopp disease) in a 2yearold girl-case report and review of the literature. Granulomatous slack skin with systemic involvement and a fatal outcome in an adolescent. An association with pityriasis lichenoides et varioliformis acuta in young children. Borra T, Custrin A, Saggini A, FinkPuches R, Cota C, Vermi W, Facchetti F, Cerroni L. The transformation of pityriasis lichenoides chronica into parakeratosis variegata in an 11yearold girl. Lymphomatoid papulosis in children: a study of 10 children registered by the Dutch cutaneous lymphoma working group. Subcutaneous panniculitis like Tcell lymphoma in the pediatric age group: a lymphoma of low malignant potential. Lupus erythematosus panniculitis in children: report of three cases and review of previously reported cases. Clonal cytophagic histiocytic panniculitis in children may be cured by cyclosporine A. Primary cutaneous Tcell lymphomas showing gammadelta phenotype and predominantly epidermotropic pattern are clinicopathologically distinct from classic primary cutaneous Tcell lymphomas. Edematous, scarring vasculitic panniculitis: a new multisystemic disease with malignant potential. Hydroa vacciniformelike cutaneous Tcell lymphoma: clinicopathologic and immunohistochemical study of 12 cases. EpsteinBarr virusassociated hydroa vacciniforme like cutaneous lymphoma in seven Chinese children. Two pediatric cases of primary cutaneous Bcell lymphoma and review of the literature. Paediatric primary cutaneous marginal zone Bcell lymphoma: does it differ from its adult counterpart Blastic plasmacytoid dendritic cell neoplasm in children: diagnostic features and clinical implications. Lymphoblastic lymphoma presenting in cutaneous sites: a clinicopathologic analysis of six cases. Although "pseudolymphoma" is usually considered as a synonym of a benign condition, some nonlymphoid malignant tumors may also simulate the picture of a cutaneous lymphoma (see the section on "malignant" pseudolymphomas in this chapter). In this context, it must be underlined that the term "pseudolymphoma" is not a diagnosis per se and should not be used to classify given cases, as it encompasses skin conditions with different etiologies, pathogeneses, clinicopathologic presentations, and behavior. Reading the pertinent literature one gets the impression that the number of cutaneous "pseudolymphomas" increases regularly. Some of the published cases represent reactive conditions that in rare exceptions may simulate histopathologically a cutaneous lymphoma, usually mycosis fungoides. This problem is discussed in the section on other "accidental" pseudolymphomas in this chapter, in order to underline that these conditions do not represent in general a pseudolymphoma, but rather may simulate a lymphoma in exceptional cases only. Pseudolymphomas are reactive, inflammatory conditions and should not be lumped together with cases considered to be at the edge between benign and malignant disorders. In this context, it must be underlined that true "progression" from a clearcut cutaneous pseudolymphoma into a malignant lymphoma of the skin is exceptionally rare. There are no exact data concerning the incidence, prevalence, and geographic distribution of cutaneous pseudolymphomas.
© 2025 Adrive Pharma, All Rights Reserved..