General Information about Erythromycin
This versatile antibiotic is mostly used to treat respiratory tract infections, corresponding to pneumonia, bronchitis, and sinusitis. It can also be effective in treating skin and delicate tissue infections, such as pimples, impetigo, and cellulitis. In addition, erythromycin can be utilized to treat sure sexually transmitted illnesses, including chlamydia and gonorrhea.
In recent years, there has been rising concern concerning the overuse of antibiotics resulting in the development of antibiotic-resistant micro organism. To fight this issue, it's essential to solely take erythromycin as prescribed by a well being care provider and to finish the entire course of treatment, even when signs improve. Failure to take action can lead to the bacteria turning into proof against the medicine, making it much less effective sooner or later.
In conclusion, erythromycin is a potent antibiotic that has been relied upon for many years to deal with a extensive range of bacterial infections. Its capability to target and kill micro organism, even those resistant to other antibiotics, makes it a vital tool in the treatment of many diseases. While there are potential side effects and precautions to consider, when used accurately, erythromycin is a useful and effective medicine for combating bacterial infections.
One of the main benefits of erythromycin is its ability to deal with infections attributable to bacteria that are resistant to different types of antibiotics. This makes it a valuable option for sufferers who are allergic to penicillin or other antibiotics. Erythromycin is also thought of protected for use during being pregnant, making it a helpful alternative for anticipating moms who want remedy for a bacterial infection.
As with any antibiotic, there are potential side effects associated with erythromycin. The most common include nausea, vomiting, diarrhea, and abdominal pain. These side effects are often gentle and may be managed by taking the treatment with food. More critical unwanted effects, while rare, could embody allergic reactions, extreme abdomen pain, and liver problems. It is essential to consult a well being care provider if any of these unwanted effects occur.
Originally discovered in 1952, erythromycin was the primary macrolide antibiotic to be developed. It was initially extracted from the bacteria Streptomyces erythreus, however now the drug is produced synthetically in laboratories. Its name is derived from the Greek word “erythros,” which means purple, due to its reddish colour.
Erythromycin is a powerful antibiotic that has been used for decades to treat all kinds of bacterial infections. It belongs to the macrolide class of antibiotics and works by stopping the growth of bacteria, preventing them from spreading and causing further damage.
Erythromycin may interact with other medicines, so it may be very important inform your physician of some other medicine you're taking. This contains over-the-counter medicines, natural supplements, and nutritional vitamins. Some medications, such as antacids, can reduce the effectiveness of erythromycin, while others, such as blood thinners, can improve the danger of unwanted aspect effects.
Erythromycin is available in a quantity of totally different types, together with tablets, capsules, and oral suspensions. It can be administered intravenously in severe cases. The dosage and frequency of administration will range depending on the type and severity of the infection being handled, in addition to the patient’s age and medical history.
Chemoradiotherapy antibiotics for acne and rosacea discount 500 mg erythromycin visa, with adjuvant surgery for local control, confers a durable survival advantage in adenocarcinoma and squamous cell carcinoma of the esophagus. Effects of neoadjuvant radiochemotherapy on pathological staging and prognosis for locally advanced esophageal squamous cell carcinoma. Long-term efficacy of perioperative chemoradiotherapy on esophageal squamous cell carcinoma. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. Curative resection for esophageal adenocarcinoma: analysis of 100 en bloc esophagectomies. Pattern of recurrence following radical oesophagectomy with two-field lymphadenectomy. To obtain the best results, the management of esophageal cancer should be individualized and based on a combination of factors including the physiologic status of the patient, tumor type and location, and stage of disease. In this article, we describe the different open surgical approaches to remove the esophagus in patients with esophageal cancer. Although minimally invasive techniques (see Chapter 39B) are increasingly applied, the benefits of fully minimally invasive esophagectomy have not yet been proven unequivocally, and an open or hybrid esophagectomy remains the standard procedure to remove the esophagus in many leading high-volume centers worldwide. The strong etiologic ties between (squamous cell) cancer of the esophagus and alcohol and tobacco usage make it imperative that patients be carefully screened for the presence of cardiovascular, pulmonary, and hepatic dysfunction regardless of their age. It has been estimated that between 20% and 30% of patients with esophageal cancer will have evidence of cardiovascular disease if carefully screened. Well-compensated cirrhosis (Child classification A) alone is not a contraindication to resection of an otherwise curable esophageal cancer, but one should be careful when considering resection in the setting of more advanced stages of cirrhosis, especially in the presence of ascites. Furthermore, patients who are planned to undergo neoadjuvant chemo(radio)therapy should be screened for renal insufficiency. Historically, the Ivor-Lewis procedure has been widely applied, including a thoracotomy with limited lymphadenectomy and thoracic anastomosis. With extensive two-field lymphadenectomy (upper abdomen and posterior mediastinum), this technique attempts to increase locoregional tumor control by enhancing the radicality of the resection. Advanced age alone should not be considered a contraindication for esophageal resection. Although the risk of mortality is higher in patients older than 70 years of age, this increased risk is due to the higher frequency of medical comorbidities such as heart, liver, and kidney disease in the elderly population rather than age per se. Surgery, most of the time combined with neoadjuvant therapy in current practice, offers the highest likelihood of cure for patients with locoregional disease. Although minimally invasive techniques are increasingly applied, the benefits of fully minimally invasive esophagectomy have not yet been proven unequivocally, and an open or hybrid esophagectomy remains the standard procedure to remove the esophagus in many leading high-volume centers worldwide. However, high-quality clinical evidence on the optimal extent of lymphadenectomy is absent, especially in the present era of neoadjuvant treatment. Consequently, individual opinions and institutional preferences currently dominate the choice of surgical technique and extent of lymphadenectomy. The proximal anastomosis is performed either through an extra incision made at the left side of the neck or in the chest (see "Anastomosis"). When a cervical anastomosis is performed, the procedure starts with a thoracotomy followed by the abdominal part of the operation, whereas in case of an intrathoracic anastomosis the laparotomy is performed prior to the thoracic phase. The thoracic dissection includes removal of the azygos vein with its associated nodes, the thoracic duct, and the paratracheal, subcarinal, paraesophageal, and parahiatal nodes in continuity with the resected esophagus. The block of tissue removed is bounded laterally on each side by the excised mediastinal pleura, anteriorly by the pericardium and membranous part of the trachea, and posteriorly by the aorta and vertebral bodies. During the thoracic phase the patient is placed in the left lateral decubitus position with a posterolateral thoracotomy performed entering the chest through the fifth or sixth intercostal space. The inferior pulmonary ligament is divided to the level of the inferior pulmonary vein. The pleura overlying the right main bronchus is divided, taking into account its membranous part. The pleura lying on both sides of the azygos arch is incised, and the arch is ligated or closed with a stapling device and subsequently transected. The pleura cranial to the azygos arch is incised and saved to create a pedicled "flap" to cover the subsequent intrathoracic anastomosis. The right paratracheal nodes are removed in between the trachea, superior vena cava, and the azygos arch. The vagal nerve should not be divided with use of electrocautery to prevent injury to the right recurrent nerve. The pleura overlying the lateral aspect of the vertebral bodies is incised from the level of the azygos arch to the diaphragm, and the intercostal veins are divided between ligatures or clips where they enter the azygos vein. A dissection plane is then created following each intact intercostal artery to reach the adventitial plane of the aorta. Dissection continues across the anterior surface of the aorta until the left mediastinal pleura is reached. Direct branches of the thoracic aorta to the esophagus should be carefully ligated before dividing. One or two communicating veins to the hemiazygos need to be ligated as they pass behind the aorta. The mediastinal tissue posteriorly between the azygos vein and the aorta just above the diaphragm includes the thoracic duct, which should be identified and transected at this stage.
Epidemiology and cost of ventral hernia repair: making the case for hernia research antibiotics for sinus infection what kind discount erythromycin uk. Tension of knotted surgical sutures shows tissue specific rapid loss in a rodent model. Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. A multicenter randomized controlled trial evaluating the effect of small stitches on the incidence of incisional hernia in midline incisions. Cost analysis of the use of small stitches when closing midline abdominal incisions. Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Laparoscopic ventral hernia repair: a comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. The enhanced viewtotally extraperitoneal technique for repair of inguinal hernia. Endoscopicassisted linea alba reconstruction plus mesh augmentation for treatment of umbilical and/or epigastric hernias and rectus abdominis diastasis-early results. Laparoscopic transversus abdominis release, a novel minimally invasive approach to complex abdominal wall reconstruction. Robot-assisted laparoscopic mesh repair of incisional hernias with exclusive intracorporeal suturing: a pilot study. Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Randomized clinical trial of mesh versus sutured wound closure after open abdominal aortic aneurysm surgery. Systematic review and meta-analysis of prophylactic mesh placement for prevention of incisional hernia following midline laparotomy. High incidence of trocar site hernia after laparoscopic or robotic Roux-en-Y gastric bypass. Port-site hernias occurring after the use of bladeless radially expanding trocars. Incidence of port-site incisional hernia after single-incision laparoscopic surgery. Survey on ventral hernias: surgeon indications, contraindications, and management of large ventral hernias. Analysis of ventral hernia repair in the obese: defining the goals of preoperative weight loss; 2016. Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Comparative analysis of biologic versus synthetic mesh outcomes in contaminated hernia repairs. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Robot-assisted laparoscopic repair of ventral hernia with intracorporeal suturing. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Endoscopic versus open component separation in complex abdominal wall reconstruction. Minimally invasive component separation results in fewer wound-healing complications than open component separation for large ventral hernia repairs. Long-term outcome of 254 complex incisional hernia repairs using the modified Rives-Stoppa technique. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Abdominal wall reconstruction: a comparison of totally extraperitoneal and transabdominal preperitoneal approaches. Benefits of multimodal enhanced recovery pathway in patients undergoing open ventral hernia repair. Sandhu Kamran Samakar nguinal hernia repair is a frequently performed operation, and laparoscopic inguinal hernia repair has become increasingly prevalent, particularly for the repair of bilateral or recurrent hernias. The first described laparoscopic inguinal hernia repair was completed in 1990 by Ger in canines1; the procedure has since evolved to include the use of a prosthetic mesh to cover the myopectineal orifice. This article reviews the anatomy, technical considerations, benefits, and possible complications of laparoscopic inguinal hernia repair. The paired medial umbilical ligaments are remnants of the fetal umbilical arteries. The inferior epigastric vessels originate from the external iliac vessels and have a peritoneal covering creating the paired lateral umbilical folds. These folds originate medial to the deep inguinal ring and travel to the arcuate line, where the inferior epigastric vessels enter the rectus sheath. The medial inguinal fossa is the space located between the medial umbilical ligament and lateral umbilical fold bilaterally.
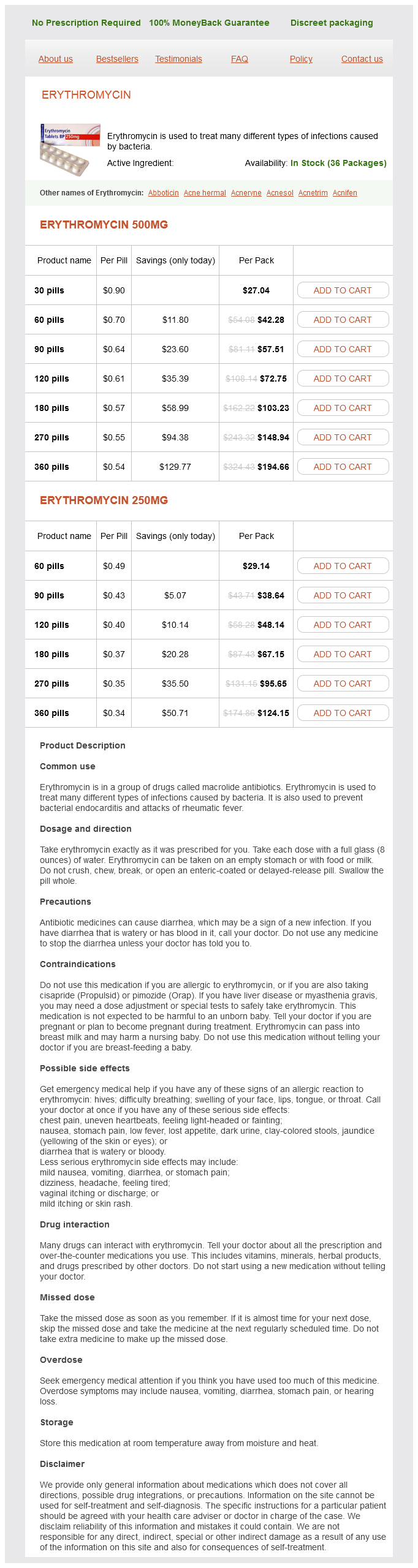
Erythromycin Dosage and Price
Erythromycin 500mg
- 30 pills - $27.04
- 60 pills - $42.28
- 90 pills - $57.51
- 120 pills - $72.75
- 180 pills - $103.23
- 270 pills - $148.94
- 360 pills - $194.66
Erythromycin 250mg
- 60 pills - $29.14
- 90 pills - $38.64
- 120 pills - $48.14
- 180 pills - $67.15
- 270 pills - $95.65
- 360 pills - $124.15
Multiple randomized clinical trials have proven that alvimopan reduces time to return of bowel function infection near eye best purchase for erythromycin. A wide array of conditions with overlapping clinical presentations and few unique objective signs prevents facile diagnosis. The physician must carefully assemble the history, context, and judiciously chosen tests to identify the malady. Most pharmacologic interventions date back decades and have either limited efficacy and/or severe side effects, although recent research is identifying novel regimens. Surgical interventions, through implantable devices or alteration of normal anatomy, have limited efficacy in many cases and carry significant risks of their own. Despite these challenges, gastric and intestinal dysmotility affect several thousand patients and carry substantial morbidity. Thus, a thorough investigation for mechanical causes ought to be pursued, including both axial imaging and barium swallow studies as needed. Endoscopy can also be informative while simultaneously harvesting biopsy samples from the gastric, duodenal, and proximal jejunal mucosa for pathological investigation. If all the above fail to elicit a diagnosis, surgeons may be asked to perform a diagnostic laparoscopy or, more rarely, laparotomy. Surgeons can also collect full-thickness jejunal biopsies to assess for visceral myopathy or neurogenic causes of small bowel dysmotility and chronic intestinal pseudoobstruction. Meilahn for his work on a prior version of this chapter that formed the foundation for the current iteration. Clinical response and side effects of metoclopramide: associations with clinical, demographic, and pharmacogenetic parameters. Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet. A double-blind multicenter comparison of domperidone and metoclopramide in the treatment of diabetic patients with symptoms of gastroparesis. Diabetic gastroparesis: treatment with domperidone-a double-blind, placebo-controlled trial. Domperidone and ventricular arrhythmia or sudden cardiac death: a population-based case-control study in the Netherlands. Clinical trial: effect of mitemcinal (a motilin agonist) on gastric emptying in patients with gastroparesis- a randomized, multicentre, placebo-controlled study. Ghrelin and motilin are cosecreted from a prominent endocrine cell population in the small intestine. The placebo response in functional bowel disorders: perspectives and putative mechanisms. Methods of gastric electrical stimulation and pacing: a review of their benefits and mechanisms of action in gastroparesis and obesity. Gastric electrical stimulation: an alternative surgical therapy for patients with gastroparesis. Erosion of gastric electrical stimulator electrodes: evaluation, management, and laparoscopic techniques. Systematic review and meta-analysis: gastric electrical stimulation for gastroparesis. Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. Treatment of refractory gastroparesis: gastric and jejunal tubes, botox, gastric electrical stimulation, and surgery. Severe gastrointestinal dysmotility in a patient with congenital myopathy: causal relationship to decrease of interstitial cells of Cajal. Absence of the interstitial cells of Cajal in patients with gastroparesis and correlation with clinical findings. A longitudinal study of gastric emptying and upper gastrointestinal symptoms in patients with diabetes mellitus. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom Index. Endoscopic pyloric injection of botulinum toxin-A for the treatment of postvagotomy gastroparesis. Motility of the antroduodenum in healthy and gastroparetics characterized by wireless motility capsule. Appraisal of medium-and long-term treatment of gastro paresis and chronic intestinal dysmotility. Effect of cigarette smoking on gastric emptying of solids in Japanese smokers: a crossover study using the 13C-octanoic acid breath test. Metoclopramide to treat gastroparesis due to diabetes mellitus: a double-blind, controlled trial. Chronic intestinal pseudoobstruction associated with altered interstitial cells of Cajal networks. Intestinal surgical resection disrupts electrical rhythmicity, neural responses, and interstitial cell networks. The early diagnosis of acute intestinal obstruction with comments on pathology and treatment: with a report on successful decompression of three cases of mechanical small bowel obstruction by nasal catheter siphonage. Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Effect of octreotide on intestinal motility and bacterial overgrowth in scleroderma. Alvimopan use, outcomes, and costs: a report from the Surgical Care and Outcomes Assessment Program Comparative Effectiveness Research Translation Network Collaborative. An evidence-based review of novel and emerging therapies for constipation in patients taking opioid analgesics.
© 2025 Adrive Pharma, All Rights Reserved..