General Information about Epitol
One of the principle makes use of of Epitol is within the treatment of epilepsy. Epilepsy is a neurological disorder that leads to recurrent seizures or episodes of uncontrolled electrical exercise in the mind. These seizures may cause a broad range of physical, emotional, and psychological disturbances, making it troublesome for people to hold out their day-to-day activities. Epitol works by stabilizing the electrical activity in the mind, which helps in reducing the frequency and severity of seizures.
Epitol can be seen as a beneficial treatment for the therapy of neuralgia of the trigeminal and glossopalatine nerves. Neuralgia is a pointy, shooting ache that happens as a result of irritation or damage to a nerve. When the trigeminal nerve (which is answerable for sensation within the face) or the glossopalatine nerve (which provides sensation to parts of the mouth) is affected, it can trigger severe and debilitating pain. Epitol helps to alleviate this pain by reducing the overactivity of the nerves.
Epitol, also recognized as Carbamazepine, is a broadly used medication for treating various neurological issues. It falls under the class of temper stabilizing brokers and antiepileptic medicines and is seen as a highly effective drug for both treating and stopping neurological disorders. In this text, we are going to take a extra in-depth take a look at what Epitol is, how it works, and its various uses within the medical subject.
In conclusion, Epitol is a highly efficient medication for the treatment of varied neurological disorders. Its versatility and effectiveness in treating epilepsy, bipolar dysfunction, alcoholic abstinence, neuralgia, and diabetic neuropathy make it a preferred choice amongst medical doctors and patients. However, like any other medication, it's crucial to follow the prescribed dosage and search medical advice before beginning treatment. With correct use, Epitol can significantly improve the quality of life for individuals with neurological issues.
Another use of Epitol is in the treatment of diabetic neuropathy. Diabetic neuropathy is harm to nerves brought on by uncontrolled diabetes. Symptoms embrace numbness, tingling, and pain within the arms and ft. Epitol may help enhance these symptoms by growing blood flow and decreasing nerve injury within the affected areas.
In addition to epilepsy, Epitol can be used to handle bipolar issues and prevent maniac-depressive episodes. Bipolar disorder is a condition that impacts an individual's temper, leading to excessive highs (mania) and lows (depression). Epitol helps to steadiness the mood swings and prevent severe episodes of mania or melancholy. This medication can be used in combination with other medicine for the therapy of alcohol withdrawal symptoms. The calming effect of Epitol may help scale back agitation and anxiety which are generally experienced throughout alcohol withdrawal.
Epitol is a prescription drug that is primarily used for the treatment of epilepsy (except for petit mal seizures). It can be used to handle maniacal conditions, prevent maniac-depressive frustration, and in addition within the remedy of alcohol withdrawal. Additionally, this treatment can successfully deal with neuralgia of the trigeminal and glossopalatine nerves, and diabetic neuropathy.
It is important to note that Epitol could cause some unwanted effects, especially when taken together with other drugs. The commonest side effects noticed embrace drowsiness, dizziness, nausea, and vomiting. In uncommon instances, it could additionally trigger extreme allergic reactions, liver damage, and low levels of blood cells. Therefore, you will want to consult a physician earlier than starting any new medicine and follow the recommended dosage rigorously.
The risk of an adverse reaction increases with age medications known to cause tinnitus epitol 100 mg purchase amex, with the greatest number occurring in patients older than 50 years. If a patient develops a chronic cough, the drug should be discontinued and a chest radiograph obtained. Fairley and his associates (1974) first reported on the prophylactic efficacy of 500 mg of cephalexin per day in preventing recurrent infections during a 6-month period of observation. Of the 22 patients, 17 remained free of infection, an impressive record because several patients had papillary necrosis, chronic pyelonephritis, and even renal calculi. Gower (1975) treated 25 women with 125 mg of cephalexin nightly for 6 to 12 months and found only 1 infection, whereas 13 of 25 women receiving a placebo had infection. Chapter12 InfectionsoftheUrinaryTract 273 Martinez and coworkers (1985) studied the effect on the vaginal and rectal flora of 250 mg of cephalexin nightly for 6 months in 23 patients with reinfections of the urinary tract. These results are in contrast to those of Preiksaitis and colleagues (1981), who found rectal Enterobacteriaceae resistance in 38% of patients when cephalexin was administered at a dose of 500 mg four times daily for 14 days. Cephalexin at 250 mg or less nightly is an excellent prophylactic agent because bowel flora resistance does not develop at this low dosage. With short-course fluoroquinolone therapy (Hooton et al, 1989), eradication of Enterobacteriaceae from the bowel and vaginal (Nord, 1988; Tartaglione et al, 1988) flora has been documented-observations that have been exploited in the use of these agents for prophylaxis. Of 11 women who completed 1 year of prophylaxis (200 mg orally), all remained free of infection. Low-dose continuous prophylaxis is indicated when the urine culture shows no growth (usually when a patient has completed antimicrobial therapy). These reported results of prophylaxis, together with agents and doses, have been summarized by Nicolle and Ronald (1987) (see Table 12-14). These studies consistently show a remarkable reduction in the reinfection rate from 2. Urinary antiseptics, such as methenamine mandelate or hippurate, have resulted in some decrease in recurrences, but they are not as effective as antimicrobial agents. Every-other-night therapy is also effective and is probably practiced by most patients. When breakthrough infections occur, they are not necessarily accompanied by symptoms; therefore we advocate monitoring for infections every 1 to 3 months, even in asymptomatic patients. Breakthrough infections usually respond to full-dose therapy with the drug used for prophylaxis. However, cultures and susceptibility tests may indicate that another drug is indicated. Low-dose prophylaxis is usually discontinued after about 6 months, and the patient is monitored for reinfection. Approximately 30% of women will have spontaneous remissions that last up to 6 months (Kraft and Stamey, 1977). Unfortunately, many of the remissions are followed by reinfections, and low-dose prophylaxis must be reinstituted. The patient is also provided a 3-day course of empirical, full-dose antimicrobial therapy to be started immediately after performing the culture. It is important that the antimicrobial agent selected for self-start therapy have a broad spectrum of activity and achieve high urinary levels to minimize development of resistant mutants. Fluoroquinolones are ideal for self-start therapy because they have a spectrum of activity broader than any of the other oral agents and are superior to many parenteral antimicrobials, including aminoglycosides. If the culture is positive and the patient is asymptomatic, a culture is performed 7 to 10 days after therapy to determine efficacy. In most cases, the therapy is limited to two inexpensive dip slide cultures and a short course of antimicrobial therapy. If the patient has symptoms that do not respond to initial antimicrobial therapy, a repeat culture and susceptibility testing of the initial culture specimen are performed and therapy adjusted accordingly. If symptoms of infection are not associated with positive cultures, urologic evaluation should be performed to rule out other causes of irritative bladder symptoms, including carcinoma in situ, interstitial cystitis, and neurogenic bladder dysfunction. Our experience with this technique has been very favorable and is particularly attractive to patients who have less frequent infections and are willing to play an active role in their diagnosis and management. Antimicrobial management through postintercourse prophylaxis is based on research establishing that sexual intercourse can be an important risk factor for acute cystitis in women (Nicolle et al, 1982). Cranberry juice contains proanthocyanidins that block adherence of pathogens to uroepithelial cells in vitro (Foo et al, 2000). Randomized trials in low-risk patients show that 200 to 750 mL daily of cranberry or lingonberry juice or cranberryconcentrate tablets reduce the risk of symptomatic, recurrent infection by 12% to 20% (Avorn et al, 1994; Kontiokari et al, 2001; Stothers, 2002; McMurdo et al, 2009). However, the actual cranberry content of juices and tablets varies substantially; therefore their efficacy is not predictable (Consumer Reports, 2001; Klein, 2002). Other factors, such as hygiene, frequency and timing of voiding, wiping patterns, use of hot tubs, and type of undergarments, have not been shown to predispose women to recurrent infection, and there is no rationale for giving women specific instructions regarding them. Although the classic symptoms of acute onset of fever, chills, and flank pain are usually indicative of renal infection, some patients with these symptoms do not have renal infection. Conversely, significant renal infection may be associated with an insidious onset of nonspecific local or systemic symptoms, or it may be entirely asymptomatic. Therefore a high clinical index of suspicion and appropriate radiologic and laboratory studies are required to establish the diagnosis of renal infection. Unfortunately, the relationship between laboratory findings and the presence of renal infection often is poor.
There is also increasing use of ureteroscopic treatment for patients with low-grade medicine 20th century epitol 100 mg generic, low-volume disease. Endoscopic management of these patients has proven to be a reasonable option, without compromise of patient survival (Cutress et al, 2012b; Grasso et al, 2012). Percutaneous nephroscopy and electroresection have been used and permit resection of large amounts of tumor (Irwin et al, 2010; Cutress et al, 2012a). However, the ureteroscopic approach may be preferred because it avoids the risk of seeding the percutaneous tract and retroperitoneum with tumor. The risk of tract seeding is small, but it has been reported (Sharma et al, 1994; Sengupta and Harewood, 1998). Chapter7 PrinciplesofUrologicEndoscopy 143 Equipment Semirigid Ureteroscopes Performance of successful ureteroscopy requires a variety of instrumentation-most important, appropriate and modern ureteroscopes. Although larger rod-lens rigid ureteroscopes are still available in some operating rooms, the smaller-diameter fiberoptic ureteroscopes are less traumatic, less often require ureteral dilation, and are equally effective. Semirigid ureteroscopes are smaller in diameter because of the incorporation of fiberoptics into their construction. Fiberoptic bundles are created from molten glass that has been pulled into small-diameter fibers. Each individual glass fiber is "cladded" with a second layer of glass of a different refractive index. This cladding improves the internal reflection, light transmission, and durability of the fiberoptic bundle. The meshlike appearance of the image from fiberoptic image bundles is caused by the lack of light transmission through this cladding. These fibers uniformly transmit light from one end of the fiber to the other proportional to the light input. The glass fibers of a fiberoptic bundle can be arranged randomly or in a precise orientation with identical location at each end of the fiber. When the fibers are grouped randomly, such as those within the light bundle, they provide excellent light transmission for illumination, but no image. When the fibers are arranged in a coherent fashion, the light from each fiber within the bundle will coalesce to transmit images. Small lenses are attached to the proximal and distal ends of the image bundle to create a telescope. By controlling the number of fibers in the bundle, and the type and orientation of the lenses, the manufacturers can determine the degree of image magnification, field of view, and focusing ability for different fiberoptic endoscopes. For example, by changing the axis of the lens at the distal tip of the image bundle, the angle of view of the ureteroscope can be changed to improve visibility of any working instruments passed out the working channel (Higashihara et al, 1990). Improvements in image bundle construction have allowed closer packing of more fibers, resulting in improved images, smaller outer diameters, and larger working channels in both rigid and flexible ureteroscopes. Another design modification is the splitting of the light bundle distally into two points of light transmission (Conlin et al, 1997). This makes possible a more centrally placed working channel as well as better distribution of the light within the working field of view. Current semirigid ureteroscopes typically have tip diameters of 7 Fr or smaller and working channels larger than 3 Fr. Semirigid ureteroscopes have either large single or two smaller individual working channels. An advantage of the separate working channels is the ability to irrigate through one unrestricted channel while a working instrument occupies the other. Separate working channels also permit passage of a lithotripsy device through the separate channel to fracture a stone that cannot be disengaged from a basket in the other channel. With a single channel, this can be difficult because of entanglement between the two working instruments. Eyepieces are commonly "in line" with the ureteroscope, which allows easy introduction of the scope. Offset eyepiece design makes possible a straight working channel for the use of more rigid working instruments such as rigid biopsy forceps or a pneumatic lithotripsy probe. Increased availability and use of the holmium laser for ureteroscopic lithotripsy has decreased the need for ureteroscopes with offset eyepieces. The advantages of the ureteroscopic approach include the ability to control the length and depth of the incision under direct vision, the avoidance of percutaneous renal access, and the ability to perform the procedure in an outpatient setting. There are two situations in which ureteroscopic endopyelotomy may not be the preferred approach. Patients with concomitant renal calculi should be treated via a percutaneous approach to allow simultaneous removal of the calculi and endopyelotomy. It may be best to limit ureteroscopic endopyelotomy to those patients without known crossing vessels, and treat those with crossing vessels with laparoscopic ureteropyeloplasty. Patients with ureteral strictures can also be managed from a ureteroscopic approach. Endoureterotomy will be less successful in patients with ureteral strictures longer than 1. Ureteroscopic incision of short ureteral strictures in otherwise healthy ureters is a reasonably successful treatment option. Other Indications for Ureteroscopy Diagnostic flexible ureteroscopy can be performed in patients with persistent positive cytology, filling defects, hematuria, and recurrent urinary tract infections localized to a single renal unit. With the miniaturization of flexible ureteroscopes, the safety of flexible ureteroscopy has increased significantly. Rather than relying on ureteropyelography alone, we can now safely and easily perform diagnostic ureteroscopy. Ureteroscopy has also been used for removal of foreign bodies including suture, proximally migrated ureteral stents, balloon catheters, and other fractured working instruments. The three-pronged grasping forceps are ideally suited for grasping and removing these foreign bodies.
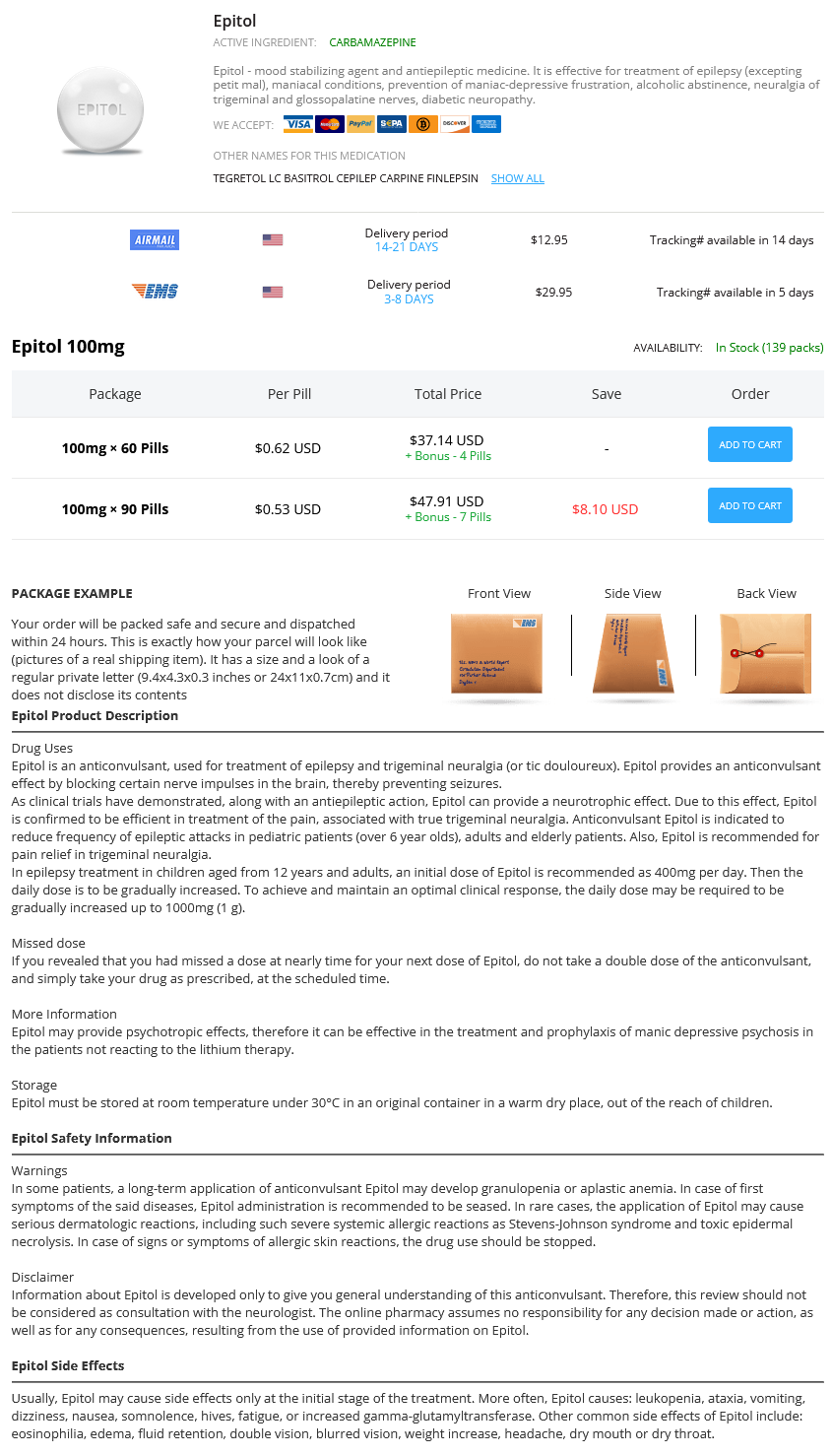
Epitol Dosage and Price
Epitol 100mg
- 60 pills - $37.14
- 90 pills - $47.91
Continuous quality improvement is the guiding principle for establishing a high-quality health care delivery system treatment centers of america order generic epitol pills, and relies on an electronic health record system as well as on quality improvement oversight (Pham et al, 2007; Gabow et al, 2012; Cosgrove et al, 2013). An electronic health record system can improve quality on the front end with electronic order entry, built-in order sets, and standardized clinical care pathways, and on the back end with facile data abstraction and reports built around broad sets of quality outcomes (Gabow and Mehler, 2011; Cosgrove et al, 2012). Electronic systems are easily modifiable for changing metrics over time, and cloud-based systems allow sharing of information between inpatient and outpatient facilities, as well as with other institutions (Schweitzer, 2012). Compared with other industries, information technology has been less aggressively adopted in health care (Menachemi et al, 2006; Simon et al, 2007). As of 2008, fewer than 20% of physicians used an electronic health record (DesRoches et al, 2008; Jha et al, 2009). Hospitals and physicians not using electronic health records by 2015 are subject to financial penalties under Medicare. Quality improvement oversight is typically undertaken by a quality improvement department, and involves data collection and monitoring systems, confidential reporting, and dashboards (Gabow et al, 2012). Such quality improvement projects have been piloted in urology but have not yet been implemented broadly (Gambone and Broder, 2007; Lee et al, 2011). Descriptive quality measures abound, but for quality metrics to affect outcomes, they must be based on solid evidence, be feasible, and have resources devoted to tracking and improvement. Congress passed the Patient Safety and Quality Improvement Act, which helped reinforce ongoing quality improvement initiatives and also launched several new initiatives to collect and disseminate performance information about medical care (Patient Safety and Quality Improvement Act, 2005). Hundreds of performance indicators have been collected in its National Library of Healthcare Indicators, and a root cause analysis system was developed to understand the causes of sentinel events. The Leapfrog Safe Practices Score assesses computer physician order entry, evidencebased hospital referral, and appropriate intensive care unit staffing. It holds an annual Patient Safety Congress and publishes the Journal of Patient Safety. The measures quantify risk-adjusted 30-day surgical outcomes, including mortality and morbidity in 21 categories. QualityConceptualFramework the conceptual framework for the measurement of quality of care in medicine was established almost 50 years ago by Donabedian (Donabedian, 1966). In this model, quality-of-care measures are categorized into three domains-structure, process, and outcome. Structure of Care Structure encompasses the fixed aspect of health care delivery and includes the space, equipment, human resources, and provider experience necessary to provide care. Structural measures specific to prostate cancer quality could include the presence of a multidisciplinary cancer center or psychological support services (Spencer et al, 2003). Although certain structural characteristics may be necessary to provide good care, they are usually insufficient to ensure highquality care. Therefore the best structural measures are those that can be shown to have a positive influence on the process of care and on patient outcomes (Brook and McGlynn, 1996). For proxy measures to be useful as quality measures, intervention should affect both the measure and the underlying disease (Guyatt et al, 1993; Girling et al, 2012). Quality-of-life assessment, typically by patient survey, provides a comprehensive evaluation of how the illness and its treatment affect patients. Surgeon volume is also associated with structural covariates such as lymph node count at the time of robotic cystectomy (Marshall et al, 2013). Hospitals with higher lymph node counts have been shown to have higher survival rates after radical cystectomy (Hollenbeck et al, 2008). Patients with renal trauma are more likely to be offered conservative management and have a lower chance of requiring multiple procedures if they are treated at a level 1 trauma center (Hotaling et al, 2012). Process of Care Process of care is the set of activities that goes on between patients and practitioners and is often divided into interpersonal process and technical process. Examples include antibiotic prophylaxis and discussion of treatment options (Wolf et al, 2008). Process measures are often considered to be the best measure of quality (Brook and McGlynn, 1996; Brook et al, 2000), and the most fertile area for improvement in value (Schneider et al, 2004; Malin et al, 2006). Interpersonal process refers to how the clinician relates to the patient and includes issues such as whether the clinician supplies sufficient information in a clear enough manner for the patient to make an informed treatment choice. Patient survey data are generally used to assess quality of interpersonal process. Technical process refers to whether medically appropriate decisions are made when diagnosing and treating the patient and whether care is provided in an effective and skillful manner-for instance, selecting the correct operative repair for female urethral stricture disease (Ackerman et al, 2010). One way to evaluate the appropriateness of medical treatment is to determine if the care provided is consistent with current medical knowledge and adheres to the professional standard. This assessment can be done by developing quality indicators, such as those delineated earlier, that describe a process of care that should occur for a particular type of patient in a specific clinical circumstance. To be valid, these quality indicators should be based on the evidence in the medical literature and on current professional standards of care. The performance of physicians and health plans is then assessed by calculating rates of adherence to the indicators for a sample of patients. Using quality indicators to evaluate appropriateness of care is relatively straightforward. However, assessing the effectiveness or skill of technical process of care is much more difficult. Indeed, direct observation may be necessary to assess the quality of technical process of care. Alternatively, it may be necessary to rely on measuring outcomes to evaluate whether care was provided in a skillful manner.
© 2025 Adrive Pharma, All Rights Reserved..