General Information about Enalapril
Enalapril can also be used to treat coronary heart failure, a condition in which the guts is unable to pump enough blood to fulfill the body's wants. This may cause fluid buildup within the lungs and extremities, leading to symptoms similar to shortness of breath, fatigue, and swelling within the legs and ft. By reducing blood strain and improving blood flow, enalapril may help to cut back the signs of coronary heart failure and enhance the quality of life for these dwelling with the condition.
Enalapril is out there in tablet form and is often taken once or twice a day, with or with out food. The dosage will depend upon the individual's condition and response to the medicine. It is important to take enalapril as prescribed and not to miss any doses, as this could have an result on the effectiveness of the treatment. It could take several weeks for the complete results of enalapril to be felt, so you will need to proceed taking it as directed even when there aren't any instant symptoms.
Like any treatment, enalapril may trigger unwanted effects in some people. The most common side effects embody dizziness, lightheadedness, and a dry cough. More severe unwanted facet effects, although uncommon, could include chest ache, problem respiration, and swelling of the face, throat, or extremities. It is essential to seek medical consideration if any of these symptoms happen.
Enalapril could work together with other medicines, so you will want to inform the doctor of some other medicines, dietary supplements, or natural cures being taken before beginning treatment. This consists of over-the-counter drugs similar to ibuprofen and naproxen, as properly as prescription medicines for other situations.
Enalapril, brand name Vasotec, is a generally prescribed medication for the therapy of hypertension, heart failure, and other heart-related conditions. It is classed as an angiotensin-converting enzyme (ACE) inhibitor, meaning it really works by blocking a pure substance in the body that constricts blood vessels and increases blood pressure.
In conclusion, enalapril, also recognized as Vasotec, is a generally prescribed treatment for the treatment of high blood pressure, coronary heart failure, and other heart-related situations. As an ACE inhibitor, it really works by enjoyable blood vessels and reducing blood pressure, reducing the risk of serious well being issues. It is essential to comply with the prescribed dosage and inform the physician of another drugs being taken to avoid potential interactions. With proper use, enalapril may help enhance the general health and well-being of these with heart problems.
In addition to high blood pressure and coronary heart failure, enalapril may be prescribed for other heart-related situations corresponding to diabetic nephropathy, a complication of diabetes that affects the kidneys, and left ventricular dysfunction, a situation in which the left facet of the guts is unable to pump blood effectively. It can also be used to forestall or manage coronary heart assaults in patients with a history of heart disease.
High blood pressure, also referred to as hypertension, is a medical condition by which the force of blood in opposition to the partitions of the arteries is persistently too excessive. Over time, this can result in serious health issues such as coronary heart illness, stroke, and organ harm. Enalapril works by serving to to loosen up and widen blood vessels, making it simpler for the center to pump blood and reducing the workload on the guts.
Historically blood pressure 50 year old male buy 5 mg enalapril mastercard, such patients had a relatively poor prognosis but the use of targeted therapy, such as the tyrosine kinase inhibitor, imatinib, has considerably improved responses. Days 1 and 15 of the cycle Days 25, 912, 1619 and 2326 Once daily Weekly for 4 weeks 30 mg/m2 1. Days 15 of each cycle Days 15 of each cycle Day 5 of cycle 1 only Once per cycle Further cycle the same as consolidation (4 weeks) Maintenance for 2 years Vincristine Prednisolone Mercaptopurine Methotrexate 1. Once every 3 months For 5 days every 3 monthsw Every day Once weekly Every 3 months 876 Methotrexate i. The figure demonstrates that patients are treated with initial induction therapy, then remission is consolidated with at least two courses of chemotherapy. Patients are assessed for the necessity and their suitability for allogeneic stem cell transplant during this treatment. This figure provides a summary only and should not be used as a guide to prescribing or dispensing therapy. Sadly, this is an indicator of a lack of progress in the therapy of this disease over the years. Whilst it is possible to achieve 80% remission rates, relapse rates remain high, with 5-year survival of 3540% in those younger than 60 years at diagnosis and 515% in those older than 60 years at diagnosis (Dohner et al. For this reason, many patients opt for treatment in the context of clinical trials. They have been used to develop individualised risk-adapted treatment strategies, particularly inluencing which patients. Unfortunately, the largest patient group identiied comprised those with a normal karyotype; a standard cytogenetic approach does not allow further risk stratiication in this group. It is worth stating, however, that our ability to detect mutations is improving very quickly; the current challenge is to understand the relative importance of such mutations, given that an individual patient may have several mutations, to be able to best apply this new knowledge for patient beneit. In patients younger than 40 years, myeloablative allogeneic bone marrow transplantation has resulted in disease-free survival of 4565% at 5 years post-transplant. Only about 10% of patients are suitable for myeloablative allogeneic bone marrow transplants, although reduced-intensity conditioning regimens have a more general applicability. This process is thought to increase the activity of some tumour-suppressor genes, resulting in anti-tumour effects. Whenever possible, patients who enter remission should be offered an allogeneic bone marrow transplant, as chemotherapy alone is unlikely to cure relapsed disease. This antibody, when used in combination with standard chemotherapy, seems to reduce relapse risk in all but the highest-risk patients. Concerns have been raised about possible toxicity in the form of veno-occlusive disease of the liver, and the dosing schedule is not yet optimised. Increasing numbers of such targeted therapies are likely to be tested in the next few years. Given the signiicant differences in cost between the two regimens, the latter currently remains the standard of care (Burnett et al. The side effects of hydroxycarbamide are generally mild but include rashes and gastro-intestinal disturbances. It promotes the expression of suppressed normal haemopoiesis at the expense of the malignant clone. In a large randomised controlled trial, patients were randomised to receive imatinib or a combination of interferon- and cytarabine. Many patients were intolerant of the interferon and cytarabine combination and crossed over to receive imatinib after trial commencement. The Philadelphia chromosome became undetectable in 68% of imatinib recipients compared with 7% of those in the alternative arm (Hughes et al. Treatment is slightly more successful if transformation is lymphoid rather than myeloid. Imatinib, typically at higher doses than are used in chronic phase disease, can also be used to attempt to return patients to chronic phase disease. There is no evidence that early treatment of asymptomatic patients improves outcome. Corticosteroids can reduce the lymphocyte count without contributing to myelosuppression and are used to treat autoimmune phenomena such as haemolytic anaemia and immune thrombocytopenia. However, no survival advantage for the use of fludarabine has been demonstrated (Rai et al. More recent studies have looked at the use of bendamustine, an intravenous alkylating agent. Chlorambucil, alone or in combination with rituximab, remains an excellent choice for patients with signiicant comorbidities because the treatment is less immunosuppressive. Binding of this antibody induces both antibodymediated and complement-mediated T-cell cytotoxicity against malignant B cells. Both of these agents are oral drugs which have targeted action so as to avoid the systemic effects seen with conventional chemotherapy agents. This susceptibility is increased because many treatments, such as campath-1H, ludarabine and bendamustine, have generalised anti-lymphocyte action and are not absolutely speciic for malignant lymphocytes. Stem cell transplantation the potential role of stem cell transplantation is increasingly being explored in the management of all types of leukaemia. The conditioning regimen most commonly used is a combination of high-dose cyclophosphamide and total body irradiation. Other conditioning regimens include high-dose melphalan, ludarabine, busulphan or cytarabine. After administration of conditioning therapy, 23 days elapse to allow its elimination from the body, and then previously harvested stem cells are reinfused peripherally. The stem cells will return to and repopulate the marrow, restoring normal haemopoiesis. Throughout this time, patients require intensive supportive care and the procedure, particularly allogeneic stem cell transplantation, causes signiicant morbidity and has a mortality rate of 530% (Rezvani et al.
To work they must get secreted by the S2 segment of the proximal tubule into the urine heart attack grill arizona buy 5 mg enalapril with amex. Hypoalbuminemia results in an increased volume of distribution of diuretics and lesser delivery to the kidneys and is one of many factors related to decreased diuretic responsiveness. These agents are the most powerful diuretic class, causing the excretion of 20% to 25% of filtered sodium load. Bumetanide and torsemide are broken down by the liver and do not accumulate in renal failure. The thiazide group and metolazone are moderately potent diuretics, resulting in the excretion of 5% to 8% of filtered sodium. The "potassium-sparing" drugs are considered mildly potent, causing the excretion of only 2% to 3% of filtered sodium. As a consequence of sequential nephron blockade with diuretics, volume depletion can occur and electrolyte disturbances most commonly hyperkalemia are frequent and must be anticipated with prudent use of the laboratory. Novel strategies employing agents to enable greater gastrointestinal elimination (patiromer calcium, sodium zirconium cyclosilicate) may play a role in the future in the enablement of drugs that antagonize the renin-angiotensin-aldosterone axis. In addition, they face increased risks of readmissions and longer-term mortality, including pump failure and arrhythmic death. Her baseline renal filtration function was moderately impaired and as a result was at risk for inpatient and short-term postdischarge death or rehospitalization. In approximately 25% of patients with acute heart failure, acute kidney injury develops during the hospitalization, and this is termed type 1 cardiorenal syndrome. Neurohormonal activation is a hallmark of type 1 acute cardiorenal syndrome and involves the sympathetic nervous system, renin-angiotensinaldosterone system, arginine vasopressin, endothelin, and many other systems that are maladaptive in the setting of acute heart failure. Type 1 cardiorenal syndrome is associated with increased central venous congestion and has been linked consistently to longer lengths of stay, rehospitalization, and mortality. Sequential nephron blockade of sodium reabsorption can be a strategy to consider in patients who have refractory congestion. Patients have to be very carefully monitored with frequent assessment of electrolytes with this strategy. Confirmation of a heart failure epidemic: findings from the Resource Utilization Among Congestive Heart Failure (R. Etiology and pathophysiology of new-onset heart failure: evaluation by myocardial perfusion imaging. Clinical trials with endothelin receptor antagonists: what went wrong and where can we improve Adenosine receptor expression in the development of renal fibrosis following ischemic injury. Dual A1/A2B receptor blockade improves cardiac and renal outcomes in a rat model of heart failure with preserved ejection fraction. Non-steroidal anti-inflammatory drugs and risk of heart failure exacerbation: a systematic review and meta-analysis. Loop diuretics in acute heart failure: beyond the decongestive relief for the kidney. Acute and chronic cardiovascular effects of hyperkalemia: new insights into prevention and clinical management. At the early stage, decreased systemic vascular resistance results in a mild reduction in mean arterial pressure, which is balanced by increased cardiac output that maintains adequate kidney perfusion. Vasodilation secondary to portal hypertension and systemic inflammation induced by gut bacterial translocation tend to induce renal arterial vasoconstriction because of the activation of vasoconstrictive systems in response to decreased effective blood volume. At the most advanced stages of cirrhosis, renal vasoconstriction can no longer be balanced by increased cardiac output and renal blood flow markedly decreases. Recently, the concept of systemic inflammatory in multiorgan disease has emerged and challenged the vasodilation theory. Even in the absence of overt bacterial infection, cirrhosis is characterized by a state of systemic inflammation, correlated to the severity of liver disease and portal hypertension. In addition, the term hepatorenal disorders was proposed to encompass the full range of conditions in which liver and kidney disease coexist. However, it can be reasonably assumed that patients with advanced cirrhosis frequently have chronic kidney changes resulting from comorbidities. Changes in drug distribution because of volume overload and altered pharmacokinetics resulting from changes in renal and hepatic blood flow and function can affect the concentration and half-life of medications and their metabolites leading to nephrotoxicity. It has been suggested that cirrhosis may not be a predisposing factor for contrast mediainduced nephropathy. Patients with intravascular volume loss because of diarrhea or diuretics should be treated with crystalloids, whereas patients with gastrointestinal bleeding should be given packed red blood cells to maintain a hemoglobin value between 7 and 9 g/ dL. Differentiation between the two entities is not currently possible, because this would require a kidney biopsy. However, all of these tools have limitations, especially in patients with advanced cirrhosis. In candidates for liver transplantation, it has been shown that there is a poor correlation between conventional markers and biopsy findings. Within the kidney, the proximal tubule is located in an area that is especially exposed to hypoxic injury after hypoperfusion. Whatever the cause, hypoxia leads to proximal tubule dysfunction, resulting in an increase in excreted low molecular weight proteins into urine. All of these markers are increased in tubular injury, but none of them is specific of any part of the nephron.
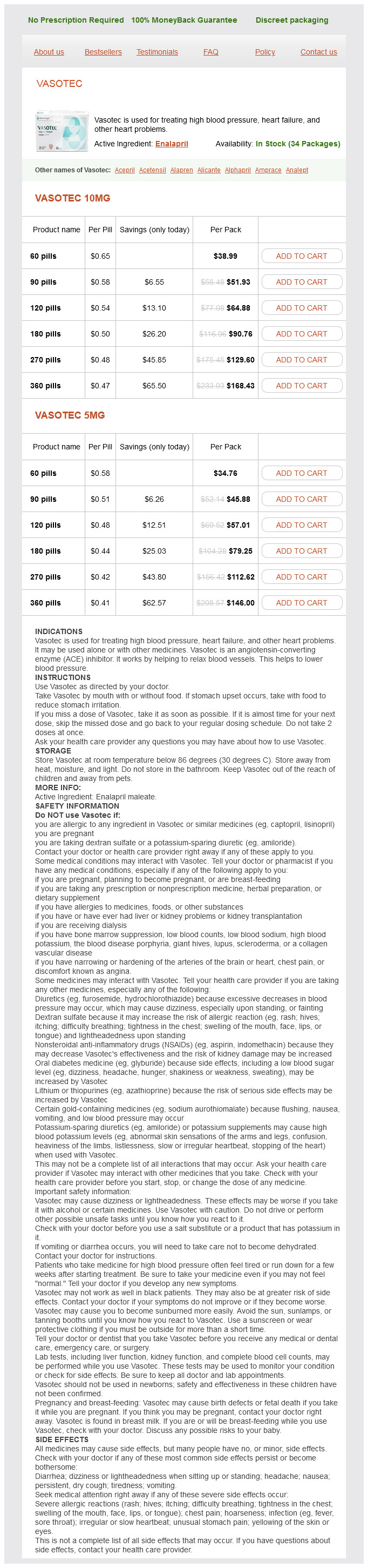
Enalapril Dosage and Price
Vasotec 10mg
- 60 pills - $38.99
- 90 pills - $51.93
- 120 pills - $64.88
- 180 pills - $90.76
- 270 pills - $129.60
- 360 pills - $168.43
Vasotec 5mg
- 60 pills - $34.76
- 90 pills - $45.88
- 120 pills - $57.01
- 180 pills - $79.25
- 270 pills - $112.62
- 360 pills - $146.00
This measurement blood pressure chart 15 year old discount 10 mg enalapril with visa, unfortunately, can be used only to compare efficiency of different treatments in a given moment, not as a tool to establish the effect of treatment on the patient. In all other techniques, serum levels are far from being in steady-state conditions, and similar clearances lead to different mass removal rates. Bradykinin, another potent renal vasodilator, produces large increases in renal and glomerular blood flow mediated through the bradykinin B2 receptor. Other vasodilating factors are insulin-like growth factor, calcitonin gene-related peptide, and cyclic adenosine monophosphate. In these latter cases, exogenous marker clearance may be the solution or at least may represent an important auxiliary tool. The effect on healthcare systems and providers, together with the benefits for the entire population, is clearly evident. However, the serum creatinine value can provide important information about the level of kidney function even when it is not in a steady state. Renal blood flow is kept fairly constant in the presence of significant variations of renal perfusion pressure (line A). When a pathologic event occurs, the mechanism is lost, and even small variations in perfusion pressure result in significant variations of renal blood flow (line B). Significant variations in blood pressure are counterbalanced by changes in the renal vascular tone, and the final result is the maintenance of blood flow within normal ranges. This mechanism enables compensation for changes in plasma flow through a variation in filtration fraction. The combined effect of autoregulation and filtration fraction determines the quantity and composition of the urine. If the patient receives a fluid infusion and extracellular volume expansion therapy, these conditions may be reversible, and the original equilibrium can be restored. In some pathologic conditions, however, or when arterial underfilling remains untreated for longer times, the original alteration, which is functional in nature, may become structural, and parenchymal damage may occur. In such conditions, autoregulation is lost, glomerular hemodynamics and the tubular glomerular feedback are altered, and so is the modulation of filtration fraction. During the evolution of dysfunction, the serum creatinine will underestimate the level of dysfunction. Serum creatinine is measured readily and easily and is reasonably specific for renal function. Critically ill patients may have abnormalities in liver function and markedly decreased muscle mass. In addition, tubular reabsorption ("backleak") may occur in conditions associated with low urine flow rate. Instead, it is important to determine whether renal function is stable or getting worse or better-which can be accomplished usually by monitoring serum creatinine value alone. By contrast, in a patient perfectly matched with the preceding one for age, race, and sex who has a baseline creatinine of 2. Thus it seems that either a different set of criteria is needed in patients with preexisting disease or some absolute creatinine criteria must be integrated into the classification system. At rest, organ systems operate at baseline capacity, and this capacity can be increased to a certain maximum capacity. However, when a healthy person exercises, the cardiac output can double or even triple. The ability to test the reserve of an organ system is often an excellent diagnostic tool to uncover subclinical disease. Similarly, stress testing of the kidney appears to generate insights into the presence or absence of kidney disease and parenchymal loss resulting from injury and potentially fibrosis. However, when the kidney is diseased or injured, the glomerular and tubular function may be affected equally, or its form and functional capacity may Chapter 9 / Glomerular Filtration Rate, Renal Functional Reserve, and Kidney Stress Testing diverge. An assessment of glomerular and tubular function may be more informative than just one of these domains. Glomerular reserve testing has been well established but is used infrequently in routine clinical care. Tubular function diagnostic testing is relatively new and in its clinical "infancy. Primary hyperfiltration in kidney disease has been shown in patients with diabetes mellitus, polycystic kidney disease, secondary focal segmental glomerulosclerosis, sickle cell anemia, high altitude renal syndrome, and obesity, hypertension, nephrotic syndromes, and glomerulonephritis. Our own group has pointed out the methodology to perform a complete renal reserve stress test. This observation seems to support the hypothesis that an overall increase in blood flow is the main mechanism rather than a temporary hemodynamic perturbation in the afferent/efferent tone and equilibrium. It is important to recognize that the loss of renal reserve also may manifest as a loss in autoregulation capacity in the kidney. The idea of assessing renal reserve has been present for decades but is used infrequently in clinical practice, whereas the cardiac stress test is used routinely. In our view, the simple reason is that cardiologists perceive that they can intervene in patients with diminished cardiac reserve. Chief among those chores include the handling of electrolytes, water, and amino acids; catabolism of various proteins; and the active secretion of endogenous and exogenous acids. Tubular function assessment may be more informative than glomerular reserve in patients who already have advanced kidney disease. However, once a patient has kidney injury/disease, glomerular reserve already is reduced substantially and therefore is less informative.
© 2025 Adrive Pharma, All Rights Reserved..