General Information about Dutas
Dutas is usually well tolerated and might provide vital aid for males suffering from BPH. It is important to note that it's not a cure for the situation, however somewhat, it helps to manage its symptoms. In some cases, males might need to proceed taking Dutas long-term to maintain its results.
Benign prostatic hyperplasia (BPH), also referred to as an enlarged prostate, is a standard condition that affects tens of millions of men around the world. It occurs when the prostate gland, which is liable for producing fluid that nourishes and protects sperm, becomes enlarged and begins to press against the urethra. This can result in uncomfortable symptoms such as issue urinating, frequent urination, and a weak urine stream.
In rare instances, Dutas can also increase the danger of high-grade prostate cancer. It is necessary for men taking this medication to have regular check-ups with their doctor to watch for any potential issues.
In conclusion, Dutas is an efficient treatment for managing the signs of BPH. It works by inhibiting the conversion of testosterone to DHT, a hormone involved in the growth of an enlarged prostate. While it could have some potential side effects, the benefits of Dutas far outweigh the risks for many men. If you are experiencing signs of BPH, consult along with your doctor to see if Dutas could additionally be an appropriate therapy possibility for you. Remember to at all times follow your doctor’s instructions and report any unwanted aspect effects you expertise. With proper remedy, BPH could be managed and men can go back to living their lives with out the discomfort and inconvenience of an enlarged prostate.
Dutas is available in capsule type and is usually taken as quickly as a day. It can take a quantity of weeks earlier than the total results of the medication are seen, and it is very important continue taking it as prescribed for finest results. In addition to treating BPH, Dutas may also be prescribed to deal with male sample baldness, as DHT can additionally be responsible for hair loss in men.
DHT is a hormone that's concerned in the development of BPH. It is a stronger and stronger form of testosterone, and can trigger the prostate gland to develop larger and press towards the urethra. By inhibiting the conversion of testosterone to DHT, Dutas helps to forestall the growth of the prostate and alleviate the symptoms of BPH.
As with any treatment, there are potential unwanted side effects associated with Dutas. The most common unwanted aspect effects embrace decreased libido, erectile dysfunction, and decreased ejaculate quantity. These side effects are sometimes delicate and may go away with continued use. However, if they persist or turn into bothersome, it is essential to converse with a doctor.
Fortunately, there are remedies obtainable for BPH, certainly one of which is a drugs known as Dutas. Dutas, also recognized by its generic name dutasteride, is a sort of treatment often known as a 5-alpha-reductase inhibitor. It works by blocking the conversion of testosterone to dihydrotestosterone (DHT) within the physique.
The diagnosis may be readily apparent in the setting of hemophilia hair loss causes in women cheap dutas 0.5 mg buy, but in other circumstances it is less clear. Streaks of blood, as opposed to the uniformly bloody fluid of a hemarthrosis, may be seen in the synovial fluid during routine arthrocentesis because of needle trauma to skin or other periarticular structures. Blood that appears in the synovial fluid at the end of an arthrocentesis is also because of trauma, particularly if the initial synovial fluid was not bloody. During an arthrocentesis, if frankly bloody fluid is seen initially on entering the joint, hemarthrosis must be suspected. If the original arthrocentesis was traumatic, synovial fluid obtained from the new site should become clear or be only bloodtinged. A hematocrit similar to peripheral blood is more likely from a traumatic arthrocentesis, whereas fluid from a hemarthrosis has a hematocrit less than peripheral blood. A major concern with hemarthrosis is long-term joint damage owing to inflammation resulting from recurrent bleeding. As such, accurately identifying hemarthrosis and instituting appropriate treatment can reduce long-term joint-related disability. What finding in the bloody synovial fluid may indicate a fracture has caused the hemarthrosis? A fracture may release blood and bone marrow elements including lipids into the synovial fluid. These fat globules may be seen floating at the top of the synovial fluid by bedside visualization of the fluid in the syringe or collection tube. If there are fat globules present in the synovial fluid identified by oil red O staining, a fracture should be suspected. Is it safe to perform arthrocentesis when a patient has a prolonged prothrombin time from warfarin therapy? If a patient on warfarin develops an acute monoarthritis, diagnostic aspiration is warranted, even if the prothrombin time is excessively prolonged. In addition, some authorities report that reversal of anticoagulation is not necessary if the proper technique is carefully observed and an appropriately small gauge needle is used. Caution should be observed, particularly in large joints where it is difficult to apply direct pressure, such as the shoulder or knee. There are no specific published guidelines for reversal of anticoagulation before arthrocentesis; however, fresh frozen plasma or small doses of vitamin K (0. Vitamin K should never be given subcutaneously as it may cause prolonged reversal of anticoagulation from warfarin. A mild compression bandage and ice may be applied and analgesia provided with acetaminophen or narcotics. Symptoms usually spontaneously subside if the prothrombin time is reduced from supratherapeutic to simply therapeutic. Occasionally, an intraarticular injection of corticosteroids such as triamcinolone hexacetonide will be needed to control symptoms. Destructive arthritis from a single episode of hemarthrosis is rare; however, chronic joint destruction resulting from recurrent bleeding from warfarin therapy has been reported. As the joint capsule distends, severe pain follows with swelling from effusion and decreased range of motion. The swelling will eventually tamponade the bleeding and the hemarthrosis will gradually resolve over a matter of days to weeks. Almost all patients with severe hemophilia (<1% of normal factor activity) and half of patients with moderate disease (1% to 5% factor activity) will have recurrent hemarthroses spontaneously or following minor trauma. If factor levels are >5% of normal, hemarthroses tend to be less frequent or occur following more significant trauma. Hemarthroses first begin to occur in weight-bearing joints when a child is just learning to walk. The mainstay of therapy for acute hemarthrosis in hemophilia is rapid replacement of deficient factor to achieve a level of 30%. In appropriate patients, factor replacement therapy can be promptly instituted by the family at the first symptoms of hemarthrosis to decrease the risks of sequelae. Patient education and involvement are critical for the success of any treatment program. Other initial treatment consists of placing the joint at rest in as much extension as can be tolerated (to prevent contractures), with applications of ice packs and other local measures. Once acute bleeding and pain are controlled, graded physical therapy to prevent muscle atrophy and contractures should be instituted. When should septic arthritis be suspected if a hemophiliac develops acute monoarthritis? The presence of fever and/or if the pain of a suspected hemarthrosis fails to improve after factor replacement, concomitant septic arthritis must be suspected and aspiration of the joint becomes mandatory. Any synovial fluid obtained on routine aspiration of a hemarthrosis should be submitted for Gram stain and culture. Staphylococcus aureus and Streptococcus pneumoniae are most common organisms identified (Box 49-2). Do recurrent hemarthroses have any long-term consequences in patients with hemophilia? As the patient approaches adulthood, acute hemarthroses become less frequent but chronic joint symptoms supervene. Recurrent hemarthroses lead to accumulation of hemosiderin in the joint lining tissues. The end result is a chronically swollen joint, less painful than seen in acute hemarthroses, with decreased range of motion. Surrounding muscles become atrophic and joint contracture is a frequent complication.
The resultant antibodyÂantigen interaction leads to fixation of complement and initiation of the inflammatory process hair loss yahoo article order discount dutas on line, causing glomerulonephritis and alveolar hemorrhage. Immunofluorescence staining with Ig antibodies reveals linear deposition of Ig in the glomerular basement membranes. Immunofluorescence studies reveal granular (lumpy) deposition of Ig, characteristic of immune complex deposition, within the glomerulus. Thus, immunofluorescence studies are usually negative or reveal only scant Ig deposition, usually in areas of necrosis. The spectrum of clinical presentation may range from relatively mild disease limited to the upper respiratory tract to fulminant life-threatening involvement of the upper and lower respiratory tract, kidneys, and other end organs. The disease progression is also variable and protean, including protracted mild disease remaining in the upper respiratory tract despite absence of treatment, widespread but relatively mild and slowly progressive disease, and rapidly progressive pulmonary and renal disease manifesting as alveolar hemorrhage syndrome and rapidly progressive renal failure on presentation. A further caveat is the observation that relatively mild and limited disease may rapidly progress to more diffuse and active disease at any time during the course in at least 10% of cases. Death may result from respiratory failure, renal failure, infection, other end-organ involvement, or as a complication of treatment. Titrate to effect while keeping the total white blood cell count >3500 /L and the absolute neutrophil count >1000 to 1500 /L to lessen the risk of infection. Patients with subglottic stenosis can also be treated with bronchoscopy, intralesional steroid injections with or without topical mitomycin C, followed by dilation of the airway. Several medications frequently used in combination with low-dose prednisone to maintain remission include azathioprine, methotrexate, mycophenolate mofetil, and leflunomide. Patients who have been in complete remission for 12 to 18 months on standard maintenance therapy have a 50% risk of relapse once that therapy is stopped. A recent study suggests that maintenance therapy for more than 36 months is associated with less chance of relapse. Patients allergic to sulfa drugs can receive dapsone, atovaquone, or inhaled pentamidine. Apply 2% mupurican ointment with a cotton bud inserted half way into the nasal vestibule between irrigations to diminish carriage of S. Rates of malignancy (skin and bladder cancers and acute myeloid leukemia) are increased, particularly in patients receiving a total dose of >36 g. The risk of ovarian failure is up to 50% in patients >20 years of age who receive a total dose of >20 g, those >30 years who receive a total dose of >10 g, and those >40 years who receive a total dose of 5 g. Patients typically present with acute onset of rapidly progressive glomerulonephritis (100%) and up to 50% have pulmonary infiltrates and/or effusions. The renal pathology is a focal, segmental necrotizing glomerulonephritis, frequently with crescents. Plasmapharesis and intravenous gammaglobulins have been used in a few patients with progressive renal failure or pulmonary hemorrhage. The phases may appear simultaneously and do not have to follow one another in the order presented here. It consists of allergic manifestations of rhinitis, polyposis, and most commonly asthma (80% to 90%). Peripheral blood and tissue eosinophilia develop, frequently causing a picture resembling Lцffler syndrome (shifting pulmonary infiltrates and eosinophilia), chronic eosinophilic pneumonia, or eosinophilic gastroenteritis. Life-threatening systemic vasculitis occurs on average 3 years after the onset of the prodromal phase. Patients can develop myocarditis, valvular insufficiency, neurologic symptoms (most commonly vasculitic peripheral neuropathy), eosinophilic gastroenteritis, purpura, and testicular pain. There is no direct correlation between the degree of eosinophilia and disease activity. The diagnosis should be suspected in a patient with a previous history of allergy or asthma who presents with eosinophilia (>1500 cells/L) and systemic vasculitis involving two or more organs. They are highly specific and composed of a central eosinophilic core surrounded radially by macrophages and giant cells (in contrast to granulomas with a basophilic core seen in other diseases). Inflammatory cells are also present: eosinophils predominate, with smaller numbers of neutrophils and lymphocytes. Those with severe presentations may benefit from 3 days of pulsed methylprednisolone (1 g/day) with or without plasmapharesis. The major cause of death is cardiac involvement with myocardial infarction and congestive heart failure. Serious end-organ manifestations, including necrotizing glomerulonephritis and alveolar hemorrhage, occur less frequently. It is notable that patients with cystic fibrosis frequently have gram-negative infections of their airways. Cohen P, Pagnoux C, Mahr A, et al: ChurgÂStrauss syndrome with poor-prognosis factors: a prospective multicenter trial comparing glucocorticoids and six or twelve cyclophosphamide pulses in forty-eight patients, Arthritis Rheum 57:686Â693, 2007. Comarmond C, Pagnoux C, Khellaf M, et al: Eosinophilic granulomatosis with polyangiitis (ChurgÂStrauss): clinical characteristics and long-term followup of the 383 patients enrolled in the French Vasculitis Study Group cohort, Arthritis Rheum 65:270Â281, 2013. Martinez V, Cohen P, Pagnoux C, et al: Intravenous immunoglobulin for relapses of systemic vasculitides associated with antineutrophil cytoplasmic autoantibodies: results of a multicenter, prospective, open-label study of twenty-two patients, Arthritis Rheum 58:308Â317, 2008. Mukhtyar C, Hellmich B, Bacon P, et al: Outcomes from studies of antineutrophil cytoplasm antibody associated vasculitis: a systematic review by the European League Against Rheumatism systemic vasculitis task force, Ann Rheum Dis 67:1004Â1010, 2008. Ribi C, Cohen P, Pagnoux C, et al: Treatment of ChurgÂStrauss syndrome without poor-prognosis factors: a multicenter, prospective, randomized, open-label study of seventy-two patients, Arthritis Rheum 58:586Â594, 2008. Urticarial lesions lasting longer than 24 to 48 hours and resolving with hyperpigmentation are likely vasculitic. Obstructive pulmonary disease commonly occurs in patients with hypocomplementemic urticarial vasculitis syndrome. Small-vessel vasculitis includes a variety of conditions that are grouped together because of the involvement of small blood vessels (<50 m in diameter) of the skin, especially arterioles and postcapillary venules.
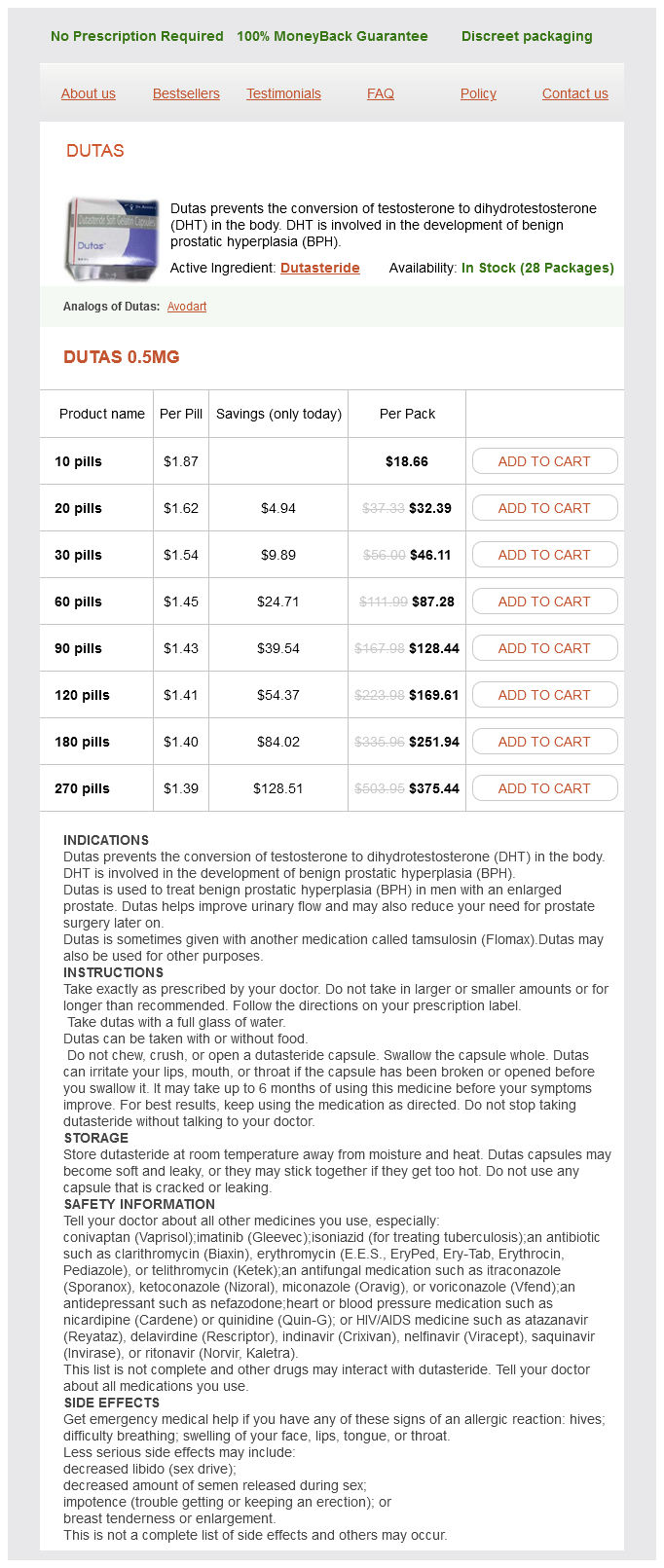
Dutas Dosage and Price
Dutas 0.5mg
- 10 pills - $18.66
- 20 pills - $32.39
- 30 pills - $46.11
- 60 pills - $87.28
- 90 pills - $128.44
- 120 pills - $169.61
- 180 pills - $251.94
- 270 pills - $375.44
Electron microscopy shows immune complex deposits in both subendothelial and subepithelial distributions hair loss cure ayurvedic buy dutas 0.5 mg otc, although subepithelial lesions should involve less than 50% of glomeruli. The pathology report should also describe the activity and chronicity of the lesion. Clinically, patients almost always have proteinuria (frequently nephrotic), cellular casts, and hematuria and, not infrequently, decreased renal function. Membranous lupus nephritis (class V) is characterized by the presence of granular global or segmental subepithelial immune deposits seen by immunofluorescence or electron microscopy. Clinically, patients who have pure membranous disease frequently have extensive proteinuria but only minimal hematuria or renal functional abnormalities. Membranous disease can also be observed as a transition stage after treatment for proliferative glomerulonephritis. What is the importance of evaluating biopsies for the extent of activity or chronicity? Historically on a renal biopsy report, pathologists would provide a calculated score to represent disease activity and disease chronicity. However, more recent literature shows mixed predictive value of using such a score and these calculations are no longer universally used. However, the identification of histological changes that represent chronicity and activity are thought to be helpful in contributing to the overall description of the renal biopsy. Evidence of fibrosis indicates chronic scarring disease, which may be less likely to respond to therapy Table 16-5). Which serological tests are most useful when following a patient with lupus nephritis? In addition, patients with active lupus nephritis have decreased levels of complement components. Thus, two alternative theories have been proposed to explain the pathogenic mechanisms of these antibodies. The activation of complement components through the classical pathway, with amplification by the alternative pathway, appears to be involved in the pathogenesis of glomerular damage. Complement activation may cause direct damage as well as recruit inflammatory cells to the sites of immune complexes. Which patients with severe lupus nephritis are more likely to progress to end-stage renal disease? Other features, which have been suggested, include lower socioeconomic status, poor compliance with medications, and comorbidities such as hypertension and diabetes. Failure to normalize the serum creatinine and decrease proteinuria to <1 g/day within 6 months of starting therapy is associated with a poorer long-term renal prognosis. Patients who fail to respond to both are candidates for rituximab or calcineurin inhibitors (cyclosporin, tacrolimus). Previously, cyclophosphamide was given as a daily oral dose or a prolonged (18 to 24 months) course of intravenous dosing. There is also accumulating data that low-dose cyclophosphamide followed by maintenance therapy is equivalent in efficacy to higher-dose regimens. Low-dose therapy ("Euro-Lupus" protocol) is associated with fewer serious infections and less infertility but has mostly been studied in white Europeans. Note that the risk of premature ovarian failure correlates with the cumulative dose of cyclophosphamide and the age of the patient. If creatinine clearance is less than 35 to 40 mL/min, then start the initial dose at 0. Which cytotoxic agents are most frequently used for maintenance therapy in treatment of lupus nephritis? Each of these drugs are given in association with a dose of prednisone required to control extrarenal manifestations, and prednisone is tapered over time. Calcineurin inhibitors (cyclosporin, tacrolimus) have also been used for maintenance therapy and in patients with refractory disease. A 30-year-old woman with severe nephritis and end-stage renal failure is referred for further evaluation and treatment. The patient, who has been on dialysis for nearly 5 years, is being considered for transplantation but is afraid that her lupus will destroy the donor kidney. Lupus nephritis accounts for up to 1% to 2% of cases of end-stage renal failure requiring dialysis or transplantation. There is some evidence that transplantation before initiation of dialysis may result in improved allograft and patient survival. Furthermore, even in patients with recurrent nephritis, it is unlikely to lead to allograft loss. Retrospective analysis has reported that lupus patients have a similar incidence of graft survival rates as compared with nonlupus patients; however, the presence of antiphospholipid antibodies may decrease the rate of allograft survival. Manifestations of diffuse disease include intractable headaches, generalized seizures, aseptic meningitis, acute confusional state, cognitive dysfunction, psychiatric disease (especially psychosis and severe depression), and coma. Manifestations of focal disease include stroke syndromes such as hemiparesis, focal seizures, movement disorders such as chorea, and transverse myelitis. These autoantibodies are hypothesized to affect neuronal function in a generalized manner. Patients with acute encephalopathy frequently demonstrate elevated levels of antineuronal antibodies or other evidence of autoantibody production in the cerebrospinal fluid.
© 2025 Adrive Pharma, All Rights Reserved..