General Information about Divalproex
Like any treatment, Depakote may cause side effects, but not everybody experiences them. Common side effects might include dizziness, drowsiness, nausea, vomiting, and diarrhea. More critical unwanted aspect effects, although uncommon, can include liver problems and low platelet count, which can result in easy bruising or bleeding. It is essential to report any new or persistent unwanted effects to the doctor for correct management.
Epilepsy is a neurological disorder that impacts approximately three.four million individuals in the United States alone. It is characterised by recurring seizures, which are sudden, uncontrolled electrical disturbances in the mind. These seizures can vary in kind and severity, from delicate to extreme, and might have a big impression on a person’s every day life. They can even have critical consequences, corresponding to falls, accidents, and even demise.
There are numerous types of epilepsy, and Depakote has shown to be effective in treating various varieties of seizures. It is usually prescribed for generalized tonic-clonic seizures, that are characterized by lack of consciousness, stiffening of muscular tissues, and jerking movements. This kind of seizure may be very intense and can lead to severe accidents. Depakote helps to scale back the frequency and intensity of those seizures, thereby enhancing the quality of life for folks with epilepsy.
In conclusion, Depakote (divalproex) is a extensively prescribed medication for the therapy of epilepsy, particularly for generalized tonic-clonic, absence, and partial seizures. It has additionally confirmed to be effective in managing bipolar dysfunction. However, like all medicine, it must be taken as prescribed and under the supervision of a healthcare professional. With proper use, it can significantly enhance the standard of life for folks residing with seizures.
Apart from treating epilepsy, Depakote can be prescribed for the treatment of bipolar disorder. Bipolar disorder is a continual mental health situation that is characterized by extreme temper swings, ranging from manic episodes of excessive power to depressive episodes of low temper. Depakote works by stabilizing the mood swings, making it a valuable therapy choice for this situation.
This medication is also used to treat absence seizures, which contain a short loss of consciousness with minimal movements. It has been proven to be efficient in as much as 80% of individuals with absence seizures, considerably lowering the variety of episodes. Depakote can also be used for partial seizures, which contain one part of the brain and may cause unusual sensations, movements or behaviors. It can be used alone or together with other medicines to handle most of these seizures.
Divalproex is a medicine that falls underneath the class of anticonvulsants, also referred to as anti-epileptic drugs. It is mostly recognized by its model name Depakote, and is extensively prescribed for the therapy of assorted types of seizure problems. Divalproex has been accredited by the United States Food and Drug Administration (FDA) since 1983, and continues for use as an effective remedy option for folks with epilepsy.
Depakote is available in various types, together with tablets, delayed-release tablets, extended-release tablets, and sprinkle capsules. The dose prescribed might range relying on the kind of epilepsy, the severity of seizures, and the individual’s age and weight. It is important to comply with the dosage suggestions offered by the doctor and to not change the dose without consulting them.
Depakote works by rising the degrees of a chemical referred to as gamma-aminobutyric acid (GABA) in the mind. GABA is a neurotransmitter that helps to relax the overexcited nerve cells in the mind, thus reducing the likelihood of seizures. This medicine also works by lowering the activity of glutamate, one other neurotransmitter that's answerable for stimulating nerve cells. These combined actions of Depakote assist to stabilize the electrical exercise in the mind and forestall seizures.
Nodules show a great range in size but are most commonly in the 110 mm range treatment 1st degree heart block cheap generic divalproex uk, smooth, well defined and sometimes with a centrilobular or peribronchovascular distribution. With therapy, clinical and radiographic signs clear in weeks in 3060% of patients, but there is a substantial relapse rate (50% in two recent studies)185,186 and up to one-third of patients are left with persistent radiographic abnormality. Secondary organizing pneumonia Organizing pneumonia is commonly associated with a recognized precipitating cause and in the Mayo Clinic series of 74 patients, 36% were classified as secondary, compared with 50% cryptogenic cases. They usually respond well to steroids, though with a high prevalence of relapse on withdrawal of steroids. Four patients had symptoms suggestive of an antecedent respiratory infection, and a further three had infection identified at biopsy. Overall 94% of lesions had irregular margins and about 50% of lesions had air bronchograms, satellites, or pleural tags. In the acute exudative phase, there is diffuse alveolar interstitial thickening due to edema, and associated hyaline membranes. Males and females are equally affected, with a wide age range (1383 years); mean ages also vary widely in various series from 28 to 65 years. The chest radiograph shows diffuse consolidation, sometimes with a zonal predominance and often with air bronchograms. In 3070% of patients, septal thickening is found in areas of ground-glass opacity, perhaps corresponding to alveolar collapse adjacent to septa. Honeycombing is seen in 1226% of cases, and should lead to suspicion of background fibrosing interstitial pneumonia. The presence of traction bronchiectasis suggests that the disease is in the organizing phase, while honeycombing is seen in the fibrotic phase. It is thought to represent a reactive lymphoid hyperplasia; evolution to frank lymphoproliferative disease is now thought not to occur. Dyspnea and a nonproductive cough are common and may be present for months to years. On examination inspiratory dry crackles are common, while clubbing occasionally occurs. On physiology, a restrictive ventilatory defect, with preserved airflow, is found. Subpleural nodules, bronchovascular thickening, and septal thickening were also common, seen in 19 of 22 patients. Mediastinal or hilar lymphadenopathy was seen in 15 patients, particularly in those with intrathoracic Castleman syndrome. The cysts appear to represent dilated small bronchi and bronchioles caused by lymphocytic infiltration and partial obstruction. Among siblings in this cohort, cigarette smoking was associated with an odds ratio of 3. All patients imaged beyond infancy developed fine or coarse peripheral interstitial septal thickening. Hilar and mediastinal lymphadenopathy, consolidation, atelectasis, pleural thickening and air-trapping were also seen. In two affected neonates, the features were characterized by groundglass and reticular abnormality with interlobular septal thickening. Affected individuals may present with neonatal respiratory distress, or may present in childhood or adulthood with gradual onset of dyspnea. In particular, the finding of centrilobular nodules or tree-in-bud pattern was very suggestive of infection. The presence of septal thickening or pleural effusion as predominant findings should suggest acute eosinophilic pneumonia (see Chapter 11, p 660). Interdisciplinary approach to diagnosis There is moderate interobserver variation among radiologists and pathologists in characterization of diffuse lung disease. In a study of 131 patients evaluated by 11 thoracic radiologists, agreement on the first choice diagnosis was moderate (kappa 0. Histopathologic information had the greatest impact on the final consensus diagnosis, but presentation of clinical and imaging information resulted in alteration of pathologic diagnosis in 11 of 58 patients. The pulmonary function indices that reflect these abnormalities are routinely used in clinical practice to make an assessment of the extent of disease and monitor progress. However, the differential diagnosis must include infectious pneumonia, acute hyper- 583 Chapter 10 · Idiopathic Interstitial Pneumonias and Immunologic Diseases of the Lungs tests are limited by inability to account for the regional inhomogeneity of fibrosing lung disease. However, the severity of physiologic impairment,66 and the change in physiologic parameters over a 1-year interval, are good predictors of long-term survival. It has recently been hypothesized303 that these previously described cases of unexplained upper lobe fibrosis represented idiopathic pleuroparenchymal fibroelastosis,304 a rare condition characterized histologically by marked thickening of the apical visceral pleura and prominent subpleural fibrosis, with a mixture of elastic tissue and dense collagen. One of the individuals in this series experienced a spontaneous pneumothorax, followed by a postsurgical bronchopleural fistula which ultimately led to death. Individuals with this condition may be at risk for prolonged spontaneous or iatrogenic pneumothorax. The autoimmune-mediated inflammation and fibrosis that characterize these diseases in other organs can irreversibly disrupt the normal functioning of the lung. Many of these diseases are characterized by the presence of a specific type of autoantibody, which may greatly assist specific diagnosis (Table 10. The underlying mechanisms that account for the tissue changes encountered in this group of illnesses are unknown. As a group they can affect each portion of the lung, the pleura, alveoli, interstitium, vasculature, lymphatic tissue, and airways both large and small (Table 10. It is about three times more common in females than males and usually has an insidious onset, pursuing a variable course with relapses and remissions.
Surgical thromboendarterectomy may be undertaken in carefully selected patients with substantial success treatment 3rd nerve palsy buy 250 mg divalproex overnight delivery. The thrombi in the smaller vessels show recanalization, forming a lattice of fibrous trabeculae lined by endothelium. New blood channels may form within the thrombi, and medial hypertrophy occurs secondarily. Plexiform lesions (see description in the section on Pulmonary arterial hypertension idiopathic and associated disorders, p. Others show only changes such as atelectasis, pleural thickening, or pleural effusion, with no radiographic signs of pulmonary hypertension. Unsurprisingly, pleural changes are more frequent in patients with thromboembolic pulmonary hyper- Box 7. Note the more prominent vessels in the denser (relatively overperfused) regions of the lung. The subpleural irregularity posteriorly in the right upper lobe probably reflects a previous pulmonary infarct. The intervening normal lung may appear abnormally dense, because of relatively increased perfusion, and these areas may be misinterpreted as having an abnormal ground-glass pattern due to another cause. Pulmonary angiography433 reveals filling defects caused by thrombi in the lobar or segmental arteries, with occlusions of large- and medium-sized vessels. If the thrombus in the main pulmonary arteries is laminated, the typical angiographic signs of filling defects may be absent. Mostly these conditions affect the small vessels, and these are discussed in Chapter 10. Vasculitis confined to the large vessels and causing pulmonary hypertension is recognized but is much less common;451 Takayasu disease is the best known example. Takayasu arteritis (Takayasu disease, occlusive thromboarteriopathy, pulseless disease) is an arteritis of medium and large arteries that most commonly affects segments of the aorta and its main branches. Takayasu arteritis occurs chiefly in Asian women, and is manifested between 10 and 20 years of age in 75% of patients. Adjacent sections showed an aneurysmal pouch arising from the anterior aspect of the main pulmonary artery. B, Mosaic perfusion pattern in the upper lobes, presumed to reflect arteritic involvement and/or thrombosis of the medium-sized and smaller pulmonary vessels. Involvement of pulmonary arteries occurs in approximately half the patients455,456 and there appears to be a correlation between the frequency of pulmonary and systemic artery lesions. The thickened walls of involved vessels sometimes show early or delayed enhancement following contrast enhancement. Posttraumatic false aneurysm471 (reported as a complication of SwanGanz catheter placement),472,473 dissecting aneurysm of a pulmonary artery,474 postembolic aneurysm,475 bronchial carcinoma,476 and myxomatous emboli from a right atrial myxoma477 are all very rare causes of pulmonary artery aneurysm. In one autopsy series,480 rupture of the aneurysm was the immediate cause of death in 38 of the 45 tuberculosis patients examined. It is rare to see the aneurysm as a discrete mass in an otherwise normal lung (Behçet disease being an exception). Usually the aneurysm is adjacent to , or surrounded by, the infective consolidation that caused it, and it may therefore be very difficult to appreciate. In terms of rarity, idiopathic pulmonary artery aneurysms are limited to single case reports. Mycotic aneurysms may also occur in association with lung abscess or septicemia, particularly in Box 7. An additional complication in some patients with chronic liver disease is portopulmonary hypertension, which is characterized by increased intrapulmonary vascular resistance;486 whereas some regard this entity as being entirely separate from hepatopulmonary syndrome,487 others suggest a linkage. The pathophysiology behind the hypoxemia is complex and cannot entirely be ascribed to right-to-left shunting through the abnormal vessels. Krowka and colleagues491,492 have classified the vascular lesions of the hepatopulmonary syndrome as: · · type 1 (minimal) the commoner type with a spidery appearance of the peripheral vessels on angiography and some response (decreased shunting) to 100% oxygen type 2 (accounting for approximately 15% of cases) essentially small, but macroscopic, arteriovenous fistulas that do not respond to supplementary inspired oxygen. Another survey revealed a similar incidence of pulmonary infections but a much lower proportion of bacterial pneumonia and relatively few cases of pneumococcal pneumonia. In both of these series the precise cause of more than half the episodes could not be determined, and they were presumed to result from pulmonary infarction or missed infection. In one more recent study, no identifiable cause for the acute chest syndrome was discovered in 87% of patients (median age 14 years). Autopsy series, which clearly represent the severe end of the spectrum of pulmonary disease, show a high prevalence of pulmonary infarcts, even in infants and young children. Distinguishing consolidation resulting from infection from that caused by infarction is often impossible. One clue to the diagnosis of infarction may be the late development of a pulmonary shadow; consolidation resulting from pneumonia is likely to be present on the initial film. If the shadowing is clearly interstitial in character and the patient has fever, viral or mycoplasmal pneumonia are considerations. Radionuclide lung scintigraphy shows extensive extrapulmonary uptake caused by the bypassing of the pulmonary arteriolar bed,494 and scintigraphic shunt calculations have shown that more than half of the pulmonary blood flow may bypass the alveoli. Some of these abnormally dilated peripheral vessels can be seen to abut the pleural surface. Typical features of hepatopulmonary syndrome: a, marked dilatation of the segmental pulmonary arteries in the lower lobes and slightly increased nodularity in the subpleural lung posteriorly; B, obvious enlargement of the extremely peripheral pulmonary vessels nestling in the costophrenic recess. The edema may be the result of treatment with analgesics such as morphine or may be the consequence of heart failure. Several hemodynamic factors are at work, and the relative role of each may be difficult to unravel in an individual case. Chronic anemia of any cause gives rise to a sustained increase in cardiac output even when the patient is at rest. In addition, there may be areas of ground-glass opacification;500 in the study by Bhalla et al.
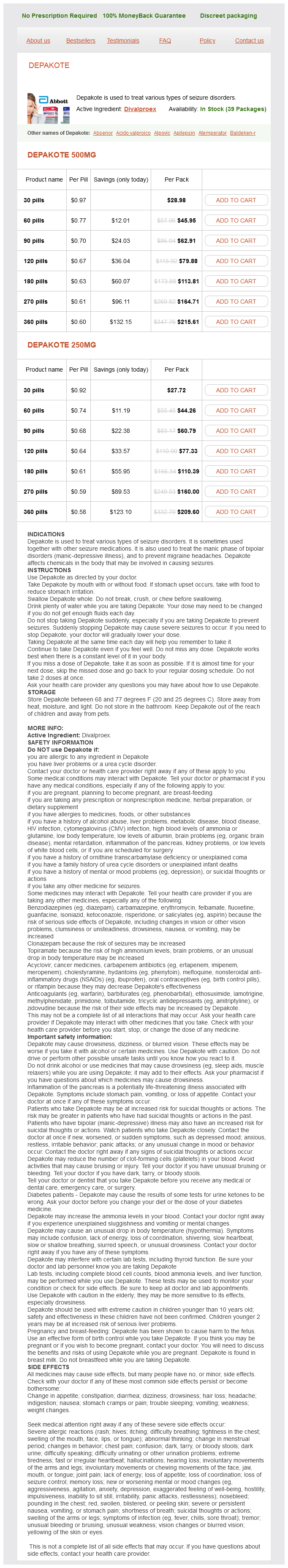
Divalproex Dosage and Price
Depakote 500mg
- 30 pills - $28.98
- 60 pills - $45.95
- 90 pills - $62.91
- 120 pills - $79.88
- 180 pills - $113.81
- 270 pills - $164.71
- 360 pills - $215.61
Depakote 250mg
- 30 pills - $27.72
- 60 pills - $44.26
- 90 pills - $60.79
- 120 pills - $77.33
- 180 pills - $110.39
- 270 pills - $160.00
- 360 pills - $209.60
Application of microwave technology to faster analysis of proteins/peptides is an emerging field that is gaining more attention symptoms 9 dpo divalproex 250 mg buy online. One of initial studies was microwave-assisted Akabori reaction for peptide analysis [100]. The classical Akabori reaction [101], devised in 1952 for the identification of C-terminus amino acids, involved the heating of a linear peptide in the presence of anhydrous hydrazine in a sealed tube for several hours. The C-terminus group is liberated as free amino acid and can be distinguished from the remaining amino acid residues that have been converted to hydrazides. To monitor the hydrazinolysis progress, dimethyl sulfoxide was added to dilute the reaction mixture that allowed aliquots of the reaction mixture to be drawn every few minutes over a period of about an hour. The initial Akabori cleavage, involving the loss of C-terminal tyrosine from the modified heptapeptide (m/z 838), led to the formation of the hexapeptide hydrazide at m/z 689. In all three fragment ions, the same C-terminal amino acid (tyrosine) was lost with different N-terminal sequence. Clearly, microwave-assisted Akabori reaction can lead to rapid identification of C-terminus amino acid in a polypeptide including its amino acid sequence information at both Cterminus and the N-terminus. Microwave-assisted Akabori reaction was extended to cyclic oligopeptides for the rapid determination of the sequence of amino acids [102]. The traditional Edman degradation is not particular attractive to sequencing of cyclic peptides since selective hydrolysis of peptide bonds by this method is not easy to achieve because of the lack of free N-terminus. The other approach using tandem mass spectrometry also proves to be difficult because the indiscriminate ring-opening pathways often gives a set of acylium ions of the same massto-charge ratio [103, 104]. In the case of glycine-containing cyclic peptides, microwave-assisted hydrazinolysis led to selective ring-opening at glycine residue to generate the corresponding open chain hydrazide(s) in a few minutes. For example, a nonapeptide, cyclo (-Phe-His-Trp-Ala-Val-Gly-His-Leu-Leu-), treated with 98% hydrazine under microwave irradiation for a few minutes, generated a linear oligopeptide hydrazide (m/z 1093). Since there was no arginine, aspargine, cysteine, and other amino acids that react with hydrazine under microwave irradiation, no additional peaks resulted from modifications appeared in the mass spectrum. A number of other non-glycine-containing cyclic peptides were also investigated under microwave irradiation [105]. Those cyclopeptides were all opened to form linear hydrazides in about 1020 minutes. Another application area in microwave technology is the use of microwave irradiation for the enzymatic digestion of proteins [106]. As discussed in the early part of this chapter, enzymatic cleavage to produce smaller peptide fragments of protein samples is an important step in structural characterization of proteins [24]. Traditional enzymatic digestion method usually takes several hours, whereas microwave-assisted digestion occurs in minutes. The peaks marked with an asterisk represent bn-H2O ions, whereas the peaks marked with a black square represent the internal fragment ions. The protein was treated with trypsin at a 1: 25 protease-to-protein ratio and the solution was subjected to microwave irradiation for about 10 minutes. The result was similar to what was obtained using traditional digestion approach that took about 6 hours. The action mechanism involved in the observed rate acceleration of the enzymatic cleavage of proteins under microwave irradiation was studied at different microwave temperatures at different irradiation time intervals. The results suggest that the rapid increase in the reaction temperature is at least partially responsible for the large acceleration of digestion observed under microwave conditions [106]. This strategy using microwave irradiation for protein digestion has significant implications in proteomics research in which protein digestion is often a tedious step in protein identification. For those tightly folded proteins, they are known to require long hours for adequate proteolysis by enzymes under conventional conditions. Clearly, this approach can dramatically enhance proteolysis rates under microwave irradiation, improve the efficiency of protein digestion, thus protein identification. These noncovalent interactions may involve enzyme and substrate, protein and ligand, protein and protein, and antigen and antibody [107, 108]. In a drug discovery process, it is desirable to have a good understanding of potential drug candidates that have affinities toward a particular target protein. A sample containing potential drug ligands is continuously infused through the column. The order of elution of ligands from the column parallels their affinities for the target protein, with the tightest binding ligands eluting last. This reagent contains a sulfo-N-hydroxy-succinimide that reacts with amines to form a stable amide bond and is soluble in aqueous solvents. This technique offers resolution of multiple binders and the rank order for a wide range of binding affinities and class-specific structural trends. In this approach, drug ligands and target protein are incubated under native conditions. Active compounds will form tightly bound noncovalent complexes with the target protein. The complexes will then be separated from the unbound (inactive) molecules by size-exclusion chromatography. The column was equilibrated with 100-L 25 mM ammonium bicarbonate (pH 8) for 1 minute at 3000 rpm. About 100-L aliquot of the incubation mixture was loaded onto the column and centrifuged. A nonbinding compound elutes first as the void marker because it shows no affinity to the target. This technique is relatively simple, as compared to immobilized protein affinity column, and it provides greater indication of binding under native conditions with considerable sensitivity (picomole range). In addition, the analysis of small molecule ligands is more straightforward than analyzing the protein/drug ligand complex.
© 2025 Adrive Pharma, All Rights Reserved..