General Information about Depakote
What conditions does Depakote treat?
It is essential to follow the prescribed dosage and never miss any doses. Suddenly stopping Depakote or altering the dosage with out consulting a doctor can enhance the chance of seizures and other serious unwanted aspect effects.
More severe unwanted side effects which will happen embrace liver injury, which can be monitored via regular blood exams, and pancreatitis, a doubtlessly life-threatening condition. It is important to seek immediate medical consideration if symptoms corresponding to stomach ache, lack of appetite, jaundice, or dark urine happen while taking Depakote.
Depakote could interact with different medications, together with birth control tablets, antidepressants, and blood thinners. It is crucial to inform a doctor about any drugs, dietary supplements, or herbal merchandise being taken to keep away from potential interactions and surprising unwanted effects. Depakote may also increase the danger of birth defects if taken during being pregnant, so it's essential for girls of childbearing age to make use of efficient contraception while taking the medication.
What is Depakote?
Depakote is primarily used to deal with numerous forms of seizures, including generalized seizures, absence seizures, and partial seizures. It can also be used to stop migraine complications and deal with bipolar dysfunction. In some cases, Depakote may be prescribed off-label for circumstances such as borderline personality dysfunction, post-traumatic stress disorder (PTSD), and impulse control issues.
Like another medicine, Depakote could trigger unwanted effects, though not everybody experiences them. Some of the widespread unwanted side effects include nausea, vomiting, diarrhea, dizziness, and drowsiness. These unwanted aspect effects are normally gentle and may go away because the body adjusts to the medication. If these side effects persist or turn out to be bothersome, it could be very important consult a doctor.
Depakote is available in a number of types, together with delayed-release tablets, extended-release tablets, sprinkle capsules, and oral syrup. The different varieties enable for flexibility in dosing and make it easier for patients to take the medicine as prescribed.
What are the potential side effects of Depakote?
Depakote, also referred to as divalproex sodium, has been a trusted medication for treating seizures for over 30 years. It is an anticonvulsant drug that's used to regulate numerous kinds of seizures, together with epileptic seizures, absence seizures, and even certain types of psychiatric disorders. Let's take a closer look at what Depakote is and the method it works.
Depakote is a prescription medicine that was permitted by the united states Food and Drug Administration (FDA) in 1983. The energetic ingredient in Depakote, divalproex sodium, is a compound that converts to valproic acid within the body. Valproic acid will increase the degrees of gamma-aminobutyric acid (GABA) in the mind, which is a neurotransmitter that helps to calm and stabilize nerve activity. By increasing GABA levels, Depakote helps to regulate seizures and prevent them from occurring.
The dosage of Depakote varies depending on the individual's age, weight, and medical situation. It is normally taken two to three times a day, with or without food, as directed by a doctor. The delayed-release and extended-release tablets must be swallowed whole and not crushed or chewed. The sprinkle capsules may be opened and the contents sprinkled on meals, making it simpler for kids or those who have issue swallowing tablets to take the treatment.
Are there any precautions to consider when taking Depakote?
How is Depakote taken?
In conclusion, Depakote is a well-established treatment for treating seizures and different circumstances. It has been effective in controlling seizures and enhancing the quality of life for many sufferers. However, it is essential to comply with the prescribed dosage and monitor any potential unwanted effects carefully. If you or a liked one is taking Depakote, be sure to talk about any considerations or questions with the prescribing doctor to make sure the safest and best treatment.
Catheters in these large vessels are often undesirable in head and neck surgery due to their intrusion into the surgical field symptoms joint pain fatigue generic depakote 250 mg fast delivery. Femoral vein catheters offer the benefit of being far from the surgical field and also serve as a reliable central access in cases of surgical bleeding originating from the vessels of the neck. For hemodynamic monitoring, blood pressure measurements every 3 minutes with a sphygmomanometer are usually adequate for most cases. Based on the principle of arterial wall unloading, this monitor uses two finger cuff sensors wrapped around the index and middle finger to obtain a blood pressure signal that is calibrated using a special transfer function. After processing, the monitor provides a real-time continuous display of systolic, mean, and diastolic blood pressure, left ventricular stroke volume, and cardiac output and pulse pressure variability. For patients with uncontrolled hypertension, congestive heart failure, or ischemic heart disease, invasive monitoring of the arterial pressure by an indwelling arterial catheter is beneficial. Blood samples for determination of arterial blood gases, hemogram, and other blood chemistries can be taken from the arterial line. Complications from arterial cannulation such as ischemia and infections are fortunately rare. Central venous pressure monitoring is useful to optimize blood volume status in patients with a history of congestive heart failure. Similarly, monitoring of pulmonary artery pressure and cardiac output with a pulmonary artery catheter is occasionally required for critically ill patients. As an alternative to these invasive procedures, beat-to-beat left ventricular output and stroke volume can be measured much less invasively by arterial line tracing contour analysis. Complex computer algorithms serve to calculate the area under the systolic portion of the arterial pulse waveform. This technique has been shown to be accurate and reliable when compared to cardiac output measurements by a pulmonary artery catheter. This noninvasive technique is also useful in predicting the hemodynamic response to intravenous fluid administration. Cyclical fluctuations of the arterial blood pressure tracing related to the expiratory and inspiratory phases of the respiratory cycle have been used to detect hypovolemia when the difference is >10 mm Hg. Because low blood volume decreases right ventricular preload, increases right ventricular afterload, and decreases left ventricular afterload, a marked variability in stroke volume can be used as a predictor of responsiveness to fluid administration in low cardiac output states. Because the accuracy of this technique depends on the quality of the arterial waveforms, this technique is not reliable in the presence of frequent atrial or ventricular arrhythmias, especially atrial fibrillation. Intraoperative transesophageal echocardiography examinations routinely performed by cardiovascular anesthesiologists are seldom needed for head and neck surgery, except for very rare cases of cardiogenic shock. This primitive and imprecise scheme often led to anesthetic overdose and terrifying intraoperative patient awareness and recall. For this reason, this monitor is not as commonly used in head and neck surgery compared to other surgical specialties. Typically, this is needed in cases presenting with high risk for intraoperative strokes such as complex surgical resection involving the carotid arteries or in patients with known critical carotid stenosis. The desired position may impose potentially harmful anatomical and physiologic changes to the patient. The anesthetized and paralyzed patient may be subjected to exaggerated postures, which they would not be able to tolerate if they were awake. All pressure points and prominent bony parts, especially elbows and heels, should be free from direct contact with the cold steel operating table. These vulnerable areas should be protected by careful padding with foam pads to prevent peripheral nerve injuries. In large patients, a well-padded arm protector toboggan can be placed to protect the arms from being leaned upon by surgical assistants. The operating room table is often turned 90 or 180 degrees from the anesthetic machine to allow free access around the head and neck not only for the attending surgeon, but for all the surgical assistants. The patient is usually positioned in the supine position with the back of the table elevated 30 degrees to improve surgical access. Elevation of the head and thorax shifts abdominal contents away from the diaphragm, decreases atelectasis of the lower lobes of the lungs, and improves functional residual capacity. It also facilitates venous drainage away from the operative site, resulting in a less bloody operative field and decreased tissue edema. Side effects include decreased cerebral perfusion, risk of air embolism, and concealed blood loss trickling down unnoticed under the surgical drapes. When neck extension is needed to improve surgical access, mechanical compression of the carotid sinus located at the bifurcation of the common carotid artery may lead to the carotid sinus reflex. In patients with carotid sinus hypersensitivity, this reflex is greatly exaggerated and can be triggered by simple extension of the neck without direct manual compression of the carotid sinus. It can be used either to cut or to vaporize the lesion depending on the laser settings. It is especially useful in resecting bulky tumors of the epiglottis and vocal cords. Surgical lasers have the potential for inadvertent tissue damage and for causing fires. The eyes of the patient must be protected with moist eye pads or special laser eye covers. To prevent sudden patient movement and inadvertent impact of the beam, muscle relaxation is usually required to help ensure an immobile surgical field. Instruments with a polished surface can reflect laser beams to an unintended destination and thus cause injury, especially to eyes of operating room personnel. A smoke evacuator system with a high-efficiency particulate air filter should be positioned at the surgical site.
Measuring the quality of care for patients with cancer serves a number of important functions symptoms for diabetes order cheapest depakote. Stakeholders, including patients, payers, and physicians, use the results to make informed decisions regarding treatment. Patients may decide among care centers or hospitals depending upon available quality measures or "grades. For example, patients with cancer of the head and neck with advanced cancer (T) stage or metastatic lymph nodes should be referred to radiation oncology for consideration of postoperative radiation therapy. Understanding levels of adherence to these guidelines and working to improve compliance should serve to improve patient care overall. For example, routine preoperative imaging with a specific imaging modality may or may not affect treatment or improve outcome. Assessing the specific value of a preoperative imaging tool allows for decisions to be made at a system-wide level for such studies. Establishing metrics that define quality care enables changes in the quality improvement process. Development of Quality Metrics the establishment of quality measures typically evolves from the consensus of an expert multidisciplinary panel convened to review the literature and provide commentary; strong expert consensus is essential. A thorough and comprehensive review of the literature is performed to identify the available evidence regarding a particular process of care. This evidence is vetted to determine the level of evidence of the available clinical research (Table 7. The best process measure comes from research that a specific practice results in improved outcome(s). For example, patients treated surgically for squamous cell carcinoma of the head and neck with extracapsular extension of cancer detected in their cervical lymph nodes have improved locoregional control from the administration of postoperative adjuvant chemoradiotherapy rather than radiation therapy alone. Once a quality measure is accepted, performance of physicians and/or institutions can be evaluated by adherence to this measure. Clinical status relates to the biologic outcome of the disease, such as 5-year survival after cancer diagnosis. Other clinical outcomes include postoperative events, such as 7-day return to operating room, 30-day readmission rate, postoperative wound infections, or 30-day mortality rates. The assessment of functional status includes disease effects on the patient in the physical, emotional, and cognitive domains. Karnofsky performance status is a well-validated measure of patient functional status that also correlates with quality of life and predicts survival. Although patients who are more satisfied are more likely to complete and follow through with treatment regimens, no correlation exists between patient satisfaction and the quality of the care process. Finally, a robust outcomes measure must account for factors that are not directly influenced by the health system. These variables include age, socioeconomic status, insurance status, race, cultural beliefs, and comorbidities. While measuring outcomes may seem most relevant to patient care, assessing quality of care requires outcome measures that can be directly attributed to a specific process of care. Administrative records can be examined, although they typically lack sufficient clinical detail; tumor staging is typically not part of the diagnosis code for insurance records. Medical records may be filled with clinical detail, but systematic reviews are labor intensive and not feasible at a national scale to evaluate patterns of care. Cancer registries were established by the National Cancer Act and may include information regarding tumor stage, first course of treatment, and overall survival. However, the level of detail can be quite variable and thus be inadequate as a data source to monitor cancer care quality. For example, although a cancer registry may capture pathologic assessment, postoperative chemotherapy and/or radiation therapy details may be lacking. Furthermore, the actual completion of recommended therapy is typically not present. The various limitations of these data sources clearly signal the need for a better reporting system. These guidelines enable individual physicians to deliver optimal evidence-based care for their patients. Adherence to some or all of these guidelines serves as the basis for measuring quality of care. These guidelines serve to standardize care and decrease variation in care that can lead to poor quality of care. These guidelines are not in themselves quality performance measures and were not formulated for that purpose. Currently, available treatment guidelines cover general issues of otolaryngology such as cerumen impaction and acute sinusitis. There are general performance measures that may be applied to care of patients with cancer of the head and neck. For example, there are metrics for systematic and complete pathology reporting that include tumor staging and histologic grade. The mission of this committee was to formulate evidence-based quality of care measures for patients with cancer of the head and neck. The committee was also charged to promote compliance with these standards as a framework to measure quality of care in head and neck surgery. A multidisciplinary committee was formed and began to develop quality measures in 2006. Working groups focused on metrics related to pretreatment, treatment, and posttreatment care.
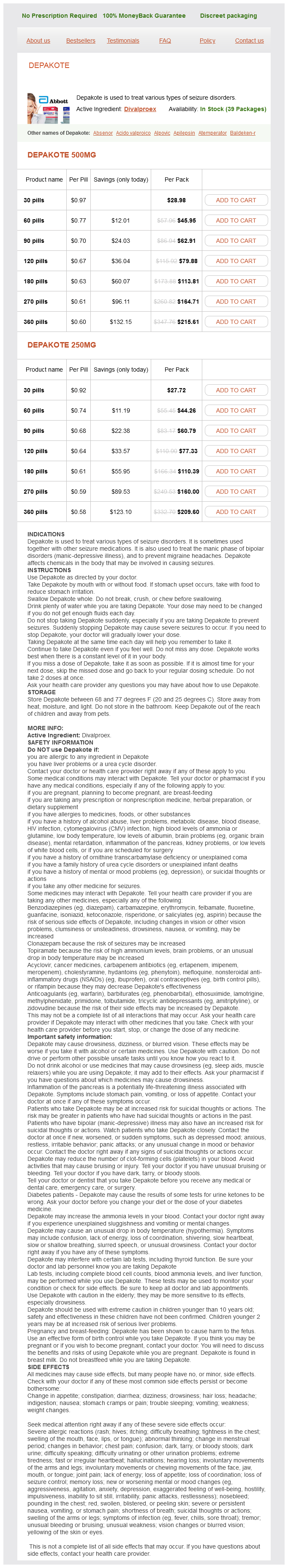
Depakote Dosage and Price
Depakote 500mg
- 30 pills - $28.98
- 60 pills - $45.95
- 90 pills - $62.91
- 120 pills - $79.88
- 180 pills - $113.81
- 270 pills - $164.71
- 360 pills - $215.61
Depakote 250mg
- 30 pills - $27.72
- 60 pills - $44.26
- 90 pills - $60.79
- 120 pills - $77.33
- 180 pills - $110.39
- 270 pills - $160.00
- 360 pills - $209.60
Anteroinferiorly medicine abuse order depakote 500 mg, the lacrimal sac is situated between the anterior and posterior lacrimal crests at the junction between the medial wall and the floor. The lacrimal part of the orbicularis oculi arises from the posterior lacrimal crest. At the junction of the medial wall and the roof, the frontoethmoidal suture presents the anterior and posterior ethmoidal foramina, the former transmitting the nasociliary nerve and anterior ethmoidal vessels and the latter the posterior ethmoidal nerve and vessels. The lateral wall is formed by the orbital process of the zygomatic and the orbital surface of the greater wing of the sphenoid. On the orbital process of the zygomatic bone are the orbital tubercle (Whitnall) and the orifices of one or two canals, which transmit the branches of the zygomatic nerve. Through this fissure, the oculomotor, the trochlear, the ophthalmic division of the trigeminal (V1), and the abducens nerves enter the orbital cavity, also some filaments from the cavernous plexus of the sympathetic and the orbital branches of the middle meningeal artery. Passing posteriorly through the fissure are the ophthalmic vein and the recurrent branch from the lacrimal artery to the dura mater. The lateral wall and the floor are separated posteriorly by the inferior orbital fissure, which transmits the maxillary nerve (V2) and its zygomatic branch, the infraorbital vessels, and the ascending branches from the sphenopalatine ganglion. The base of the orbit (orbital rim), quadrilateral in shape, is formed superiorly by the supraorbital arch of the frontal bone, in which is the supraorbital notch or foramen for the passage of the supraorbital vessels and nerve; inferiorly by the zygomatic bone and maxilla, united by the zygomaticomaxillary suture; laterally by the zygomatic bone and the zygomatic process of the frontal joined by the zygomaticofrontal suture; and medially by the frontal bone and the frontal process of the maxilla united by the frontomaxillary suture. The optic foramen is a short, cylindrical canal, through which passes the optic nerve and ophthalmic artery. The extraocular muscles-four rectus muscles and two obliques-effect movement of the eye. The third cranial nerve innervates all but the lateral rectus and the superior oblique muscles, which are innervated by the fourth and sixth cranial nerves, respectively. The rectus muscles originate at the annulus of Zinn and insert on the globe forming a muscle cone, which is the central anatomic space in the orbit. Secretory glands-the glands of Moll, Krause, and Wolfring-may be found along the margin of the eyelid. The lacrimal drainage system, located in the inferonasal orbit, is represented by the puncta, canaliculi, lacrimal sac, and nasolacrimal duct. Each of these epithelial surfaces represents a potential site of origin for cancer. In the same study, random biopsy of the middle turbinate showed evidence of dysplasia in 21% of workers. All workers had been employed for at least 10 years, and there was an average latent period of 18 to 36 years before the development of carcinoma, most of which were squamous cell or anaplastic. The molecular mechanisms responsible for metal translocation in olfactory neurons and deposition in the olfactory bulb are unclear, but chelation by metal-binding molecules such as carnosine (beta-alanyl-L-histidine) may be involved. A meta-analysis of 12 large case control studies estimated that male wood workers had a summary odds ratio of sinonasal cancer of 2. This is uniquely different from the mucosa of the rest of the upper respiratory tract, which is derived from endoderm. Upward extension of these neoplasms toward the cribriform plate or fovea ethmoidalis is not uncommon and heralds intracranial extension. As most sinonasal cancers are relatively asymptomatic when small, it is often the manifestation of local spread that prompts patients to seek medical attention. In the maxillary sinus, direct extension may occur anteriorly into the soft tissues of the cheek, superiorly into the orbit with resultant proptosis and diplopia, inferiorly into the oral cavity, or posteriorly into the pterygomaxillary space where it may spread along the branches of the maxillary division of the trigeminal nerve (V2). Cancer of the frontal sinus is quite rare, but the most significant direct extension is posteriorly to the frontal lobes. Cancer of the ethmoid sinus often presents with medial extension to the orbit, superior extension to the cribriform plate, and posterior extension into the sphenoid sinus and nasopharynx. In addition to direct local extension, cancer of the paranasal sinuses can spread to nearby structures via the many fissures and foramina located in this region. From the frontal sinus, cancer may extend into the nasal cavity through the nasofrontal duct. Perineural Spread the dissemination of cancer cells along nerves is a frequent pathologic finding among a variety of cancers, including head and neck, upper gastrointestinal, pancreatic, and prostate carcinomas. Tumors that have a considerable propensity to disseminate along nerves are known as neurotropic cancers. Alternatively, they may spread in an antegrade fashion and along the involved nerve and its terminal branches. In either case, this neural spread makes surgical resection more complicated and achieving negative surgical margins less certain. Intraneural invasion was found in 32% of these cases, and 34% invaded more than 1 cm distal to the tumor. Regional Metastases the lymphatic drainage of the posterior nasal cavities and paranasal sinuses is primarily to the retropharyngeal and lateral pharyngeal nodes at the base of the skull and then to the upper jugular lymph nodes. Cancer of the anterior nasal cavity and those that erode through the maxilla into the soft tissues of the face spread to the submandibular and upper jugular lymph nodes. Regional metastases from paranasal sinus cancer are relatively uncommon and have been characterized to a greater extent for maxillary sinus cancer than for other paranasal sites. The risk of developing regional metastasis after treatment correlates with local tumor recurrence. The role of elective neck dissection or radiation has yet to be defined in patients with cancer of the maxillary sinus. Distant Metastases Although distant metastasis from cancer of the paranasal sinus does occur, failure to control the disease secondary to local recurrence is far more common. Cancer of the ethmoid has a similar rate of distant metastasis, with adenocarcinoma having a slightly higher rate than squamous cell cancer (15% to 20% vs. There is a different staging system for tumors of the maxillary sinus from that used for ethmoid sinus and nasal cavity tumors. The nodal staging system for maxillary, ethmoid, and nasal cavity tumors is the same as for other sites in the head and neck and depends on the number, size, and laterality of involved lymph nodes.
© 2025 Adrive Pharma, All Rights Reserved..